Attention deficit hyperactivity disorder (ADHD) is the most frequent disorder in childhood and adolescence, and is seen as a public health problem. The recommended treatment includes pharmacological and psychosocial treatment. The aim of this work was to study the changes in the prescribing of the medicines used in ADHD treatment in the Region of Murcia, as well as their socio-demographic variability.
MethodA retrospective observational study was conducted using the dispensing of medicines for ADHD treatment by means of prescription in the Region of Murcia from 2010 to 2014. The consumption rates were determined as defined daily doses (DDD) per thousand inhabitants/day (DIDs), stratified by gender and age. The reasons for prevalence of treatment by gender were also determined by comparing male and female consumption rates.
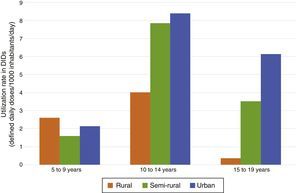
ResultsThe consumption of medicines for ADHD treatment had almost doubled in the period studied, from 5.58 DIDs and 3.39 DIDs in 2010 to 9.34 DIDs and 6.71 DIDs in 2014, for the age range of 10–14 and 15–19, respectively. Boys from 10 to 14 showed the highest consumption rates, showing a high geographical variability with less consumption in rural areas.
ConclusionThe results showed a large increase in the use of medicines for ADHD treatment in the Region of Murcia, although the consumption rates are still lower than in other Autonomous Communities or neighbouring countries. A wide geographical variability was found, with a higher consumption in adolescents from urban areas.
El trastorno por déficit de atención e hiperactividad (TDAH) es la alteración del comportamiento más frecuente en la infancia y la adolescencia, representando un problema de salud pública. El tratamiento recomendado incluye tratamiento farmacológico y psicosocial. El objetivo de este estudio es analizar la evolución del consumo de los fármacos utilizados para el TDAH en la Región de Murcia y su variabilidad sociodemográfica.
MétodoEstudio observacional retrospectivo referido a la dispensación de medicamentos para el tratamiento del TDAH mediante receta en la Región de Murcia entre los años 2010 y 2014. Se calcularon las tasas de consumo expresadas en dosis diarias definidas (DDD) por 1.000 habitantes/día (DIDs), estratificadas por sexo y edad y las razones de prevalencia de tratamiento por sexo comparando las tasas de consumo de hombres y de mujeres.
ResultadosDurante el periodo estudiado prácticamente se ha duplicado el consumo de medicamentos para el tratamiento del TDAH, pasando de tasas de 5,58 DIDs y 3,39 DIDs en 2010 a 9,34 DIDs y 6,71 DIDs en 2014, para las franjas de edad de 10 a 14 años y de 15 a 19 años, respectivamente. Los varones de entre 10 y 14 años presentan las tasas de consumo más elevadas, observándose variabilidad geográfica con menores consumos relativos en las zonas rurales.
ConclusiónSe ha producido un importante aumento del uso de los medicamentos para el TDAH en la Región de Murcia, si bien las tasas de consumo siguen siendo inferiores a los datos de otras comunidades autónomas o países de nuestro entorno. Se observa una gran variabilidad geográfica con un mayor consumo en adolescentes de zonas urbanas.
Attention deficit hyperactivity disorder (ADHD) is the most frequent behavioural disorder in children and adolescents,1 with an estimated prevalence of 5–7% worldwide2–4 and 6.8% in Spain,5 greater in males, and inversely correlated to age.3
This disorder can have a significant negative impact on the children that suffer from it and their social environment (family, school), and is considered a public health problem that adds to the economic burden of families and society overall.6
The treatment recommended by most clinical practice guidelines7 consists of a multimodal approach that includes pharmacological treatment and psychosocial interventions aimed at improving psychological and academic problems. The only drugs indicated for the treatment of ADHD currently distributed in Spain are methylphenidate and atomoxetine, whose use has increased significantly in recent decades.8,9
The aim of this study was to analyse the evolution in the use of the drugs indicated for treatment of ADHD in the Region of Murcia and its variability based on sociodemographic variables.
Materials and methodsWe conducted a retrospective observational study of the drugs in the N06BA group of the Anatomical Therapeutic Chemical classification (centrally acting sympathomimetics) dispensed by all pharmacies in the Region of Murcia to fill out prescriptions issued from the public health system of Murcia. We collected data for the period ranging from January 2010 to December 2014.
The data were retrieved from the billing database of the Colegio Oficial de Farmacéuticos (Official Board of Pharmacists) of Murcia, which contains information for all dispensed prescriptions issued from the public health system of Murcia. The data fields available in the system are the national code, drug name, number of dispensed packages and total cost, as well as geographical variables (health area and municipality) and demographic variables (age and sex). In our study, we collected data for the following variables: drug, number of packages dispensed, year of prescription, sex, age and municipality.
We completed the utilisation data for our study using the Nomenclátor database of the Ministry of Health, which provides information on medicines authorised for use in Spain, to collect data regarding the therapeutic subgroup (active principle), doses per package, units per package and defined daily dose (DDD) for the dispensed medicines. The latter is the unit of measure recommended by the World Health Organisation (WHO) for drug utilisation studies, and expresses the assumed average maintenance dose per day for a drug used for its main indication in adults.
We expressed drug utilisation in terms of daily doses per inhabitant (DIDs), which stands for the DDDs per 1000 inhabitants:
We obtained the annual data for the number of inhabitants from the census-based estimates of the Centro Regional de Estadística (Regional Statistics Centre) of the Region of Murcia.
We performed a descriptive analysis of patients aged 5–19 years stratified by age and sex. Since the percentage of prescriptions with complete patient data (age and sex) varied between the different years under study, we adjusted utilisation rates by the arithmetic mean imputation method,10 with calculation of the 95% confidence interval (CI).
We calculated the treatment prevalence by sex, comparing utilisation rates in male and female patients. We compared the groups by means of contingency tables and the Chi-Square test for association. We defined statistical significance as a P-value of less than 0.05.
We also performed a geographical analysis by municipality for the 2014 data, assessing differences in utilisation based on the type of municipality, categorised based on the definitions of the Law for the Sustainable Development of Rural Areas into rural (those with a population density of less than 100inhabitants/km2 and a population of less than 5000 inhabitants), semi-rural (density of less than 100inhabitants/km2 and population between 5000 and 30,000 inhabitants) and rural.
We set a level of significance of 5% for all statistical tests. We processed the data, performed the statistical analysis and produced charts using the Microsoft® Access 2016 and Microsoft® Excel 2016 software applications.
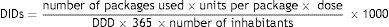
ResultsDuring the period under study, the use of drugs for the treatment of ADHD practically doubled, going from 5.58 DIDs in the 10–14 years age group and 3.39 DIDs in the 15–19 years age group in 2010 to 9.34 and 6.71 DIDs in the same groups in 2014, as can be seen in Fig. 1.
Table 1 shows the utilisation rate by age group and sex, with a higher utilisation between ages 10 and 14 years that increased from 8.63 DIDs in 2010 to 14.77 DIDs in 2014 in boys, and from 2.39 DIDs in 2010 to 3.64 DIDs in 2014 in girls. The highest interannual increase occurred between ages 15 and 19 years, with increases of 17.64% in male patients and 22.53% in female patients.
Rate of ADHD drug utilisation expressed in defined daily doses per 1000 inhabitants per day (DIDs). Region of Murcia, 2010–2014.
| 2010 | 2011 | 2012 | 2013 | 2014 | ACGR (%) | |
|---|---|---|---|---|---|---|
| Male | ||||||
| 5–9 | 2.29 (1.81; 2.91) | 2.55 (2.05; 3.18) | 2.91 (2.37; 3.57) | 3.55 (2.99; 4.21) | 3.7 (3.15; 4.35) | 12.74 |
| 10–14 | 8.63 (7.53; 9.88) | 10.49 (9.3; 11.84) | 13.71 (12.19; 15.42) | 13.25 (11.98; 14.65) | 14.77 (13.46; 16.2) | 14.38 |
| 15–19 | 5.32 (4.51; 6.27) | 6.92 (6; 7.99) | 8.07 (7.05; 9.24) | 9.53 (8.48; 10.71) | 10.19 (9.12; 11.38) | 17.64 |
| ≥20 | 0.46 (0.39; 0.54) | 0.56 (0.48; 0.65) | 0.56 (0.48; 0.65) | 0.55 (0.47; 0.63) | 0.63 (0.55; 0.71) | 8.18 |
| Female | ||||||
| 5–9 | 0.86 (0.58; 1.28) | 0.89 (0.61; 1.3) | 1.1 (0.75; 1.6) | 0.86 (0.61; 1.22) | 0.97 (0.7; 1.33) | 3.05 |
| 10–14 | 2.39 (1.87; 3.07) | 2.83 (2.27; 3.54) | 2.91 (2.34; 3.63) | 3.53 (2.93; 4.24) | 3.64 (3.05; 4.34) | 11.09 |
| 15–19 | 1.34 (0.97; 1.85) | 1.68 (1.26; 2.24) | 2.03 (1.56; 2.64) | 2.42 (1.94; 3.04) | 3.02 (2.48; 3.68) | 22.53 |
| ≥20 | 0.22 (0.19; 0.26) | 0.25 (0.25; 0.25) | 0.28 (0.28; 0.28) | 0.32 (0.32; 0.32) | 0.34 (0.34; 0.34) | 11.50 |
ACGR: annual cumulative growth rate of utilisation of ADHD drugs in defined daily doses per 1000 inhabitants per day (DIDs).
The proportion of male patients receiving pharmacological treatment for ADHD was greater compared to female patients, with the rate peaking at 4.51 (P<.001) in the 10–14 years age group in 2012 (Table 2).
Defined daily dose of ADHD drugs per 1000 inhabitants per day (DIDs) by sex and by age group. Region of Murcia, 2010–2014.
| Year | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|
| 5–9 | 2.9 (2.08; 4.05) | 2.71 (1.98; 3.73) | 2.75 (2; 3.77) | 4.08 (3.09; 5.38) | 3.74 (2.9; 4.82) |
| 10–14 | 3.97 (3.12; 5.06) | 3.6 (2.91; 4.44) | 4.51 (3.66; 5.54) | 3.83 (3.21; 4.57) | 3.97 (3.36; 4.69) |
| 15–19 | 3.88 (2.75; 5.48) | 3.91 (2.88; 5.31) | 3.77 (2.84; 5.01) | 3.77 (2.96; 4.79) | 3.21 (2.59; 3.97) |
| ≥20 | 2.57 (1.25; 5.28) | 3.52 (1.86; 6.65) | 2.98 (1.73; 5.12) | 3.34 (2.05; 5.45) | 2.47 (1.66; 3.7) |
Prevalence rate as ratio of utilisation in male versus female patients.
P<.001 for the entire series.
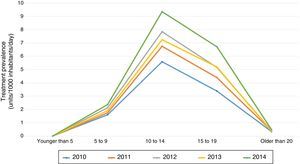
When it came to the consumption data for the 5–19 years age group, we found that methylphenidate was the most frequently dispensed active in every year included in the study, and also the drug whose dispensing experienced the greatest growth, from 3.56 DIDs in 2010 to 5.86 DIDs in 2014 (Fig. 2). The utilisation rate of atomoxetine remained stable in recent years, with a slight increase to 0.52 DIDs in 2014.
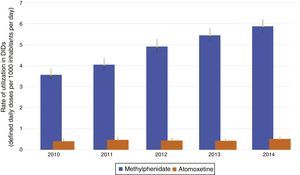
Fig. 3 shows the differences in consumption in the population aged 5–19 years between different municipalities in the Region of Murcia in 2014, with a maximum of 10.54 DIDs in San Pedro del Pinatar and a minimum of 0.67 DIDs in Ulea, and 3 small municipalities where no patients were treated that year: Ojós, Villanueva and Ricote. As can be seen in Fig. 4, differences based on the type of municipality the patient resided in started to appear from age 10 years, with utilisation in urban and semi-rural settings doubling utilisation in rural settings in the 10–14 years age group. This gap widened from age 15 onward, with most of the patients that received treatment residing in urban settings (6.02 DIDs), where the rate nearly doubled that in semi-rural areas (3.51 DIDs), and minimal utilisation in rural settings (0.36 DIDs).
In recent years, there has been a considerable increase in the dispensing of ADHD drugs in the Region of Murcia, as has also been observed in several studies in Spain and abroad. In Castilla y León,9 utilisation grew 18-fold between 2005 and 2009, and there was a similar trend in the Basque Country.11 This has also occurred in other countries, such as Slovenia,12 Switzerland,13 Denmark,14 United Kingdom15 and Germany,16 in every instance coinciding with the introduction in the market of slow-release methylphenidate formulations.
The rate of consumption of these drugs in paediatric patients in the Region of Murcia was considerably lower than the one found in a recent study conducted in the Basque Country,11 where 16 out of every 1000 children aged 6–13 years were receiving treatment with methylphenidate or atomoxetine (15.85 DIDs) in 2012. In the late 1990s, the Region of Murcia was already one of the autonomous communities in Spain where the use of methylphenidate was lowest.8 This study, conducted between 1992 and 2001, found a north–south gradient that has also been observed in relation to other diseases or risk factors,17,18 with higher utilisation rates in Catalonia, Navarre, Rioja, Galicia and Aragon compared to Andalusia, Murcia and the centre of Spain, which the authors associated with variability in medical practice, although it is also possible that this gradient is related with the accessibility of health care services and other aspects derived from economic and cultural factors. We could hypothesise the same in relation to the lower consumption of ADHD medication in rural areas, which may have been due to a lower prevalence of disease, a lower frequency of diagnosis or to parental perceptions regarding the normalcy or abnormality of their children's behaviour. In this study we did not consider or discuss the appropriateness of treatment, although we are aware of the ongoing debate regarding the timing of initiation of pharmacological treatment in patients with ADHD.
Assuming a prevalence of ADHD of 6% for the Region of Murcia based on previous studies conducted in Spain and abroad,2–5 only 1 out of 10 patients with this diagnosis would have received pharmacological treatment, which diverges from the data for the Basque Country, with treatment in 1 out of 6 patients,11,19 or, more significantly, for Denmark14 or the United States,20 where 60% of children with diagnosed ADHD are treated pharmacologically. This may be due to differences in the method used to determine the indication for initiating treatment with methylphenidate.21
The diagnosis of ADHD is based on the observation of the child. Although the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)22 specifies that the symptoms must have a significant negative impact on academic performance and school or social life for ADHD to be diagnosed, physicians sometimes base the diagnosis on the mere presence of symptoms, which may lead to misdiagnosis.23 The criteria of the DSM-5, which is mainly used in the context of clinical practice and scientific research, produces 3–4 times as many diagnoses as the International Classification of Diseases (ICD) approach,24 whose diagnostic criteria are more stringent. Thus, the diagnosis of ADHD may or may not be made depending on the use of one or the other set of criteria, and oftentimes children occupy a grey area in the spectrum of health and disease, so that the final diagnosis and the implementation of treatment ultimately depend on the individual making the assessment and the specific social context.23
The results we obtained regarding the distribution by sex were consistent with the epidemiological patterns observed in ADHD. Treatment with methylphenidate and atomoxetine was 2–4 times more frequent in boys compared to girls,15,25,26 just as the estimated prevalence of ADHD is between 2 and 2.5 times greater in boys.2,19,27 In our study, we found drug utilisation ratios of 2.5–4.5. This is a common finding in the literature, and the DSM22 describes a 4:1 ratio for the general population. The extent to which this is due to sex-based differences in behaviour or to underdiagnosis in the female population is unknown. Several studies have been finding slightly greater growth rates in the prescription of ADHD drugs for the female sex.15,28
In our study, we found the highest prevalence of consumption in the 10–14 years age group, coinciding with the end of primary education and the start of the early cycle or secondary education. A study conducted in Germany16 found a greater prevalence of ADHD between ages 6 and 11 years, although pharmacological treatment was usually initiated from age 10 years (41.3%). A study conducted in Denmark of a cohort of children born between 1999 and 2001 found a mean age at treatment initiation of 11.9 years, with the prevalence of treatment peaking in the 10–13 years age group.14 This may be influenced by the fact that the adverse effects of methylphenidate are harder to tolerate for younger children29 and adherence to treatment is greater before age 13 years, when children depend more on their parents and are more compliant with parental decisions.30
Lastly, our data also revealed significant differences in the rate of utilisation between municipalities in the Region of Murcia. This suggests that there is a broad variability in the perception and awareness of problems associated with ADHD in parents, educators and physicians. Studies conducted in the United States31,32 and Switzerland13 have also found significant differences between areas based on geographical location and socioeconomic level, with lower prevalences of treatment in rural and semi-rural areas associated with a decreased accessibility of care, even in instances when there was a relatively high prevalence of ADHD diagnosis.31 Our data reflected higher utilisation in urban areas, especially in the adolescent population (15–19 years).
There are some limitations to our study that must be taken into account and which are characteristic of drug utilisation studies. Chief among them is the fact that there is no register of clinical diagnoses, although the only indication for which methylphenidate and atomoxetine are authorised in Spain is ADHD. On the other hand, we only considered one DDD per active principle, when the dosage may vary depending on the indication for treatment and the age of the patient. A correction of these parameters would lead to decreases in the DDIs values found in our study. Although throughout this article we have been using the terms “utilization” and “consumption,” what the study actually measured was drug dispensing. Despite these limitations, the study contributes information that may be useful to improve our understanding of the use of these drugs in Spain.
It is fair to conclude that there has been a substantial increase in the use of pharmacological treatment for ADHD in children and adolescents in the Region of Murcia, with greater utilisation in male compared to female patients, although overall the consumption of ADHD drugs was lower compared to that reported for other autonomous communities in Spain or to neighbouring countries. We found significant variations between geographical areas, with the highest utilisation in adolescents residing in urban areas.
Conflicts of interestThe authors have no conflicts of interest to declare. Diego P. Sánchez, pharmacist and owner of the La Ñora community pharmacy, declares having no association with the laboratories that distribute the medicines included in this study.
We thank the uncredited individuals who reviewed the manuscript for their corrections and suggestions, which have undoubtedly improved the final work. We also thank the Official Board of Pharmacists of the Region of Murcia for its help and collaboration in the collection of the data needed for the study.
Please cite this article as: Sánchez Martínez DP, Guillén Pérez JJ. Epidemiología del tratamiento farmacológico del trastorno por déficit de atención e hiperactividad (TDAH) en la Región de Murcia: diferencias por sexo, edad y lugar de residencia. An Pediatr (Barc). 2018;88:183–190.