An 11-year-old male, under study with a 2-month history of constitutional syndrome, presented with vomiting, epigastric pain and constipation. The most salient features of the history were ocular (conjunctival hyperemia), articular (joint pain and nonspecific limp) and cutaneous (Fig. 1).
These lesions were also found on the trunk, upper extremities, hands and feet with a 2 month evolution prior, with recent appearance of erythematous papules. The histological examination of the cutaneous lesions evinced deposition of hyaline material (periodic acid Schiff positive and diastase resistant [PAS-D]) in the vascular walls with mild perivascular inflammatory lymphohistiocytic infiltration and signs of red blood cell extravasation. The epidermal crests exhibited marked atrophy. In the dermis, there was a triangular area in the centre, with the base in the superior dermis, characterised by homogeneous collagen necrosis. Some deep blood vessels appeared to have thickened walls and occluded lumina.
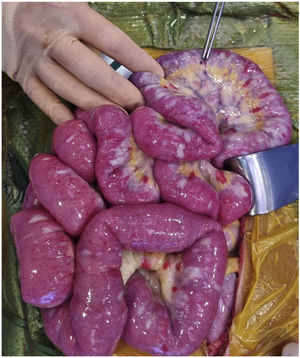
Initially, a bezoar was suspected and studied. However, after 48 hours of evolution, the patient deteriorated abruptly, developing fever, vomiting, acute abdominal pain and general malaise. An emergency abdominal-pelvic computed tomography was performed, which showed intestinal perforation. He required surgical resection and the creation of a discharge ileostomy and parenteral nutrition.
Kohlmeier-Degos disease is a rare disease of unknown aetiology, with less than 200 cases reported worldwide.1 It is characterized by a multisystemic small-vessel lymphocytic vasculitis of the small-calibre vessels that can affect the skin, gastrointestinal tract, central nervous system, eyes, lungs, cardiovascular system and the renal system.2 Gastrointestinal manifestations usually appears to develop months or years after cutaneous manifestations and they are associated with a poor prognosis. Gastrointestinal involvement may be asymptomatic or cause dysphagia, vomiting, haematemesis, melena and intestinal perforation with peritonitis.3 Neurologic involvement manifests with multiple strokes. The diagnosis is based on the cutaneous manifestations and histological features. The papules measuring 0.5–1 cm with a porcelain-white atrophic centre and an erythematous telangiectatic rim, are characteristic of the disease. They appear in the trunk and upper and lower extremities, and usually sparing the face, scalp, palms and soles.1 No effective treatment has been found to date. Some of the treatments used in its management include anticoagulants, antiplatelets, fibrinolytics, immunosuppressants, steroids, eculizumab and Janus kinase inhibitors, with little success once the systemic disease appears.3
Knowledge of the cutaneous lesions can facilitate suspicion of this devastating disease.
FundingThis research did not receive any external funding.