In neonatal units, umbilical vessel catheterization is the preferred method to gain vascular access in the initial management of the newborn because it is quick and easy.
The failure rate ranges from to 50%, as the catheter can be found in the portal system in up to 40% of cases, leading to complications. This failure rate warrants the investigation of different methods to reduce the frequency of catheter malposition. We describe different techniques to improve the success rate in umbilical vein catheterization, such as the double catheter technique, positioning the newborn in right lateral decubitus for insertion, liver compression, and ultrasound-guided catheter insertion. The primary objective of the study was to assess the impact of new techniques on the success rate of central umbilical venous catheterization.
Material and methodsPre- and post-intervention quasi-experimental study in a level B NICU conducted in January-June 2022 (pre-intervention) and July-December 2022 (post-intervention).
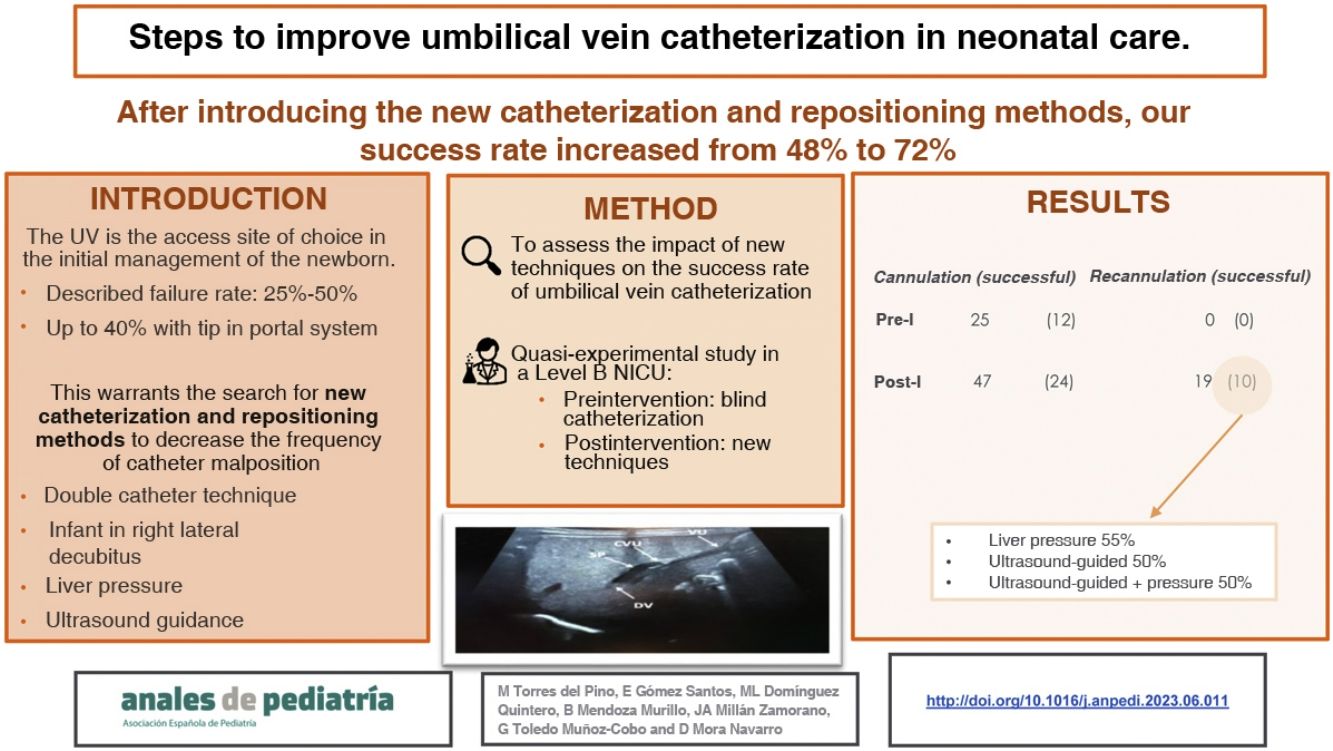
ResultsPrior to the introduction of these new catheterization techniques, the failure rate of blind umbilical catheter insertion was 52%. Since the introduction of these measures, the overall failure rate has decreased to 27%.
ConclusionsAfter the introduction of the new catheterization and recanalization methods, our success rate in umbilical vein catheterization has increased, and we believe it is necessary to implement them in units with similar failure rates to ours.
En las unidades neonatales se utiliza el catéter venoso umbilical como acceso vascular de elección en la atención inicial del recién nacido debido a su rápido y fácil acceso. Presenta una tasa de fracaso del 25% al 50%, ya que hasta en un 40% de los casos puede encontrarse en el sistema portal conllevando complicaciones. Esto justifica la búsqueda de métodos para disminuir la tasa de catéteres mal posicionados. Se describen diferentes técnicas para mejorar la tasa de éxito a la hora de canalizar la vena umbilical, como son la técnica del doble catéter, la posición del recién nacido para canalizar en decúbito lateral derecho, la compresión hepática y la canalización de forma ecoguiada. El objetivo principal de este estudio es evaluar el impacto de las nuevas técnicas en la tasa de éxito de canalización venosa umbilical central.
Material y métodosEstudio cuasi-experimental pre y post intervención en una UCIN nivel B durante Enero-Junio 2022 (preintervención) y Julio-Diciembre 2022 (postintervención).
ResultadosPrevio a la introducción de estas nuevas técnicas de canalización nuestra tasa de fracaso en la canalización, siempre llevada a cabo a ciegas, era de un 52% y con la introducción de estas medidas ha disminuido la tasa de fracaso a un 27% de forma global.
ConclusionesTras la introducción de los nuevos métodos de canalización y recanalización, nuestra tasa de éxito en la canalización de la vena umbilical ha aumentado, y creemos necesario implantarlo en unidades con tasas de fracaso similares a la nuestra.
Vascular catheterization is one of the most common procedures in everyday clinical practice in hospitals and is not free of complications.1 Ultrasound-guided central vein catheterization has been widely used in adults and subsequently in children, and in recent years it has been found to be very useful in young infants and newborns.2,3
Thus, the international evidence-based guidelines on point of care ultrasound (POCUS) of 2020 and the Cochrane review on the subject of 2015 recommend POCUS-guided technique for inner jugular vein line placement in neonates and children with a quality of evidence A.4,5 Oulego-Erroz et al. recommended ultrasound-guided subclavian and brachiocephalic venous line placement in children and neonates, associated with a greater success rate with fewer needle passes.6
The umbilical vein is the vascular access site of choice in the initial management of the newborn. The reported failure rate of blind umbilical vein line placement ranges from 25% to 50%, and this technique, contrary to line placement at other central access sites, has not been modified for decades.7,8
A correctly placed umbilical catheter is inserted through the umbilical vein, traversing the portal sinus to the ductus venosus, with confirmation of the central position by visualization of the tip at the inferior cavoatrial junction.7
During insertion, the catheter may migrate towards the left portal vein, right portal vein, splenic vein or, less frequently, the mesenteric vein.
Malposition with progression of the catheter into the portal system may take place in up to 40% of patients, and this position (subhepatic) can cause severe complications such as portal vein thrombosis, portal hypertension and portal cavernoma formation, abscess, ascites, cardiac tamponade and hepatic necrosis due to the hyperosmolality of infused solutes.7–9
Thus, in 2006, Morag et al. described a series of 133 children with portal vein thrombosis, of who 45 (34%) had a history of umbilical catheter in situ.
This warrants the search for methods that could improve the success rate in terms of achieving the central position in umbilical vein catheterization.9
One such method is the double catheter technique. It is based on the notion that the first (malpositioned) catheter followed the path of least resistance, entering one of the vessels in the portal system. The second catheter would bypass the area of misdirection, already occupied by the first catheter, and enter the inferior vena cava. The reported success rate was 50%, and the only described complication was bleeding during the removal of the malpositioned catheter, which was easily controlled.10
Another strategy is placing the infant lying on the right side. The rationale is that this position would pull the right lobe of the liver downward, increasing the external pressure on the portal vein and reducing the pressure on the ductus venosus, making it easier for the catheter to pass through the latter into the inferior vena cava. A study conducted by Kieran et al. did not find an increase in the success rate with this technique, although the authors noted that a larger sample may have supported this hypothesis. The technique was well tolerated and the position did not increase the difficulty of inserting the catheter.11
A third technique involves manual mobilization of the liver and is based on anatomical reasoning. Applying pressure over the liver to push it downwards shifts the portal sinus and improves the angle of the umbilical vein in relation to the ductus venosus, creating a flatter and straighter trajectory. It also compresses the opening into the left portal vein and reduces the angle of the caudal turn from the portal sinus to the right portal vein, making it less accessible.9 It is important to avoid applying excessive pressure, which could occlude the entry to the ductus venosus, and it may be necessary to inject a small volume of saline through the catheter to dilate it temporarily and facilitate its passage. This reduced the failure rate by 52%.9
Last of all, we discuss real-time ultrasound guided catheterization. The most recent guideline of the European Society of Paediatric and Neonatal Intensive Care on the subject recommends the use of POCUS to guide catheterization of the femoral vein, jugular vein and others, and also to assess the position of the catheter tip.4 However, the application of POCUS to umbilical vein catheterization is a novel and emerging technique that entails significant progress in this essential neonatal procedure.7
Using the liver as an acoustic window, the relevant anatomy may be visualised with the transducer (sector array or linear array) approximately at the midline, below the xyphoid and facing the head longitudinally, finding the territory of the umbilical and portal veins (Fig. 1).
The reported success rate is of 93%, with no complications.8
We present a study conducted after the introduction of a stepwise protocol aimed at improving the success rate of umbilical vein catheterization.
Material and methodsOur primary objective as to assess the impact of novel techniques in the success rate of umbilical vein catheterization over a 12-month period.
The secondary objectives were to describe the epidemiological and clinical characteristics of the patients, identify the recanalization technique used most frequently in our hospital and the technique with the highest success rate and describe the potential complications associated with malpositioned central lines.
Design: quasi-experimental pre- and postintervention study conducted in a level B neonatal intensive care unit (NICU) (not offering neonatal surgical care).
Participants: all newborns who required umbilical vein catheterization for any reason between January and June 2022 (preintervention) and between July and December 2022 (postintervention). The sole exclusion criterion was the refusal of the parents or legal guardians to consent to participation.
Description of the intervention or improvement planFirst we made a retrospective descriptive analysis of the failure and success rates in our unit of blind catheterization in the 6 months preceding initiation of the study, which were of 50%. We also conducted a literature review to improve the umbilical vein catheterization success rate by 50% in patients with a malpositioned catheter.
After this, we developed a protocol that was introduced in a clinical meeting, held twice, attended by 100% of the staff. In this presentation, we described the different techniques for umbilical vein catheter insertion and repositioning and proposed 2 hypothetical practical scenarios to illustrate how to select one technique over another, although ultimately the final decision always rests with the paediatrician in charge.
First clinical scenario: newborn that is severely ill or high workload situation (such as a night or weekend shift). If during a blind attempt to insert a catheter in the umbilical vein the catheter seems stuck or the blood does not flow back and migration to the portal territory is suspected, the catheter should be pulled back 3 cm. Then, the liver should be mobilised by pressing the upper abdomen down a depth of 1 cm and reinsertion attempted. The paediatrician could also choose to place the patient in the right lateral decubitus position for catheter reinsertion or use the double catheter technique.
Second clinical scenario: morning shift in which several paediatricians are onsite and/or the patient is not severely ill. We propose ultrasound-guided catheter insertion with sterile technique, which requires 2 experienced staff. If it is considered beneficial, it is possible to combine ultrasound-guided catheterization with the abdominal pressure strategy.
If the catheter cannot be repositioned successfully despite the implementation of the new techniques, we recommend removal from the portal system due to the risk of complications, and propose securing the catheters 2–3 cm back in preterm newborns and 4–5 cm back in term newborns, as long as hyperosmotic substances are not infused.9,12
Study variables: the primary outcome was the frequency of successful umbilical vein catheterization, defined as verification of the catheter tip position at the junction of the inferior vena cava and the right atrium by plain radiography or POCUS. Other variables under study were: sex, gestational age (weeks), birth weight (g), reason for umbilical vein catheterization, time at which the catheter was inserted (hours post birth), catheter position, duration of catheterization (days), catheter repositioning and method used for it, method used to assess the position of the catheter (ultrasound or plain chest radiograph).
Data collectionIn the first 6 months, we collected data on the variables of interest in children who underwent blind umbilical vein catheterization.
Later on, we collected data for all patients who underwent umbilical vein catheterization following the introduction of the new catheter repositioning methods and assessed whether their implementation had improved the success rate in our unit.
We developed a patient information sheet and informed consent form for the parents or legal guardians, and the study was approved by the Ethics Committee with the code 1463-N-22.
Data analysisWe entered the data in an Excel spreadsheet and performed the statistical analysis with the software package SPSS, version 21. We carried out a descriptive analysis, expressing categorical data as absolute and relative frequencies and continuous data as mean or median depending on their distribution. To assess the impact of the newly introduced catheterization techniques, we compared groups by means of the Student t-test or Mann-Whitney U test in the case of quantitative variables and the χ2 test in the case of qualitative variables. We considered P values of less than 0.05 statistically significant.
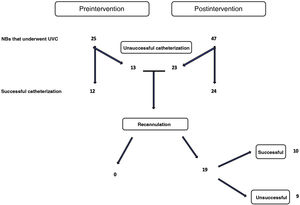
ResultsDuring the study period, we included 72 children, 25 in the preintervention group and 47 in the postintervention group (Fig. 2).
When it came to their clinical and epidemiological characteristics, there were no significant differences between the two periods (Table 1).
Epidemiological and clinical characteristics by group.
| Variable | PreinterventionN = 25 | PostinterventionN = 47 | P |
|---|---|---|---|
| Male, n (%) | 15 (60) | 28 (60) | NS |
| Female, n (%) | 10 (40) | 19 (40) | NS |
| GA (weeks), mean (SD) | 32 (5.7) | 33 (5) | NS |
| Weight (g), mean (SD) | 2189 (1282) | 2206 (1087) | NS |
| Time of catheterization (hours post birth), median (IQR) | 1 | 1 | NS |
| Indwelling time (days), mean (SD) | 3 (2) | 3.4 (2.3)) | NS |
| Reason for catheterization, n (%) | |||
| Prematurity | 14 (56) | 21 (44) | |
| HIE | 4 (16) | 5 (11) | NS |
| Sepsis | 2 (8) | 1 (2) | |
| Neonatal seizures | 0 | 1 (2) | |
| Hypoglycaemia | 0 | 2 (4) | |
| RD | 3 (12) | 5 (11) | |
| Heart disease | 0 | 1 (2) | |
| Sedation/analgesia | 0 | 1 (2) | |
| Anaemia/jaundice | 0 | 2 (4) | |
| Prematurity and RD | 1 (4) | 6 (13) | |
| HIE and RD | 0 | 2 (4) | |
| Prematurity and hypoglycaemia | 1 (4) | 0 | |
HIE, hypoxic-ischaemic encephalopathy; IQR, interquartile range; NS, not significant; RD, respiratory distress; SD, standard deviation.
We did not identify complications such as portal vein thrombosis, abscesses, ascites or necrosis in either period.
The mean catheter indwelling time was of 3 days in the preintervention period compared to 3.5 days in the postintervention period.
The relative frequency of central venous catheterization did not differ between the preintervention and postintervention periods, with percentages of 48% and 51%, respectively. Table 2 presents the data on the catheter tip position, methods used for catheterization and methods used to assess the catheter tip position.
Comparative analysis in the periods before and after the introduction of the new techniques.
| Variable | PreinterventionN = 25 | PostinterventionN = 47 | P |
|---|---|---|---|
| Successful catheterization (central position), n (%) | 12 (48) | 24 (51) | NS |
| Location of catheter tip, n (%): | NS | ||
| Central position | 12 (48) | 24 (51) | |
| Right portal vein | 11 (44) | 14 (30) | |
| Left portal vein | 2 (8) | 3 (6) | |
| Portal vein, side not specified | 0 (0) | 6 (13) | |
| Catheterization method, n (%): | NS | ||
| Blind | 25 (100) | 22 (47) | |
| Manual liver mobilization (pressure) | 0 | 19 (40) | |
| Ultrasound-guided | 0 | 4 (8,5) | |
| Ultrasound-guided with liver pressure | 0 | 2 (4,5) | |
| Lying on the side | 0 | 0 | |
| Verification of catheter tip position, n (%) | <0.05 | ||
| Plain radiography | 24 (96) | 37 (78) | |
| Ultrasound | 0 | 0 | |
| Both | 1 (4) | 10 (22) |
NS, not significant.
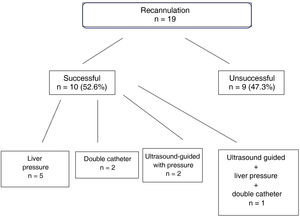
In the preintervention period, repositioning was not attempted in any case. However, in the postintervention period, out of the 23 patients in whom the first catheterization was unsuccessful, reinsertion was not attempted in 4 and attempted in 19, per the decision of the physician in charge. Of the 19 patients in whom it was attempted, repositioning was successful (catheter tip in the central position) in 10 (52%) and unsuccessful in 9, which increased the overall percentage of patients with successful umbilical vein catheterization to 72%.
The most successful catheter repositioning technique used in our unit was liver pressure (used in 5 cases), with an overall reinsertion success rate of 55%, followed by the double catheter technique (used in 2 children, successfully) and ultrasound-guided repositioning combined with liver pressure. Liver pressure followed by ultrasound-guided reinsertion with liver pressure was used in a single patient. The combination of different techniques (double catheter, liver pressure and ultrasound-guided) achieved a success rate of 50% (Fig. 3).
When it came to the assessment of the catheter tip position, following the introduction of these methods, the use of sonography besides radiography increased by 22%.
In 6 cases in the postintervention period (13%), the peripheral catheter was left in place, having attempted umbilical vein catheter repositioning, unsuccessfully, in only half of them.
DiscussionAlthough there is scientific evidence that supports the recommendation of ultrasound-guided catheterization of other vessels, such as the jugular or femoral veins,2–6 few studies contribute evidence in support of it use for umbilical vein catheterization.7,8
Unlike other studies that have reported success rates of up to 93%, in our study we did not find statistically significant differences in the first-attempt success rate between the groups. One possible explanation is that our unit is going through the learning curve for these new techniques, especially the use of POCUS to guide umbilical vein catheter placement.
Still, the new techniques succeeded in achieving correct reinsertion of 53% of the malpositioned catheters in the postintervention group. We believe that this reduced the use of material resources, saved time that would have been attempting catheterization at other access sites and, in addition, spared our neonatal patients the pain associated with invasive punctures, besides allowing earlier initiation of intravenous treatment.
The main benefit of our study is that the failure rate observed with blind catheter insertion, of 52%, decreased to 27% after the introduction of the new techniques.
The most frequently used technique was liver pressure, both for catheter reinsertion and initial insertion. Its salient qualities are that it is quick and easy to implement, does not require prior experience and is particularly appropriate for catheterization in extremely preterm or severely ill infants. The success rate in our sample was high, of 52.6% for initial catheter insertion and 55.5% for catheter reinsertion, and there were no associated complications, in agreement with the previous literature.9
The double catheter technique was used sparingly and only for repositioning. In our case, it was only used in 2 cases, successfully in both, with no associated complications.10 The approach of placing the patient in the right lateral decubitus position was not used in any instance because the literature to date has not described an increased success rate, because help from an additional staff member would be required to hold the child in the position and because the position itself could be poorly tolerated, although Kieran et al. reported that the position was well tolerated and did not increase the difficulty of inserting the catheter.11
As for the use of ultrasound, umbilical vein catheterization was guided by ultrasound in 6 instances, combined with liver pressure in 2, and this approach was successful in 50% of cases. It was used for catheter reinsertion 5 times, also with a 50% success rate. Although this technique requires at least 2 qualified staff members, frequent use of it could shorten the duration of the procedure and would allow performance of it in more severely ill and premature infants, always making sure to take the precaution of warming up the ultrasound gel. At the moment, it is a novel and emerging technique for the catheterization of umbilical vessels, and it is a significant advance in this basic neonatal procedure that we believe must be known to the largest possible number of physicians.
Another strength of our study is that we succeeded in reducing the amount of radiation that our patients were exposed to, as the initial suspicion that the catheter was malpositioned was based on clinical features and in most cases the catheter was reinserted without prior performance of a radiograph. We have also started to use sonography to assess the position of the catheter tip in addition to plain radiography, and we may eventually stop using radiography for this purpose altogether. Last of all, another positive aspect is that, as a result of the review, we have emphasised the need to remove malpositioned catheters from the portal system in our unit, on account of the risk of complications.9,12
One of the limitations of the study is that it had a quasi-experimental design and there was no simultaneous control group to compare the effects of the intervention with, which may limit the extrapolation of the results.
Another limitation is that despite the new techniques and the two hypothetical clinical scenarios presented and proposed at the beginning of the study, both the technique chosen for umbilical vein catheterization and the decision to attempt reinsertion in the case of malposition were left to the judgment of the physician in charge of the patient at the given time. As a result, reinsertion was not attempted in every instance that the catheter was not inserted correctly.
Thus, although the use of new techniques in our sample was not associated with an increased first-attempt success rate, it did increase the success rate of catheter reinsertion. Therefore, we believe it could be beneficial for neonatal units with failure rates similar to those of our unit to implement the measure bundle we applied or a similar one to increase their success rate.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.