Breastmilk is the best food for newborns and infants. The nutritional stores of a lactating woman may be more or less depleted as a result of the pregnancy and the loss of blood during childbirth. Lactation raises nutrient needs, mainly because of the loss of nutrients, first through colostrum and then through breastmilk.
Breastmilk volume varies widely. The nutrients present in this milk come from the diet of the mother or from her nutrient reserves.
The conversion of nutrients in food to nutrients in breastmilk is not complete. To have good nutritional status the breastfeeding woman has to increase nutrient intake. Human breastmilk has a fairly constant composition, and is only selectively affected by the diet of the mother. The fat content of breastmilk varies somewhat. The carbohydrate, protein, fat, calcium and iron contents do not change much, even if the mother is short of these in her diet. A mother whose diet is deficient in thiamine and vitamins A and D, however, produces less of these in her milk. The mother should be given advice on consuming a mixed diet. At each postnatal visit, both the mother and the baby should be examined, and advice on the diets of both mother and infant should be provided. A satisfactory gain in the infant's weight is the best way to judge the adequacy of the diet of the infant. Mothers should not receive less than 1800 calories per day.
La leche materna es el mejor alimento para los recién nacidos y lactantes. Las reservas nutricionales de una mujer lactante pueden estar más o menos agotadas como resultado del embarazo y la pérdida de sangre durante el parto. La lactancia plantea necesidades nutricionales especiales, principalmente debido a la pérdida de nutrientes a través de la leche materna.
El volumen de leche materna varía ampliamente. Los nutrientes presentes en la leche proceden de la dieta de la madre o de sus reservas de nutrientes.
Para conseguir un buen estado nutricional durante la lactancia, la mujer tiene que aumentar la ingesta de nutrientes. La leche materna tiene una composición bastante constante y la dieta de la madre solo afecta a algunos nutrientes. El contenido de grasa de la leche materna varía con la dieta. El contenido de hidratos de carbono, proteína, calcio y hierro no cambia mucho incluso si la madre ingiere poca cantidad de estos en su dieta. Sin embargo, si la dieta de una madre es deficiente en vitaminas hidrosolubles y vitaminas A y D, su leche contiene menos cantidades de estos nutrientes. En cada visita posnatal tanto la madre como el niño deben ser examinados, y se debe proporcionar asesoramiento sobre la alimentación saludable. Durante la lactancia se debe evitar una dieta que aporte menos de 1.800 cal al día.
Breast milk must guarantee the adequate nutrition of the infant as a continuation of intrauterine nutrition, and both the mother's nutritional status as well as her diet may influence breast milk composition, and therefore nutrient intake in the infant.
Nutritional requirements are higher in infancy than in any other stage of development, and there is evidence that the composition of breast milk changes with time to adjust to the changing needs of the child.1–4
Although there is a vast body of literature on the physiology and disease of lactating women, the professionals that care for them often lack adequate knowledge about their nutritional requirements.5 This document aims to offer updated information on the nutrition of the breastfeeding mother to facilitate the development of health care protocols based on current knowledge.
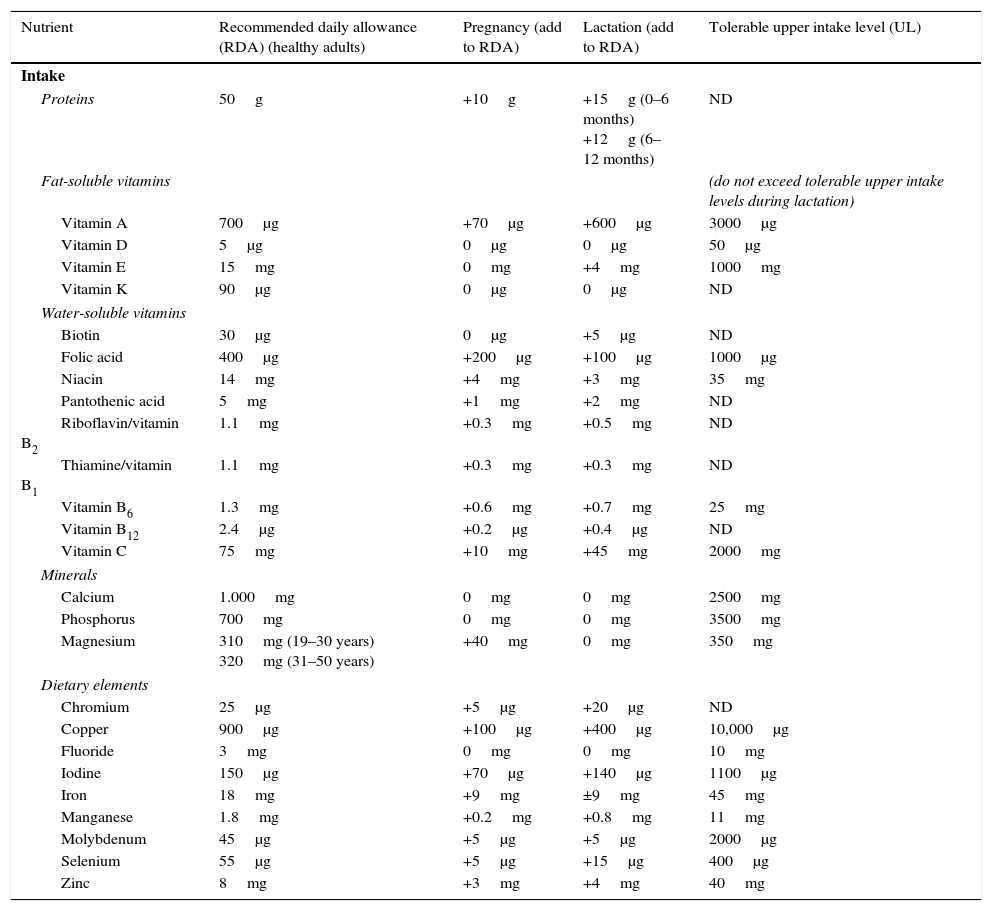
The nutritional requirements of women increase during pregnancy and lactation (Table 1).1 During lactation, the mammary glands have a degree of metabolic autonomy that guarantees adequate milk composition. Unless they are extremely malnourished, all mothers can produce milk in appropriate amounts and of appropriate quality.
Minimum nutrient requirements for healthy women as well as pregnant and lactating women.
| Nutrient | Recommended daily allowance (RDA) (healthy adults) | Pregnancy (add to RDA) | Lactation (add to RDA) | Tolerable upper intake level (UL) |
|---|---|---|---|---|
| Intake | ||||
| Proteins | 50g | +10g | +15g (0–6 months) +12g (6–12 months) | ND |
| Fat-soluble vitamins | (do not exceed tolerable upper intake levels during lactation) | |||
| Vitamin A | 700μg | +70μg | +600μg | 3000μg |
| Vitamin D | 5μg | 0μg | 0μg | 50μg |
| Vitamin E | 15mg | 0mg | +4mg | 1000mg |
| Vitamin K | 90μg | 0μg | 0μg | ND |
| Water-soluble vitamins | ||||
| Biotin | 30μg | 0μg | +5μg | ND |
| Folic acid | 400μg | +200μg | +100μg | 1000μg |
| Niacin | 14mg | +4mg | +3mg | 35mg |
| Pantothenic acid | 5mg | +1mg | +2mg | ND |
| Riboflavin/vitamin B2 | 1.1mg | +0.3mg | +0.5mg | ND |
| Thiamine/vitamin B1 | 1.1mg | +0.3mg | +0.3mg | ND |
| Vitamin B6 | 1.3mg | +0.6mg | +0.7mg | 25mg |
| Vitamin B12 | 2.4μg | +0.2μg | +0.4μg | ND |
| Vitamin C | 75mg | +10mg | +45mg | 2000mg |
| Minerals | ||||
| Calcium | 1.000mg | 0mg | 0mg | 2500mg |
| Phosphorus | 700mg | 0mg | 0mg | 3500mg |
| Magnesium | 310mg (19–30 years) 320mg (31–50 years) | +40mg | 0mg | 350mg |
| Dietary elements | ||||
| Chromium | 25μg | +5μg | +20μg | ND |
| Copper | 900μg | +100μg | +400μg | 10,000μg |
| Fluoride | 3mg | 0mg | 0mg | 10mg |
| Iodine | 150μg | +70μg | +140μg | 1100μg |
| Iron | 18mg | +9mg | ±9mg | 45mg |
| Manganese | 1.8mg | +0.2mg | +0.8mg | 11mg |
| Molybdenum | 45μg | +5μg | +5μg | 2000μg |
| Selenium | 55μg | +5μg | +15μg | 400μg |
| Zinc | 8mg | +3mg | +4mg | 40mg |
ND, not determined due to a lack of studies in these population subsets; RDA, recommended dietary allowance.
The intake must come from food sources to avoid potential overdoses.
Variations in the diet of the mother may result in changes in the fatty acid profile and levels of certain micronutrients, but they are not associated with the volume or quality of the milk produced. The milk of all mothers, even those that are malnourished, has an excellent nutritional and immunological quality. The mother's body always prioritises the needs of the baby, and consequently most nutrients, such as iron, zinc, folate, calcium and copper continue to be excreted in breast milk in adequate and constant amounts, at the expense of maternal stores. In the event of famines and disasters, and when there is risk of child malnutrition, the approach recommended by the WHO is to support breastfeeding, which guarantees the correct development of the baby, and to supplement the diet of the mother.6–8
The energy, proteins and nutrients in human milk come from the diet as well as maternal body stores. Women that do not obtain sufficient nutrients from dietary sources may be at risk of deficiency in some minerals and vitamins that perform important functions. These deficiencies can be prevented if the mother improves her diet or takes nutritional supplements.
The age, baseline postpartum weight, level of activity and individual metabolism will influence the amount of food each woman needs to consume to achieve an optimal nutritional status and an adequate milk supply. The duration and intensity of breastfeeding also have a significant impact on maternal nutritional requirements, but are rarely taken into consideration.9
The prevalence of nutrient deficiencies varies based on geographical region, culture, dietary habits and socioeconomic level.10–13 In Spain, micronutrient deficiencies are more common than energy or protein deficiencies. The content of some nutrients in human milk depends on the mother's dietary intake, especially if her diet is inadequate, and in most cases these deficits can be corrected by means of supplementation.14
The concentration of water-soluble vitamins in breast milk is highly dependent on maternal intake levels. The fat-soluble vitamin concentrations depend mostly on maternal stores, although they may be increased by exogenous sources.
It has been demonstrated that maternal requirements may also vary through different stages of lactation.15 An adequate energy intake and a balanced diet including fruits, vegetables and animal source foods help women go through pregnancy and lactation without deficiencies. Some nutrient requirements, especially iron, iodine, folic acid and vitamin A requirements, are more difficult to meet through dietary sources, and therefore mothers may need to take supplements or natural foods fortified with these nutrients.
Nutritional requirements during lactationWe ought to highlight that nutritional requirements are considerable higher during lactation than during pregnancy. During the first four to six months of life, the infant doubles the weight gained during the nine months of gestation. The milk produced in the first four months of lactation constitutes an amount of energy that is equivalent to the total energy expenditure of gestation.16
Nutritional requirements may change based on maternal age, which may impact maternal nutritional status and milk composition to varying degrees, especially in adolescent or malnourished mothers.17,18
EnergyThe nutritional recommendations for lactating women are somewhat empirical and essentially based on the volume and composition of the milk produced. In the six months that follow birth, approximately 750mL of milk are produced per day, and 100mL of breast milk provide an average of 70kcal of energy to the child. It is estimated that approximately 700kcal are required to produce one litre of milk. But the energy requirements of a lactating mother should not be calculated simply as the sum of the requirements of an adult woman that is not lactating and the calories administered to the child through breast milk, as many nutrients stored during gestation are available to support milk production.
A third of the additional energy expenditure (±150kcal/day) is due to the mobilisation of maternal stores.16
We recommend against weight-loss diets that provide fewer than 1800kcal a day, as inadequate intakes may deplete maternal stores. Intakes below 1500kcal/day may cause fatigue and a decreased milk supply. If more rapid weight loss is desired, dietary restrictions should be combined with physical exercise.
The total energy intake recommended for lactating mothers ranges between 2300 and 2500 calories a day for feeding a single child, and 2600 and 3000 calories a day for feeding twins.
ProteinThe increase in protein requirements during lactation is minimum compared to energy requirements. However, if the energy intake is low, protein will be used for energy production. The additional requirements during lactation can be satisfied by consumption of protein-rich foods (for example, one egg, 25g of cheese or 175g of milk).
If the protein intake is insufficient, the concentration of casein in milk may be inadequate. Casein is an important nutritional component of milk, and it is needed for the absorption of calcium and phosphate in the gut of the infant and has immunomodulatory functions.
Insulin resistance depends on the quality of the protein contributed by the diet rather than on its amount, and thus, consumption of fish-derived proteins during breastfeeding seems to have long-term beneficial effects on insulin regulation and sensitivity.
CarbohydrateLactose is the predominant carbohydrate in human milk and is essential to the nutrition of the infant's brain. While the concentration of lactose is less variable than that of other nutrients, the total production is reduced in mothers with severe malnutrition.18
FatThe lipids in breast milk are the fraction that most contributes to its energy content, yet they are the components that vary most in their distribution and quality. Maternal malnutrition is associated with lower concentrations of lipids in breast milk. The distribution pattern of fatty acids in breast milk is also sensitive to the mother's diet.19–21 Docosahexaenoic acid (22:6 n23) is a nutrient with a limited endogenous biosynthesis, so it must be obtained through the diet, as it is the most important omega-3 acid for the optimal development of the brain, retina and ear. The cholesterol content of breast milk is highly variable and is related to the duration of breastfeeding, maternal age, maternal diet, season and place of residence.22
The relative contribution of fat to the total energy intake recommended during breastfeeding is the same as the one recommended for the general population. Foods that contain fat must be ingested in adequate amounts. Some studies have shown that maternal intake of fish and fish oils has a positive impact on birth weight and is associated with a lower risk of preterm birth and even with better neurodevelopmental outcomes.23
It is recommended that women of child-bearing age consume one to two servings of seafood a week, including fatty fish or small-sized bluefish, such as sardines, to avoid exceeding tolerable upper intake levels of environmental pollutants. The consumption of some large fish species such as swordfish and tuna must be reduced, as they may have higher mercury concentrations.
WaterWater accounts for 85–95% of the total milk volume. There is a widespread belief that increasing water intake will increase milk production, but several studies have demonstrated that forcing the intake of fluids beyond that needed to quench thirst has no beneficial effects on lactation.18
SaltThe concentration of sodium is higher in colostrum than in mature milk. Research has found no evidence of an association between sodium intake during lactation and sodium levels in breast milk. However, it is always advisable to consume small amounts of salt, always enriched with iodine (iodised salt).
VitaminsThe concentration of some vitamins in breast milk depends on their levels in the mother, and deficiencies in the mother can lead to deficiencies in the infant. This is particularly relevant for thiamine (B1), riboflavin (B2), and vitamins B6, B12, E and A, and consequently an increase in their intake is recommended during lactation.3
Fat-soluble vitaminsVitamin AIt is involved in the photochemical reactions of the retina, it is an antioxidant, and has antimicrobial properties. The vitamin A content in milk decreases as lactation progresses. The intake obtained with a balanced diet is adequate and supplementation is not necessary. However, in developing countries it is recommended that all mothers take a single supplementary dose of 200,000IU of vitamin A as soon as possible after delivery.
Vitamin DVitamin D deficiency is fairly frequent in pregnant and lactating women. Mothers that have restricted diets, such as strict vegetarians, and those with limited exposure to UV radiation (mothers with limited exposure to sunlight, with dark skin, or that wear a veil) may have very low plasma levels. The transfer of maternal vitamin D to milk is poor, so it is recommended that all breastfed infants younger than 1 year receive supplementation with 400IU/day of vitamin D, starting its administration within a few days from birth. Supplementation will continue until the child starts consuming one litre of vitamin D-enriched formula a day.24–28
Vitamin EThe concentration of vitamin E in breast milk is sensitive to maternal intake, so the maternal diet must be assessed and supplemented if intake is inadequate.3,28
Vitamin KVitamin K is also synthesised by bacteria lining the gastrointestinal tract. If the diet is adequate, the lactating mother does not require vitamin K supplementation. Newborns usually have low levels of vitamin K, as this vitamin is not easily mobilised through the placenta and the bacterial flora of the newborn is inadequate for its synthesis in the first days of life. Following birth, intramuscular administration of 1mg of vitamin K is recommended for the prevention of haemorrhagic disease of the newborn. Parents that refuse intramuscular administration of vitamin K are offered the oral route as an alternative (2mg of oral vitamin K at birth, followed by 1mg weekly until week 12 in infants that are partially or exclusively breastfed).
Water-soluble vitaminsThe concentration of water-soluble vitamins in milk depends to a great extent on maternal levels, so that deficiencies in the mother can lead to deficiencies in the infant.3
Vitamin B6 (pyridoxine)In the early weeks of life, the vitamin B6 stores accumulated during pregnancy are crucial in maintaining adequate levels in breastfed children. The manifestations of vitamin B6 deficiency in infants also depend on its severity, although in general it presents with neurologic symptoms and different forms of dermatitis.29
Vitamin B12 (cyanocobalamine)Vitamin B12 concentrations in the milk of well-nourished mothers are adequate. However, its levels are low in mothers that are strictly vegetarian (vegan), are malnourished or have pernicious anaemia, even if they do not show signs of deficiency. In these cases, it is important that mothers receive a vitamin B12 supplement the entire time they are breastfeeding, as vitamin B12 deficiency in the infant can have short- and long-term neurological effects.30
Vitamin CThe plasma and tissue concentrations of vitamin C in smokers are lower than in nonsmokers, so an increase in vitamin C intake is recommended in mothers that smoke.
Folic acidThe recommended concentration of folic acid in breast milk can be easily achieved through dietary intake or supplementation, if needed.31
Dietary elements and mineralsCompared to vitamins, the concentrations of minerals do not seem to be correlated to maternal intake, except for iron and iodine.3,4 Copper and zinc concentrations seem to correlate strongly to maternal stores in the liver during the third trimester of the pregnancy, and maternal intake has little influence on them, although their bioavailability in milk is very high. Iodine, iron, copper, magnesium and zinc have a high bioavailability in breast milk. The selenium content is strongly influenced by the mother's diet.
IronIron supplementation is usually recommended to make up for losses sustained during childbirth, although it must be noted that women that practise exclusive breastfeeding usually experience amenorrhoea for a minimum of six months and thus do not lose iron through menstruation during that time. Therefore, it could be said that breastfeeding exerts a protective effect against maternal iron deficiency.9,32
CalciumCalcium is essential during lactation, during which it is subject to special regulatory mechanisms that lead to increased absorption, decreased renal excretion and greater mobilisation of bone calcium. To meet maternal calcium requirements, the American Academy of Paediatrics recommends lactating mothers to consume five servings a day of calcium-rich foods of any kind, such as low-fat yoghourt or cheese, and other nondairy foods that contain calcium, such as fish consumed with its bones (for example, canned sardines), salmon, broccoli, sesame seeds or cabbages, which may provide the 1000–1500mg daily recommended allowance for lactating women.33,34
ZincZinc is essential to growth, cell immunity and enzyme synthesis. While zinc concentrations in human milk are not high, they suffice to satisfy the needs of the child due to its high bioavailability. We recommend increasing zinc intake by 50% during lactation.
SeleniumSelenium is a mineral involved in the immune system, cholesterol metabolism and thyroid function. The concentration of selenium in breast milk is three times that in artificial formulae.
IodineThe iodine requirements of lactating women nearly double those of healthy adult women, as in addition to meeting maternal requirements, iodine levels must guarantee that the baby receives sufficient iodine from the milk to synthesise thyroid hormones.35–37 The iodine content of human milk is variable and depends on maternal intake. In iodine-sufficient regions, the iodine content can reach 200μg/L in colostrum and 100–150μg/L in mature milk.
Since the requirements of the infant are approximately 90μg/day, and the volume of milk ingested ranges between 600 and 1000mL/day, the minimum iodine concentration in breast milk should be 100μg/L. To achieve this, the mother must consume at least 250μg of iodine a day.
Iodised table salt (the source of iodine recommended for all individuals) only contributes half of the required intake during lactation, while salt consumption may decrease during this period. Consequently, and in adherence with the recommendations of the American Thyroid Association, we recommend that breastfeeding women take 200μg a day of supplementary iodine in the form of potassium iodide. When the iodisation of the water supply becomes nationwide and has been established for at least two years, and once its consumption has become widespread in the population, iodine supplementation will no longer be necessary in pregnant and lactating women.
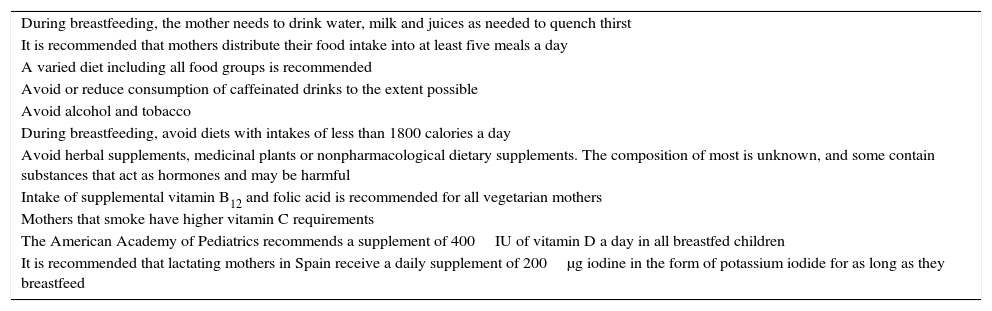
ConclusionsThe unique biological benefits of human milk justify the promotion of breastfeeding as the ideal method for feeding infants. Increased intake of certain nutrients or the use of certain supplements in lactating women is recommended to satisfy the demands of milk production and to protect the infant from nutrient deficiencies38,39 (Table 2).
Dietary and lifestyle recommendations for breastfeeding women.
| During breastfeeding, the mother needs to drink water, milk and juices as needed to quench thirst |
| It is recommended that mothers distribute their food intake into at least five meals a day |
| A varied diet including all food groups is recommended |
| Avoid or reduce consumption of caffeinated drinks to the extent possible |
| Avoid alcohol and tobacco |
| During breastfeeding, avoid diets with intakes of less than 1800 calories a day |
| Avoid herbal supplements, medicinal plants or nonpharmacological dietary supplements. The composition of most is unknown, and some contain substances that act as hormones and may be harmful |
| Intake of supplemental vitamin B12 and folic acid is recommended for all vegetarian mothers |
| Mothers that smoke have higher vitamin C requirements |
| The American Academy of Pediatrics recommends a supplement of 400IU of vitamin D a day in all breastfed children |
| It is recommended that lactating mothers in Spain receive a daily supplement of 200μg iodine in the form of potassium iodide for as long as they breastfeed |
The authors have participated in the conceptualisation and design of this document, the analysis and interpretation of the data, the writing and editing of the manuscript, and the approval of the final text submitted to Anales de Pediatría.
Conflicts of interestThe authors have no conflicts of interest to declare
We thank all the paediatricians that have been members of the Committee on Breastfeeding since its constitution.
Other authors members of the Committee on Breastfeeding are: Marta Costa Romero, Blanca Espinola Docio, Marta Gómez Fernández-Vegue, Beatriz Flores Antón, Ana Gimeno Navarro, Paula Lalaguna Mallada, Jesús Martín Calama, José Manuel Martín Morales and Laura San Feliciano.
Please cite this article as: Ares Segura S, Arena Ansótegui J, Marta Díaz-Gómez N, en representación del Comité de Lactancia Materna de la Asociación Española de Pediatría. La importancia de la nutrición materna durante la lactancia, ¿necesitan las madres lactantes suplementos nutricionales? An Pediatr (Barc). 2016;84:347.
Other authors members of the Breastfeeding Committee of the Spanish Association of Pediatrics are presented in Appendix A.