Metabolic bone disease of prematurity (MBDP) is a well-known neonatal disease characterized by a reduction in bone mineralization. It chiefly affects preterm (PT) newborns in the first weeks post birth and can result in bone density below the expected values for gestational age (GA) and length,1,2 in addition to other short- and long-term complications.
The etiology of MBDP is multifactorial, and precise diagnostic criteria have yet to be established due to a lack of consensus as to its characteristic markers. This lack of consensus regarding the diagnosis of MBDP makes it difficult to calculate its incidence, with estimates in the literature ranging from 20% to 35% of extremely low birth weight newborns.1–4
The complications associated with MBDP, such as prolonged ventilator dependence, risk of fracture, abnormal bone development, ophthalmological abnormalities and renal failure, have a severe impact not only on the patient, but also on families, by prolonging hospital stays and increasing stress, and on the health care system, as they increase health care expenditure and resource consumption.4,5
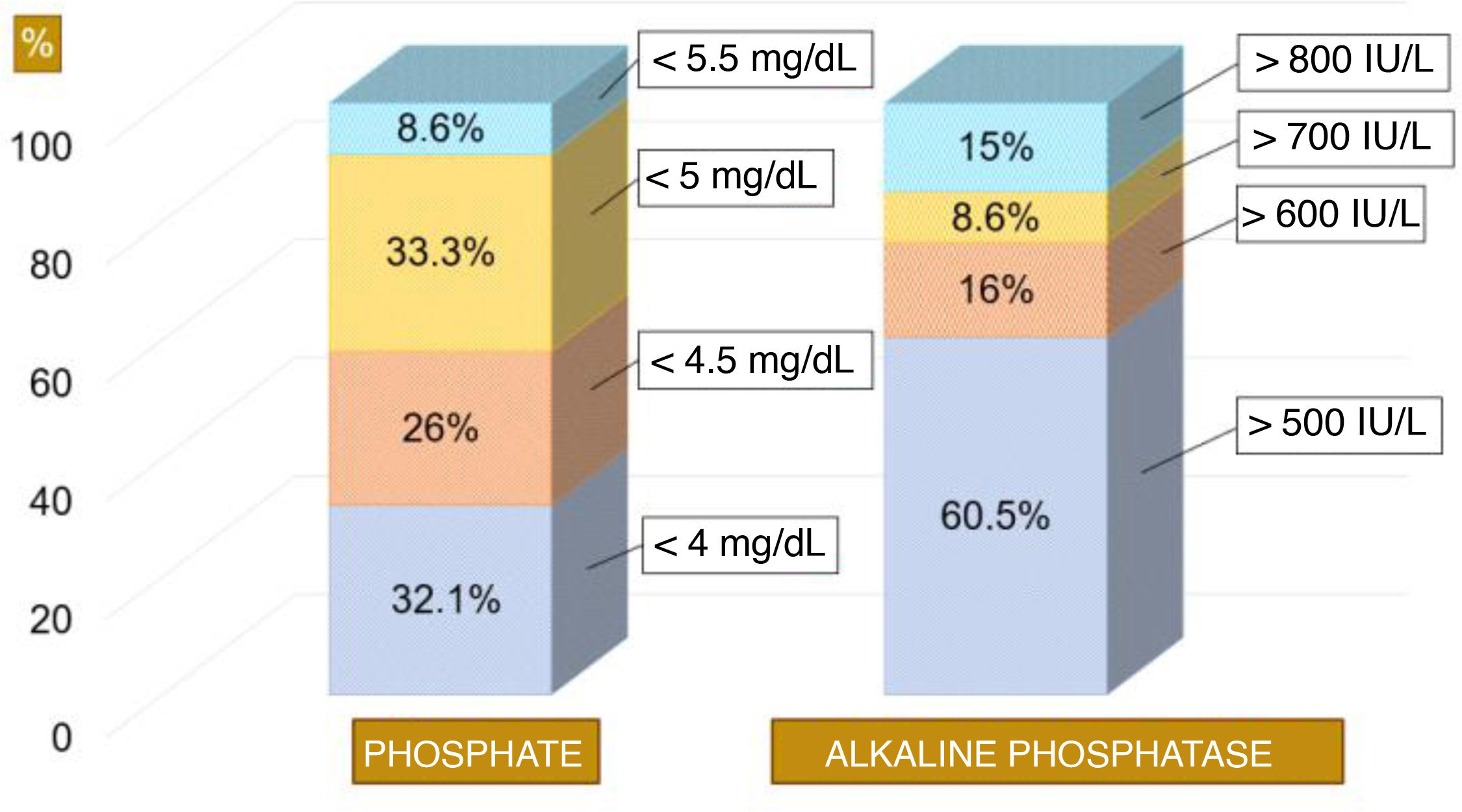
To date, hypophosphatemia and hyperphosphatasia have been the most widely used markers for diagnosis of MBDP,1 although there is no consensus on the thresholds used to define pathological values. For instance, the 2023 protocol of the Sociedad Española de Neonatología (SENeo, Spanish Society of Neonatology) proposes phosphate thresholds of less than 4mg/dL (hypophosphatemia) and greater than 500 IU/L (hyperphosphatasia) to define the risk of osteopenia, but the cutoffs differ between centers and protocols, underscoring the need to standardize diagnostic criteria and make the management of this disease more homogeneous.
For this reason, we conducted a prospective cross-sectional study through an online survey of neonatologists in Spain in 2023. The primary objective was to assess the level of consensus in the interpretation of biomarkers, the diagnosis and the treatment of MBDP in neonatal units in Spain.
The questionnaire comprised 12 items: eight pertaining to diagnosis (normal values of phosphate and alkaline phosphatase [AP], screening criteria and timing, eligibility, and methodology of screening), and four to management (initiation and completion of treatment, monitoring and follow-up).1–4 We defined consensus as agreement in 75% or more of respondents (Table 1).
List of the 12 items included in the questionnaire by topic under study.
| Items | Most frequent choice | ||
|---|---|---|---|
| Diagnostic | Pathological phosphate value | <5mg/dL | 33% |
| Pathological AP value | >500IU/L | 60.5% | |
| Timing of screening | 4 weeks post birth | 58% | |
| Does infant feeding modality affect timing of initial screening? | No | 94% | |
| Screened population | PT infants<1500g or born at GA<32 weeks without considering other risk factors | 67% | |
| Screening method | Blood chemistry and urine testing | 58% | |
| Inclusion of PTH and vitamin D in screening | Yes | 50% | |
| Radiological diagnosis | No | 81.5% | |
| Therapeutic | Treatment | Increase fortification to maximum and, if needed, add calcium and/or phosphorus supplementation | 80% |
| First monitoring | Two weeks after screening | 80% | |
| Time treatment ends | Normalization of AP values | 78% | |
| Follow-up | Yes | 98.8% | |
The table shows the answer chosen most frequently by respondents and the percentage of agreement for the item. We defined consensus as agreement of at least 75% of respondents (highlighted in green).
AP, alkaline phosphatase; GA, gestational age; PT, preterm; PTH, parathyroid hormone.
We received 81 responses (n=81). There was no consensus regarding the population in which screening is indicated, the tests that need to be performed nor the biomarker values that are considered pathological, including phosphate and APs levels. The phosphate range most frequently considered pathological in the literature (<5.5mg/dL)1,3 was only considered pathological by 8.6% of respondents. Alkaline phosphatase levels were considered high (> 500 IU/L) were considered high in 60.5% of cases (Fig. 1). Fifty-eight percent of neonatologists performed the first screening at 4 weeks post birth (Table 1).
In respect of the population eligible for screening, most respondents (67%) ordered screening in PT infants with birth weights of less than 1500g or born before 32 weeks’ gestation, without considering other risk factors. Fifty-eight percent of respondents reported that screening consisted of blood chemistry and urine tests. When it came to measurement of parathyroid hormone (PTH) and vitamin D levels, only half the units ordered them as part of the initial screening (Table 1).
As regards treatment, 80% of respondents increased fortification and added oral supplementation as needed. The first post-treatment checkup was carried out in two weeks in 80% of cases. Although MBDP has specific radiological features, 81.5% of respondents did not order imaging. Lastly, 78% of neonatologists discontinued supplementation once PA values normalized (Table 1).
The main limitations of the study concerned the design of the survey, as participation was anonymous and no information was collected regarding the characteristics of the facility, including the level of care, nor the experience of the respondent. However, we believe that the findings reflect the current heterogeneity in the diagnosis and management of this disease.
In conclusion, MBDP is a disease whose incidence and biomarker thresholds have yet to be clearly established, as evinced by the findings of our survey. There is substantial variation in the diagnosis and treatment of this disease between neonatal units in Spain. The lack of established protocols poses a barrier to the adequate management of these patients, increasing the risk of complications.1–5 In consequence, we hope that this study will inspire a collective effort to review and unify existing protocols in order to provide a clearer and more concise set of diagnostic criteria and therapeutic guidelines for the management of this disease, which is frequently encountered in neonatal care.