The observation of a feeding by a professional is important to strengthen breastfeeding. The Bristol Breastfeeding Assessment Tool (BBAT) was translated into Spanish and validated.
Material and methodsTranslation and back-translation of the original scale was done. Six pediatricians and six pediatric nurses collaborated. At the newborn's first visit, a feeding was observed and the pediatrician and nurse scored the BBAT scale independently. The nurse also scored the LATCH Breastfeeding Assessment (LATCH) and each mother filled out the Breastfeeding Self-Efficacy Scale (BSES-SF). Mothers were appointed a week later and the nurse re-scored the BBAT.
ResultsA total of 62 mothers participated. There was good internal consisitency for the BBAT (Cronbach's alpha = 0.83 in the assessment made by the nurses and Cronbach's alpha = 0.79 in the assessment made by the pediatricians). Inter-rater consistency showed an intra-class correlation coefficient of 0.91, while for the test-retest was 0.67. Concurrent validity with the BSES-SF scale was good and with the LATCH scale very good. The factor analysis showed the one-dimensional character of the scale and a good homogeneity of the 4 items (positioning = 0.771, attachment = 0.852, sucking = 0.856 and swallowing = 0.679).
ConclusionsThe scale obtained in Spanish shows good reliability and validity. The BBAT is an easy-to-use tool that allows breastfeeding assessment and determines the aspects that need to be improved.
La observación de una toma por parte de algún profesional es importante para afianzar la lactancia materna. Se tradujo al español y se validó la escala de observación de una toma Bristol Breastfeeding Assessment Tool (BBAT).
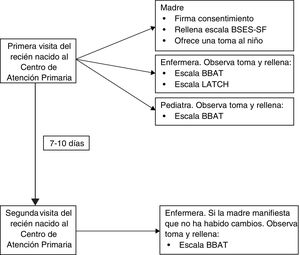
Material y métodosSe hizo traducción y retrotraducción de la escala original. Colaboraron 6 pediatras y 6 enfermeras de pediatría. En la primera visita del recién nacido se observó una toma y el pediatra y la enfermera puntuaron la escala BBAT de manera independiente. La enfermera también puntuó la escala de observación de una toma LATCH Breastfeeding Assessment (LATCH) y cada madre rellenó la escala de autoeficacia para la lactancia Breastfeeding Self-Efficacy Scale (BSES-SF). Las madres fueron citadas una semana después volviendo a puntuar la BBAT la enfermera.
ResultadosParticiparon 62 madres. La BBAT presenta una buena consistencia interna (alfa de Cronbach = 0,83 en la valoración hecha por las enfermeras y alfa de Cronbach = 0,79 en la valoración hecha por las pediatras). La fiabilidad interjueces muestra un coeficiente de correlación intraclase de 0,91, mientras que para el test-retest fue de 0,67. La validez concomitante con la escala BSES-SF fue buena y con la escala LATCH muy buena. El análisis factorial mostró el carácter unidimensional de la escala y una buena homogeneidad de los 4 ítems (posición = 0,771, agarre = 0,852, succión = 0,856 y deglución = 0,679).
ConclusionesLa traducción obtenida presenta una buena fiabilidad y validez. La BBAT es una herramienta fácil de utilizar que permite valorar una toma y determinar los aspectos que se tienen que mejorar.
Breastfeeding (BF) should be the only source of nutrition for infants in the first 6 months of life.1 However, based on the latest National Health Survey of Spain, only 39% of mothers in the country maintain exclusive BF through 6 months post birth.2 Health care professionals have an important responsibility in supporting mothers that wish to pursue this infant feeding modality.3
In this regard, the identification of mothers at risk of discontinuing BF, especially in the first days post birth, is essential.3 Several scales are available for this purpose, designed to detect the presence of problems in order to predict which mothers are at risk of discontinuing BF and be offer greater support as needed.4,5 Clearly, scales that assess modifiable aspects of BF are most pertinent, as they allow professionals to address the element identified as possibly interfering with BF.6 In addition, the use of scales allows a uniform approach in data collection and an easier exchange of information between clinicians.7
Some scales are based on the presence of variables that have been identified as risk factors for discontinuation, such as maternal age or a previous history of breast surgery.8 But these elements cannot be modified, so the usefulness of these scales is relative.
Other scales assess the self-efficacy of mothers to breastfeed (modifiable element)9 and are based on self-reporting by the mother. The most widely used is the Breastfeeding Self-Efficacy Scale, of which the short form version (BSES-SF) has been translated to Spanish and subsequently validated.10
However, most scales are based on the observation of a BF session by a health care professional. These scales have the advantage that they can be used to identify problems in BF technique, allowing its correction by professionals. In the hospital, a full BF session should be observed at least once in the immediate postpartum period. In addition, when mothers first visit the primary care centre (PCC), it would be useful for a health care professional to repeat this observation.3 There are multiple scales of this kind. Some of the best known ones are the Bristol Breastfeeding Assessment Tool (BBAT),11 the Infant Breastfeeding Assessment Tool (IBFAT),12 the Mother-Baby Assessment (MBA)13 or the LATCH breastfeeding assessment tool.14 The LATCH is the only tool for which a validation study of its adaptation to Spanish has been published.15
Thus, there are hardly any breastfeeding observation scales adapted to Spanish. We conducted a study to adapt and validate the BBAT.
Material and methodsStudy settingThe study was conducted in 3 PCCs, 1 in the Barcelona metropolitan area and 2 in the Chartered Community of Navarre. Between the 3 centres, a total of 6 paediatricians and 6 paediatric nurses participated in the study.
Study periodThe data collection took place between July 1, 2019 and December 31, 2020.
Study sampleWe consecutively recruited mothers that brought their newborns to the PPC for their initial visit until we completed the necessary sample size.
The inclusion criteria were: maternal age more than 18 years, term delivery (at 37 or more weeks of gestation), exclusive breastfeeding at the time of the initial visit to the PCC. This initial visit had to take place within 15 days post birth. To be included in the study, the mothers had to sign an informed consent form.
The exclusion criteria were: maternal language barrier, twin birth, presence of congenital anomalies that could interfere with feeding (neuropathy or craniofacial malformations).
Study variablesPrimary outcome:
- •
Score in the BBAT, which can range from 0 to 8 points.
Secondary outcomes:
- •
Score in the BSES-SF (possible score, 14–70 points) and score in the LATCH scale obtained through observation of a BF session (possible score, 0–10 points).
- •
Maternal characteristics: age, origin, educational attainment, tobacco use, single-parent family, number of previous children, previous history of BF, attendance to childbirth education classes, contact with BF support groups
- •
Pregnancy and childbirth characteristics: prenatal care, duration of gestation, type of delivery, hospital where birth took place.
- •
Infant characteristics: days of stay of newborn (NB) in maternity ward, days from birth to initial checkup, sex, 1-min and 5-min Apgar scores, birth weight, weight in initial checkup, weight in follow-up visit.
The BBAT consists of 4 items that assess the 4 key components of a feeding: positioning, attachment, sucking and milk transfer. Each item includes a note specifying the aspects to observe for each of these components. Each item is rated as follows: poor (0 points), moderate (1 point) or good (2 points), so that the possible total score ranges from 0 to 8 points.
Translation and adaptation of the BBATWe started by asking the author of the original scale for permission to carry out the adaptation. Three of the authors made initial translations to Spanish independently. Then, these translations were evaluated and an initial version of the Spanish BBAT drafted by consensus. This initial draft was back translated to English by a bilingual individual that was not acquainted with the original text of the scale. This back translation was reviewed by the authors of the study and by the author of the original scale, followed by the establishment of the definitive version of the translation to Spanish by consensus (Table 1). Lastly, a pilot test was conducted through the observation of a feeding session by 5 professionals to verify the correct comprehension of the text.
Bristol Breastfeeding Assessment Tool.
| Malo | Intermedio | Bueno | |
|---|---|---|---|
| POSICIÓNBebé bien apoyado; pegado contra el cuerpo de la madre, tumbado de lado/cuello no torcido, nariz dirigida hacia el pezón, madre segura sosteniendo al bebé. | Ninguno o pocos elementos logradosNecesita explicación sobre la posición | Logra algunos de los elementosNecesita algún consejo sobre la posición | Logra todos los elementosNo necesita consejo sobre la posición |
| AGARREAgarre positivo, boca bien abierta, el bebé logra un agarre rápido con una buena cantidad de areola dentro de la boca, el bebé permanece con un buen agarre durante toda la toma | El bebé es incapaz de agarrarse al pecho o consigue un agarre deficiente.Ningún/pocos elementos logrados.Necesita explicación sobre el agarre | Logra algunos de los elementosNecesita algún consejo sobre el agarre | Logra todos los elementosNo necesita ningún consejo sobre el agarre |
| SUCCIÓNCapaz de establecer un patrón de succión eficaz en ambos pechos (succiones rápidas al inicio y luego succiones más lentas con pausas). El bebé finaliza la toma. | Succión no efectiva; no patrón de succión | Alguna succión efectiva; patrón de succión no satisfactorio; coge y suelta el pecho | Logra un patrón eficaz de succión |
| DEGLUCIÓNAudible, regular y suave, sin chasquidos. | No se oye deglutir; chasquidos | Sonido de deglución ocasional; alguna deglución ruidosa o chasquidos | Deglución audible, regular y tranquila |
BBAT: Bristol Breastfeeding Assessment Tool.
On the day that the mothers visited the PCC, informed consent was obtained before proceeding to collect the data. The mothers completed the BSES-SF followed by observation of a BF session. The initial observation was carried out by a nurse and a paediatrician, each of who completed the BBAT independently. We analysed the resulting scores to assess inter-rater reliability (nurse-paediatrician). In this initial observation, the nurse also completed the LATCH score.
After the initial visit, an appointment was scheduled to weigh the newborn in 7–10 days. If the mother reported that there had not been significant changes in BF since the initial visit, another BF session was observed by the same nurse that had rated the observation in the first visit. We used this second observation to assess intra-rater (test-retest) reliability (Fig. 1).
Sample size calculationWe took as reference the correlation found between the BBAT and the BSES-SF in the original study by Ingram et al., which was 0.57.11 However, we chose to maximise the sample size to be able to detect a much weaker correlation and guarantee statistical power. Therefore, we made the calculations to be able to detect a correlation of 0.35, which yielded a necessary sample size of 62 patients for an α level of 0.05 and a β level of 0.20.
Statistical analysisWe conducted a descriptive analysis of the characteristics of the sample under study.
In the analysis of reliability, we assessed internal consistency by means of the Cronbach α, and defined a satisfactory reliability as a value of 0.7 or greater. We also assessed interrater reliability by means of the intraclass correlation coefficient (ICC) for the scores obtained by the nurse and the paediatrician in the initial visit. We assessed the stability of scale in the scores obtained by the nurse in patients included in the test-retest reliability analysis calculating the ICC for these two measurements. We used the Pearson correlation coefficient to assess the association between the BBAT score obtained in the first visit and the scores in the BSES-SF and LATCH assessment tool.
To assess the structural validity of the scale, we conducted a principal component analysis and considered that a given item was important in calculating the component if it had a loading greater than 0.30.
Ethical considerationsWe sought the consent of the mothers to participation in the study after informing them about it. We handed each mother a printout with information about the study and asked them to sign an informed consent form.
We safeguarded the confidentiality and anonymity of the data in adherence with current law in our region (Regulation EU 2016/679 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data of the European Parliament and of the Council).
The study was approved by the Clinical Research Ethics Committee of the Institut Universitari d’Investigació en Atenció Primària Jordi Gol (IDIAPJGol) as file 19/072-P.
ResultsBoth the forward and back translation of the BBAT were agile processes with a high level of agreement between the involved parties. No noteworthy conflicts emerged in the development of the final version in Spanish.
The sample recruited to validate the translation included 62 mothers and their newborn infants. Table 2 presents the main characteristics of the mothers, the pregnancy, the delivery and the infants.
Characteristics of the sample.
| Maternal characteristics | ||
|---|---|---|
| Age | 31.7 (5.7) | |
| Mean (standard deviation) | ||
| Origin n (%) | Spain | 24 (38.7) |
| Latin America | 23 (37.1) | |
| Maghreb | 10 (16.1) | |
| Other | 5 (8.1) | |
| Maternal educational attainment n (%) | No education | 1 (1.6) |
| Primary | 11 (17.7) | |
| Secondary | 34 (54.8) | |
| Higher | 16(25.8) | |
| Smoking mother n (%) | 4 (6.5) | |
| Single-parent family n (%) | 3 (4.8) | |
| Number of previous children | 0 (0−4) | |
| Median (minimum-maximum) | ||
| Breastfed before n (%) | 25 (40.3) | |
| Attended childbirth education classes n (%) | 32 (51.2) | |
| Has contacted a breastfeeding support group n (%) | 6 (9.7) | |
| Pregnancy and birth characteristics | ||
|---|---|---|
| Prenatal care n (%) | 62 (100.0) | |
| Gestational age | 40 (37−42) | |
| Median (minimum-maximum) | ||
| Type of delivery n (%) | Spontaneous vaginal | 46 (74.2) |
| Instrumental vaginal | 6 (9.7) | |
| Urgent caesarean | 5 (8.1) | |
| Planned caesarean | 5 (8.1) | |
| Hospital of delivery n (%) | Public | 60 (96.8) |
| Private | 2 (3.2) | |
| 1-min Apgar | 9 (7−10) | |
| Median (minimum-maximum) | ||
| 5-min Apgar | 10 (9−10) | |
| Median (minimum-maximum) | ||
| Infant characteristics | ||
|---|---|---|
| Sex n (%) | Niño | 34 (54.8) |
| Niña | 28 (45.2) | |
| Birth weight (g) | 3352 (384) | |
| Mean (standard deviation) | ||
| Days of life at first medical visit | 8.3 (3.1) | |
| Mean (standard deviation) | ||
The analysis of reliability revealed a good internal consistency, with a balanced contribution of each of the items to the score (Table 3). The correlation between each item score and the total score was high overall. The values were somewhat lower in the assessments made by paediatricians. The squared multiple correlation values were also similar for every item, reflecting a good internal consistency. The Cronbach Α for the total scale for the BF assessments made by nurses was 0.83 (0.75−0.89), compared to 0.79 (0.68−0.86) for the assessments made by paediatricians. There was no case in which removal of any single item of the scale led to a higher Cronbach α for the total score, which indicated that none of the items could be considered superfluous (Table 3).
Analysis of the internal consistency of the BBAT.
| Mean score if item is deleted | Corrected item-scale correlation | Squared multiple correlation | Cronbach α if item is deleted | |
|---|---|---|---|---|
| Assessment by nurse | ||||
| Positioning | 5.21 | 0.62 | 0.45 | 0.82 |
| Attachment | 5.08 | 0.73 | 0.55 | 0.75 |
| Sucking | 4.82 | 0.71 | 0.59 | 0.78 |
| Swallowing | 4.87 | 0.64 | 0.56 | 0.80 |
| Assessment by paediatrician | ||||
| Positioning | 5.24 | 0.60 | 0.45 | 0.74 |
| Attachment | 5.10 | 0.67 | 0.50 | 0.69 |
| Sucking | 4.89 | 0.57 | 0.42 | 0.75 |
| Swallowing | 4.90 | 0.57 | 0.43 | 0.74 |
BBAT, Bristol Breastfeeding Assessment Tool.
The degree of agreement between the scores given by nurses and paediatricians, respectively, was excellent, with an ICC of 0.91 (0.85−0.95).
In the test-retest reliability assessment, we included the data for the 36 mothers that reported that there had not been any significant changes in BF between the first and second visits. The mean time elapsed between the 2 visits was 8.3 days (standard deviation, 2.4). The ICC in the comparison of the scores obtained in the first and second visits was 0.67 (0.33−0.84).
When it came to the assessment of concurrent validity, the Pearson correlation coefficient in the comparison with other instruments was 0.81 (P < .001) for the LATCH assessment tool applied by the nurses and 0.55 (P < .001) for the BSES-SF completed by the mothers.
The assessment of the internal structure by principal component analysis is presented in Table 4. All items had high and similar loadings in component 1, which corroborated the unidimensional nature of the scale. The percentage of the total variance explained by the one-component solution was 68.27%. The analysis of the communality led to the same conclusion, as all values were close to the total variance explained.
DiscussionAs previously noted, there is a broad range of scales designed to assess BF through the observation of a feeding session.7 Selecting just one for translation and validation posed challenges for us. The LATCH assessment tool is probably the most widely used and the only one translated to Spanish and subjected to an assessment of reliability, although the translated Spanish version has not yet been validated.15 It is an easy to use scale and it has been analysed in many studies, especially in the hospital setting.4,5,14,16–18 It also appears to offer an acceptable predictive validity for BF.4,16–19 However, this scale assesses different dimensions of BF. It is used to assess the feeding session in terms of infant attachment, audible swallowing and the need of assistance to keep the infant positioned at the breast, elements that can improve with intervention. But it also assesses other dimensions, such as nipple shape (an aspect that would be difficult to modify)15 and sore or cracked nipples (which are usually due to poor BF technique).20 It would have been simpler for us to validate a scale that was already translated to Spanish, such as the LATCH score, but we decided that validating a scale that strictly assesses BF technique, which can be easily modified, would be of greater interest.
There is no other scale for rating a BF observation translated to Spanish. In addition, the studies comparing the different scales developed to date have not produced solid evidence of the psychometric validity of any of them. Therefore, these scales should be applied with caution.3,21–24 Notwithstanding, of all the scales currently available, the BBAT is among those that offer a higher validity backed by evidence.25 In addition, this scale assesses the feeding itself and indirectly provides information to health professionals on the aspects of it that need to improve. This is why this was the scale ultimately selected for adaptation.
The BBAT was created in 2015 by Ingram et al. and its one of the most recently developed scales.11 It has been validated for use in healthy term newborns and, to date, has exhibited good psychometric properties.11,26 The BBAT is simple and easy to use, and requires no training of the individual that applies it.25 The Cronbach α obtained in our study (0.83 for nurses and 0.79 for paediatricians) was higher compared to the original development study (0.69)11 and the validation study conducted in Turkey (0.77),26 and we found that the internal consistency of the translated and adapted version was very good. The correlation to the BSES-SF (0.55) was similar to the correlation found in the original study (0.57).11 The correlation to the LATCH score (0.81) was higher compared to the study by Dolgun et al. (0.76).26 Only the ICC of 0.67 in the test-retest reliability analysis was lower compared to the study by Dolgun et al. (0.89),26 although the authors of the study in Turkey did not specify the time elapsed between the test and the retest, making this a qualified comparison (the time elapsed in our study was 8 days). The fact that BF is a dynamic situation probably contributed to this result, as it is unlikely that the exact same characteristics will hold through time.
Thus, the results obtained with the translated version were similar or superior to those reported in previous studies. In addition, the high level of agreement between the scores obtained by nurses and paediatricians suggests that this tool could be used by either of these professionals interchangeably.
A very important aspect would be for data on BF to be conveyed from maternity wards to PCCs. This information seldom reaches the PCC and when it does it tends to be incomplete and not standardised. Scales can offer a simple way to convey this information, and the BBAT could be an appropriate tool for this purpose. Comparing of the assessment made in the maternity ward to the assessment obtained at the PCC would provide professionals useful information about the evolution of BF and whether more or less support is required. However, this application has not even been explored, and studies are required to corroborate its usefulness.
The main limitation of our study was the lack of a gold standard that could serve as reference. This is one of the main concerns in the validation of BF observation scales. Nevertheless, the findings in our study and the previous evidence on the BBAT scale show good results that are consistent with other feeding observation scales (LATCH) and BF self-efficacy scales (BSES-SF). Further research is required on the predictive validity of the BBAT and to obtain more evidence on its validity in different settings and circumstances.
In conclusion, the Spanish translation of the BBAT presented in this study exhibited adequate validity and reliability for use in the clinical assessment of a BF session by paediatricians and paediatric nurses.
Conflict of interestsThe authors have no conflicts of interests to declare.
We thank Dr Jenny Ingram for allowing us to adapt the scale and for reviewing the back translation. We also thank all the mothers and infants who participated in the study.
Please cite this article as: Balaguer-Martínez JV, Esquivel-Ojeda JN, Valcarce-Pérez I, Ciriza-Barea E, García-Sotro C, López-Santiveri A, et al. Traducción al español y validación de una escala para la observación de una toma de lactancia materna: la «Bristol Breastfeeding Assessment Tool». An Pediatr (Barc). 2022;96:286–293.
Previous presentation: the results of this study were presented as a communication in the online course Actualización en Pediatría 2021.