By using path analysis, the aim of this study is to show how anxiety, low self-esteem and a decrease in hours of sleep interact to lead to an increase in overweight in children.
MethodA random sample of 291 schoolchildren was included. A cross-sectional design was used, measuring their body mass index (BMI) and applying the Stait-Trait Anxiety inventory for Children and the Children’ Depression Inventory.
ResultsThe mean sleep time was 9h and 50min. There was an inverse relationship between hours of sleep and BMI. Similarly, anxiety and low self-esteem were predictors of the number of hours of sleep.
ConclusionsThese data allow it to be concluded that, on one hand, the population studied sleeps less than the 10 or 11h recommended for their age. On the other hand, it has been demonstrated how certain emotional states can encourage increased BMI in children, but this relationship is associated with reduced sleep.
En este estudio, utilizando el path anaylisis, se pretende mostrar cómo la ansiedad, la autoestima negativa y el sueño interaccionan favoreciendo el sobrepeso infantil.
MétodoParticiparon en la investigación 291 niños de los que se obtuvo su índice de masa corporal (IMC) y se les aplicó el Cuestionario de Autoevaluación Ansiedad Estado/Rasgo para niños y la Escala de autoestima del Inventario de Depresión Infantil.
ResultadosLa media de sueño diaria fue 9 h y 50min. La ansiedad-rasgo y autoestima predijeron un menor número de horas de sueño y las horas de sueño, a su vez, un IMC más elevado.
ConclusiónEstos datos permiten concluir, por una parte, que la población estudiada duerme menos de las 10 u 11 h recomendadas para su edad. Por otra parte, se ha mostrado cómo determinados estados emocionales pueden favorecer el incremento del IMC en los niños, pero dicho incremento estaría relacionado con la reducción de horas de sueño asociada a esos estados emocionales.
There is wide agreement among researchers that childhood overweight and obesity may become a pandemic in the course of this century. It is estimated that up to two thirds of obese children will grow up to be obese adults.1–3
The prevalence of childhood overweight and obesity in Spain is of around 31–35%.4–6 This is due to a set of factors that act in synergy to promote weight gain. In this study we focused on three elements: anxiety, low self-esteem, and sleep. Several studies have found a significant association between anxiety and an increase in body mass index (BMI) in children of both sexes.7–9
Likewise, low-self esteem has also been associated to childhood overweight.10 Studies on the subject usually show that the self-esteem of overweight children is lower than that of children with normal weights.11 But few studies have tried to show the mechanism by which self-esteem contributes to overweight.
One factor that has a significant influence on childhood overweight along with emotional states is sleep duration. The literature suggests that there is an inverse correlation between sleep duration and the risk of developing overweight or obesity during childhood.12,13 Children who sleep fewer hours are more likely to be overweight or obese. More specifically, 10-year-old children should sleep at least 10 or 11h a day. Thus, the 50th percentile for total sleep duration in this age group is above 10h.14 The risk of overweight is greater in children who sleep less than 9h a day.15
Anxiety, self-esteem and sleep duration are independently associated to weight gain in childhood. Still, those two emotional variables also influence sleep.16 Thus, for instance, it has been established that there is a significant inverse correlation between sleep duration and trait-anxiety scores.17
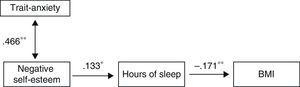
In this study we used path analysis to test a theoretical model that posits that trait-anxiety and low self-esteem can promote weight gain in children by decreasing sleep duration.
MethodParticipantsWe obtained a random sample from the school system of the Principality of Asturias. To select the sample, we requested a complete enrolment list of all public schools that taught 4th year of primary school from the Consejería de Educación (Department of Education) of the Principality of Asturias, Spain. Participants were selected by randomised cluster sampling to obtain representative results that could be generalised to the general population of Asturias within this age range. Each school was considered a cluster. Sample size was calculated a priori to obtain a midrange effect size (effect size d=0.5),18 type I error (probability of ¿ error=0.05) and sampling power (1−probability ¿ error=0.95) using the GPower 3 application.19 This calculation set a minimal sample size of 252 participants. We assessed a total of 291 children from a total of 30 public schools in the Principality of Asturias. Girls accounted for 48.50% of the sample, and boys for 51.50%, with a mean age of 9.33 years and a standard deviation of 0.55.
ToolsWe used the following tools in this study: a Firstline FPS4141 digital scale to measure the weight and a Kóndor CF265 measuring tape to measure height. These 2 measurements were used to calculate the BMI.
The State-Trait Anxiety Inventory for Children (STAI-C)20 consists of 40 items rated on a Likert scale. It can be administered to single individuals or to groups, and completing it takes between 15 and 20min. It is appropriate for its use in children between 8 and 15 years of age. The Trait-Anxiety scale consists of 20 items through which the participant can express “how he or she feels in general”. We only used the Trait-Anxiety scale in the study because this variable is likely to be more stable and thus may have a stronger association with the BMI dependent variable.
The Children's Depression Inventory (CDI)21 consists of 27 items with three possible answer choices. It can be administered to individuals or groups, and completing it takes between 15 and 20min. It is used in children 7–15 years of age to measure dysphoria and poor self-esteem. In the process of giving informed consent, the parents also answered a question about the time their children went to bed and got up both on weekdays and during the weekend.
ProcedureWe sent letters to parents requesting their informed consent for the participation of the children in a study of childhood lifestyle habits to be performed during school hours. We assured them that the data would be kept confidential and that participation would be anonymous.
The study involved an individual interview with each participant in a school office. All children consented to participate in the study. The height and weight of the children were measured and recorded before starting the interview, and were used later to calculate their BMI applying the cut-off values specified by Cole et al.22 These cut-off values are an international reference used in many epidemiological studies, which helps make direct comparisons of childhood obesity trends across the world.
Participants were barefoot for the measurement of weight and height, standing straight with the chin parallel to the floor. To verify the reliability of the height measurements, a series of 50 measurements was performed and compared to another such series carried out by a different researcher, which resulted in a good value of the kappa coefficient for inter-rater agreement (0.75). The intra-rater reliability was even higher (0.79).
After the personal interview, the trait-anxiety scale of the STAI-C and the negative self-esteem subscale of the CDI were administered to each participant. All participants were given the necessary directions to fill out each of the questionnaires correctly, and the research team addressed any questions that arose before and during the process. Before the participants left after completing the questionnaires, the materials were reviewed to ensure that participants had followed the instructions given to them.
To establish the number of hours that children slept daily, participants were asked which time they got up and which time they went to bed. To establish the children's bedtimes, they were asked what they did before going to bed. Since most of them reported that they watched television before bed, they were asked what show they watched each day of the week before going to bed, and until what time or whether they watched the entire programme. To determine the number of hours spent watching television, the children were shown a TV guide that specified the actual duration of the programmes in order to obtain more reliable answers, and it is worth noting that the children seemed eager to point out the programmes they watched and see their ratings. Thus, bedtimes could be established with greater accuracy. Then, the daily hours of sleep were calculated using the times reported by the child for going to bed and getting up. The parents also answered a question about the number of hours that their child slept a day in the questionnaire sent to them along with the consent form. Subsequent analyses used the number of hours of sleep reported by the child to the researcher, as this variable was considered more suitable because it had been collected in a more objective and controlled manner.
Data analysisThe statistical analysis consisted of a path analysis performed with the Mplus 5 software.23 The analyses employed a fundamentally confirmatory logic. The model was evaluated based on the statistical significance of the chi-squared test and goodness of fit measures that included the Tucker Lewis Index (TLI), the Comparative Fit Index (CFI) and the Root Mean Square Error Approximation (RMSEA).
ResultsApplying the cut-off values set by Cole et al.,22 the prevalence of overweight and obesity was 31.3% and 12.4%, respectively. When it came to sex (see Table 1), the data showed that the percentage of overweight was higher in girls (33.8%) than in boys (28.9%), while obesity was more prevalent in boys (13.4%) than in girls (11.3%).
Of all participants, 24.5% (25.9% of boys and 23.4% of girls) scored above the 70th percentile in the trait-anxiety scale. As for negative self-esteem, 36.3% of participants (33.4% of boys and 38.9% of girls) scored above the 70th percentile. We used Student's t-test to compare the scores obtained by boys and girls in the trait-anxiety scale and the negative self-esteem subscale (see Table 2), and found no statistically significant differences (t [283]=−1.037; P>.05).
We found a positive correlation between the data for the number of sleep hours collected during the study and the number of hours reported by the parents (r=0.274; P<.001). These two variables appear to be related; however, we observed that the mean hours of sleep reported by parents was 9.55h, fewer than the mean hours of sleep documented during the study, which was 9.84h.
Before performing the path analysis, we did other analyses to identify outlier cases by means of box plots and normality tests, such as checking whether the skewness and kurtosis statistics were within the −1 to +1 range. Box plot diagrams did not reveal atypical values, although we found that 9 cases were far from the mean for the variable corresponding to the daily hours of sleep. The skewness and kurtosis values fell within the −1 to +1 range, as shown in Table 3.
Skewness and kurtosis statistics.
| Mean | Standard deviation | Skewness | Skewness standard error | Kurtosis | Kurtosis standard error | |
|---|---|---|---|---|---|---|
| Negative self-esteem | 5.43 | 2.759 | 0.301 | 0.144 | −0.231 | 0.288 |
| Trait-anxiety | 32.89 | 5.813 | 0.326 | 0.142 | −0.309 | 0.284 |
| Body mass index | 19.594 | 3.22 | 0.691 | 0.142 | 0.209 | 0.284 |
| Daily hours of sleep | 9.84 | 0.679 | −0.381 | 0.143 | 0.519 | 0.284 |
Table 4 shows the correlation matrix for the variables under study: negative self-esteem, trait-anxiety, BMI, and number of hours of sleep per day.
We developed different linear regression equation models with the variables noted above, treating BMI and daily hours of sleep as criterion variables. Table 5 lists the standardised coefficients, the significance of these coefficients, and the explained variance percentage for each model. Table 5 shows the emotional variables model with the variables centred around zero. This model did not reach statistical significance to predict BMI (F [2.281]=0.932, P=.395) and explained 0.01% of the variance (adjusted R2). However, these variables provided a statistically significant model for predicting daily hours of sleep (F [2.280]=3.877, P=.022), explaining 2.0% of the variance (adjusted R2). The model that had the daily hours of sleep as the dependent variable found that negative self-esteem predicts a reduced number of sleep hours (¿=−0.126; P=.050).
We used the associations that had showed a statistically significant correlation to develop the path analysis model (see Table 4) and the linear regression equations (see Table 5). Our model used maximum likelihood estimation.
The path analysis (Fig. 1) showed that the tested model based on the previously found significant correlations was a good fit. The chi-squared test did not reach statistical significance (4.498, P=.17); the CFI and TLI goodness-of-fit indices were 0.982 and 0.965, respectively, and the RMSEA had a value of 0.041, with a confidence interval of 0.000–0.114.
DiscussionThe model obtained through path analysis showed that high trait-anxiety and negative self-esteem scores are associated with an increase in BMI. But this relationship between these emotional states and childhood overweight is itself associated to a reduction in sleep duration, which supports our initial hypothesis. Children aged 9 and 10 years who have higher anxiety and negative self-esteem scores are more likely to be overweight, and this can be explained by the effect that these emotional states have on sleep duration, which would be the factor directly associated with weight gain.
This finding is consistent with recently published data that shows the role of reduced sleep duration in the increase of childhood overweight.24–28
More than half the children in Spain sleep less than the 10 or 11h recommended for their age. In our study, the mean duration of daily sleep was 9h and 50min, which means that many children sleep between 1 and 2h less than recommended. Correcting this habit (which would have a direct effect on children's health and specifically on their BMI) would require changing the lifestyle factors that make children in this age group go to bed after 10 pm, such as inappropriate television watching.
The relationship between the reduction in sleep duration and overweight could be due to hormonal changes that cause sleeplessness. Among these changes, we would like to mention decreased tolerance to glucose and insulin sensitivity; an increase in cortisol levels in the afternoon; and elevated ghrelin levels and reduced leptin levels leading to increased hunger and difficulty reaching satiety.25 Furthermore, reduced sleep duration is also associated with the consumption of higher-energy foods, and thus with an increased calorie intake.15
In the model presented in this study, low self-esteem predicts, albeit indirectly, BMI increases in children. This suggests that there is a feedback loop between these two variables, as the literature has consistently shown that one of the psychological effects of childhood overweight is low self-esteem.11,29,30 Thus, it appears that low self-esteem in children both causes and results from childhood overweight. In this regard, Ternouth et al.31 showed how emotional problems, low self-esteem and an external locus of control are risk factors and predictors of greater weight gain in adulthood.
On the other hand, the effect of anxiety on sleep is also well known. This emotional state can result in difficulty falling asleep or in waking up early, leading to a reduction in sleep duration. Furthermore, the psychophysiological changes that cause anxiety and lack of sleep promote one another in a feedback loop,32 and lead to a higher calorie intake and a lower energy expenditure.33,34
It has been shown that overweight children score significantly lower than their normal weight counterparts in all areas of self-esteem, especially as it regards physical appearance and athletic ability. Furthermore, girls that have a high BMI and whose parents criticise their excess weight report having a very poor body image.16 In our study we observed that negative self-esteem and overweight can form a vicious circle, as self-esteem is associated with a reduction of sleep duration that may further promote overweight, while overweight leads to a more negative self-esteem. The model presented here does not explain a high percentage of the variance. However, it must be taken into account that only a small part of the paediatric population has anxiety and low self-esteem. It is estimated that about 10% of overweight boys and 20% of overweight girls have a low overall self-esteem.29 Moreover, a child's BMI is determined by a broad range of variables. This accounts for the amount of variance that this model can explain.
One of the main inferences that could be drawn from this study has to do with preventing childhood overweight. Ensuring proper sleep duration may be a key element in prevention, and in some cases this could entail the management of emotional states like anxiety or low self-esteem.29,35
One of the limitations of this study is its cross-sectional design, which may put in question the importance of the relationships between the studied variables.36 Still, the use of path analysis helps overcome this problem if only partially, as this method involves the a priori development of a theoretical model based on literature review and in which the relationships between a series of variables are established later on by the use of statistical methods.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Amigo-Vázquez I, Busto-Zapico R, Peña-Suárez E, Fernández-Rodríguez C. La influencia del sueño y los estados emocionales sobre el índice de masa corporal infantil. An Pediatr (Barc). 2015;82:83–88.