Despite lack of proven effectiveness and its potential to cause severe burns, steam inhalation therapy (SIT) is still used as a treatment for benign respiratory conditions.
ObjectiveTo characterise cases of burns related to steam inhalation therapy (BRSIT) in order to formulate appropriate preventive criteria.
Patients and methodsA review was conducted on cases of BRSIT admitted to a Burns Unit between 2006 and 2012, analysing epidemiological data, clinical aspects, severity and course.
ResultsA total of 530 patients were admitted; 375 (70%) with scalds, and 15 with BRSIT (2.8% of burns; 4% of scalds). SIT was indicated in most cases for mild upper airway infections. The median age of patients was 7 years (2.5m-14y). The burned area (BA) was ≥10% in 60% of cases (max. BA 22%). Injuries involved trunk, genital area, and extremities; only in one case was the face affected. The mean hospital length-of-stay was 14 days (3-30d). Five patients (33%) were admitted to the PICU, most of them (60%) younger than 3 years. Eight patients (53%) underwent surgical treatment (skin grafting). In a 12-year-old patient whooping cough was diagnosed in the Burns Unit, and a 2.5-year-old patient developed staphylococcal toxic shock syndrome. No patient died. The final course was satisfactory in all patients.
ConclusionsBRSIT can be severe and cause significant use of health resources. Professionals caring for children, particularly paediatricians, should seriously consider their prevention, avoiding treatments with SIT, and educating parents in order not to use it on their own.
Todavía se emplean vahos con agua caliente como tratamiento de procesos respiratorios banales, a pesar del riesgo de ocasionar quemaduras y de no haberse demostrado su efectividad.
ObjetivosCaracterizar los casos de quemaduras relacionadas con vahos (QRV) en una población de niños quemados con el objeto de formular criterios para su prevención.
Pacientes y métodosRevisión de pacientes ingresados por QRV en una unidad de quemados durante el periodo 2006-2012. Se analizó: epidemiología, clínica, gravedad y evolución.
ResultadosIngresaron 530 pacientes quemados; 375 (70%) con escaldaduras y 15 con QRV (2,8% del total; 4% de las escaldaduras). Los vahos fueron indicados mayoritariamente para tratar episodios catarrales banales. La edad mediana fue 7 años (2,5 meses-14 años). La superficie corporal quemada (SCQ) fue ≥10% en el 60% de los casos (SCQ máxima 22%). Las quemaduras afectaron al tronco, a los genitales y a las extremidades y solo en un caso afectó a la cara. La estancia media hospitalaria fue de 14 días (3-30d). Cinco niños (33%) ingresaron en la UCIP, la mayoría (60%) menores de 3 años. Ocho casos (53%) requirieron intervención quirúrgica (injerto de piel). Un paciente de 12 años fue diagnosticado de tos ferina y otro de 2,5 años presentó un shock tóxico estafilocócico. No hubo fallecimientos. Todos los pacientes evolucionaron satisfactoriamente.
ConclusionesLas QRV pueden ser graves y consumir importantes recursos. Los profesionales de la atención al niño, particularmente los pediatras, deben velar por su prevención, absteniéndose de indicar los vahos como tratamiento y educando a los padres para que no los utilicen por sí mismos.
Scalds are the most frequent cause of burns in childhood, especially between the ages of 1 and 3 years, when children become more independent but are little aware of the dangers around them. Scalds usually occur in the home in the process of meal and infusion preparation.1 As happens with other types of burns2, warnings are important for their potential prevention, and may even have legal repercussions. This is the case of several states in the USA, where warnings about tap water scalds have led to various laws establishing a maximum temperature of 49°C for hot tap water (1983 Washington State Law).3
On the other hand, steam inhalation therapy (SIT), which has been used traditionally and is still employed today to treat mild respiratory tract infections despite the lack of evidence to support its effectiveness, can also cause burns indirectly through scalding.
The aim of this study was to describe the patients admitted to our hospital with hot water burns related to steam inhalation therapy, determining the incidence and severity of such injuries, paying special attention to factors that may be useful in establishing criteria to prevent such burns.
Patients and methodsWe performed a retrospective descriptive study by reviewing the cases of patients admitted to the burns unit of the Hospital Universitario Vall d’Hebron of Barcelona (UQVH; the burns referral unit for the region of Catalonia and the Balearic Islands) from January 1, 2006 to December 31, 2012. The population under study consisted of paediatric patients (age <16 years) admitted to the UQVH with burns related to steam inhalation therapy (BRSIT). We analysed factors relating to the causative mechanism, the signs and symptoms, the severity of the injuries and the outcome of patients. The burns considered severe, based on depth and extent, were partial-thickness burns (second degree) covering 10% or more of the total body surface area (or ≥15% in children aged 10 years or older) and full-thickness burns (third degree) covering 5% or more of the total body surface area (all ages).4 The study was approved by the ethics and clinical research committee of the Hospital Universitario Vall d’Hebron.
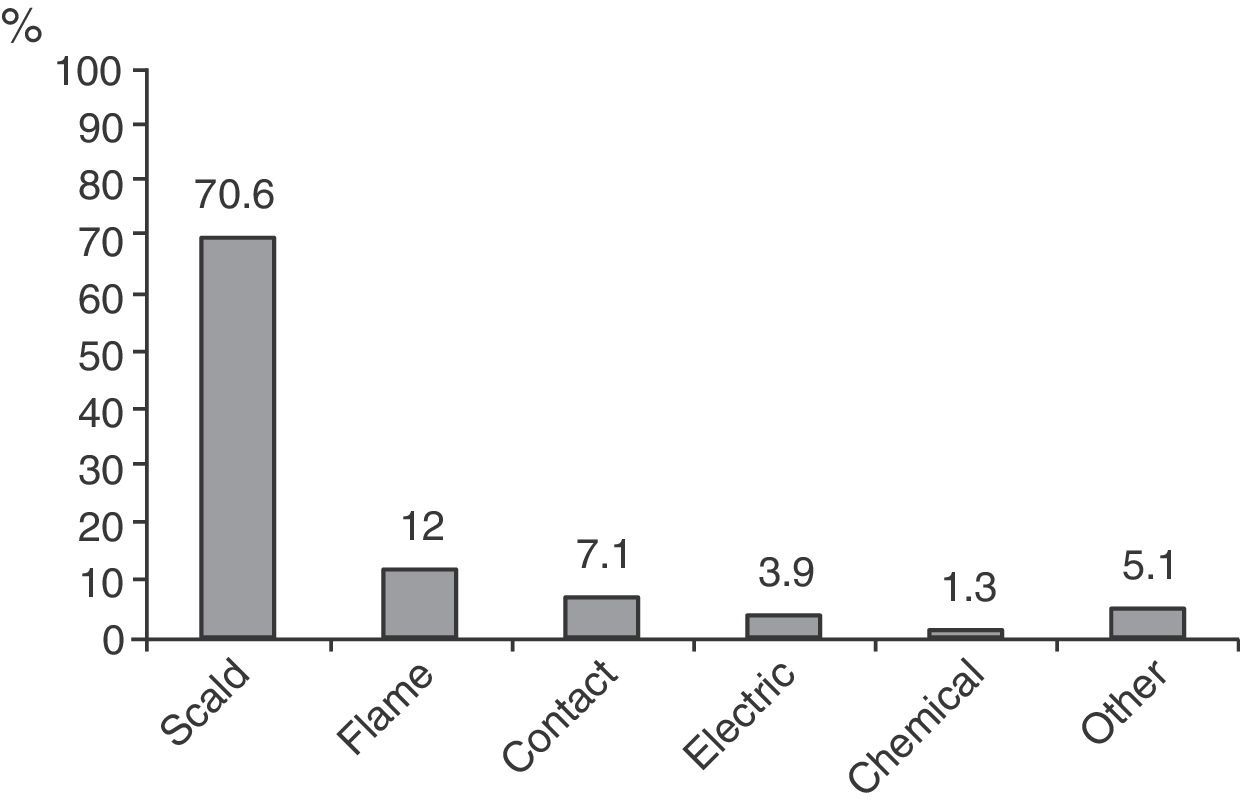
ResultsIn the period under study 530 burnt patients were admitted to the UQVH, of which 375 (70%) presented with scalds and 15 with BRSIT. The contribution of different aetiological mechanisms is described in Figure 1, which shows that scalds are the most frequent cause of burns in children. BRSIT accounted for 4% of the scalds and 2.8% of all burns.
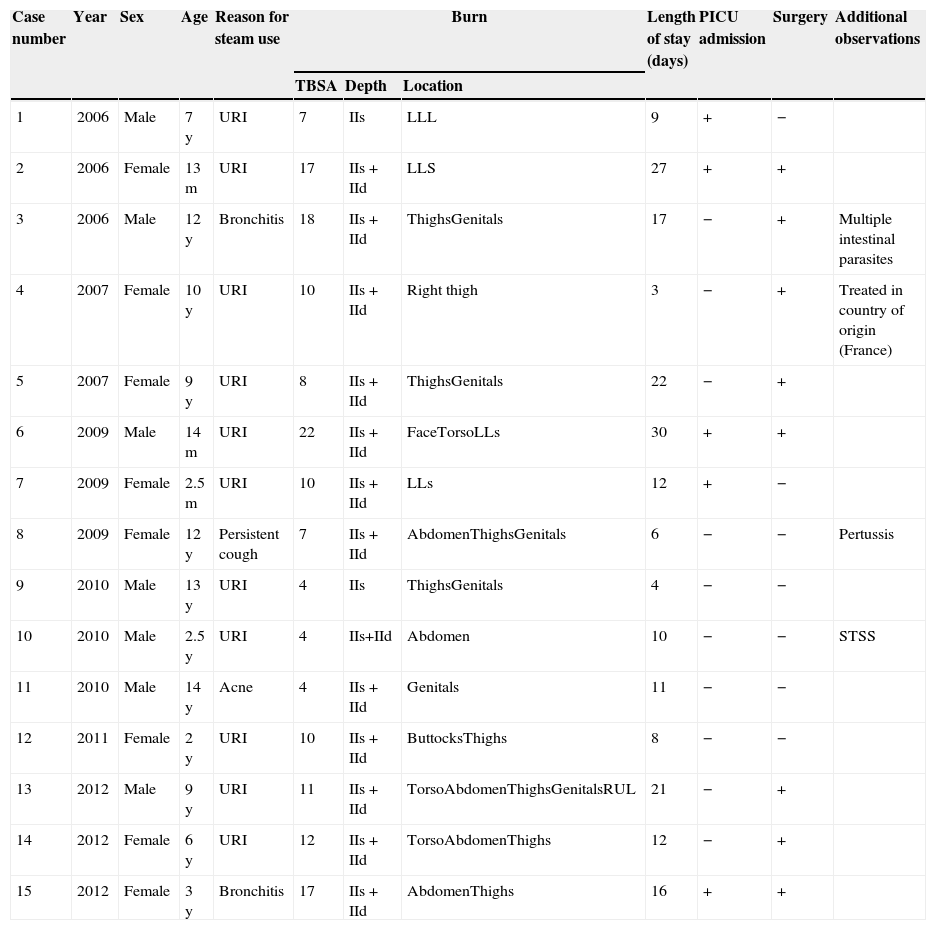
Table 1 shows the key data concerning the causes of BRSIT.
Paediatric patients hospitalised due to steam inhalation burns (2006–2012). Clinical and evolution features.
| Case number | Year | Sex | Age | Reason for steam use | Burn | Length of stay (days) | PICU admission | Surgery | Additional observations | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| TBSA | Depth | Location | |||||||||
| 1 | 2006 | Male | 7 y | URI | 7 | IIs | LLL | 9 | + | − | |
| 2 | 2006 | Female | 13 m | URI | 17 | IIs+IId | LLS | 27 | + | + | |
| 3 | 2006 | Male | 12 y | Bronchitis | 18 | IIs+IId | ThighsGenitals | 17 | − | + | Multiple intestinal parasites |
| 4 | 2007 | Female | 10 y | URI | 10 | IIs+IId | Right thigh | 3 | − | + | Treated in country of origin (France) |
| 5 | 2007 | Female | 9 y | URI | 8 | IIs+IId | ThighsGenitals | 22 | − | + | |
| 6 | 2009 | Male | 14 m | URI | 22 | IIs+IId | FaceTorsoLLs | 30 | + | + | |
| 7 | 2009 | Female | 2.5 m | URI | 10 | IIs+IId | LLs | 12 | + | − | |
| 8 | 2009 | Female | 12 y | Persistent cough | 7 | IIs+IId | AbdomenThighsGenitals | 6 | − | − | Pertussis |
| 9 | 2010 | Male | 13 y | URI | 4 | IIs | ThighsGenitals | 4 | − | − | |
| 10 | 2010 | Male | 2.5 y | URI | 4 | IIs+IId | Abdomen | 10 | − | − | STSS |
| 11 | 2010 | Male | 14 y | Acne | 4 | IIs+IId | Genitals | 11 | − | − | |
| 12 | 2011 | Female | 2 y | URI | 10 | IIs+IId | ButtocksThighs | 8 | − | − | |
| 13 | 2012 | Male | 9 y | URI | 11 | IIs+IId | TorsoAbdomenThighsGenitalsRUL | 21 | − | + | |
| 14 | 2012 | Female | 6 y | URI | 12 | IIs+IId | TorsoAbdomenThighs | 12 | − | + | |
| 15 | 2012 | Female | 3 y | Bronchitis | 17 | IIs+IId | AbdomenThighs | 16 | + | + | |
Patients numbered in chronological order.
TBSA, total body surface area (% area burned); IId, deep partial-thickness (second degree) burn; IIs, superficial partial-thickness (second degree) burn; LLL, left lower limb; LLs, lower limbs; PICU, paediatric intensive care unit; RUL, right upper limb; STSS, staphylococcal toxic shock syndrome; URI, upper respiratory infection.
All the patients included presented with scalds. Most incidents were related to the treatment of upper respiratory tract infections (colds). In children younger than 9 years, the burn usually resulted from the child tripping on the container. In older children injuries were facilitated by covering the container with a towel with the purpose of intensifying the effects of the steam.
In our series, the injuries were evenly distributed between both sexes (8 girls and 7 boys). The mean age was 7 years (2.5 months–14 years) and 33% of the patients were younger than 3 years. The mean total body surface area burned (TBSA) was 11% (4–22%), and the TBSA was equal to or greater than 10% in 60% of the patients. Eighty percent of the patients younger than 3 years had severe burns. The burns involved the torso, genital area, and limbs, with involvement of the face in only one patient (case 6). The mean length of stay was 14 days (3–30days). Five children (33%) were admitted to the PICU, and most of them (60%) were younger than 3 years. Eight patients (53%) required surgery (skin grafting). One 12-year-old girl was diagnosed with pertussis at admission (case 8), and one boy aged 2.5 years developed staphylococcal toxic shock syndrome (case 10). There were no deaths and the final outcome was favourable in all patients.
DiscussionThe data we present for this series of 15 paediatric patients confirm that SIT is associated with incurring potentially severe burns in children, especially in the youngest age group (age <3 years). Furthermore, these burns can result in complications such as staphylococcal toxic shock syndrome, as seen in case 10. This complication develops most commonly in patients aged between 6 months and 3 years, who are less likely to produce the antibody to staphylococcal toxin TSST-1, and is currently considered the main cause of mortality in mild burn cases.5 On the other hand, the respiratory symptoms of children admitted for BRSIT require additional care and may worsen or lead to complications during hospitalisation, demanding significant adjustments of the treatment plans. This happened in the patient diagnosed with pertussis (case 8), who required the implementation of specific preventive and isolation measures.
Several publications have addressed this type of burns in children. The study performed by Wallis et al.6 reviewed the cases of 27 children treated between 2001 and 2006. The children were 7 months to 14 years of age, and 44% were younger than 3 years. More severe burns were observed in children younger than 3 years, as happened in our study. It is worth noting that 75% of the injuries in the study occurred while the children were under parental supervision, a factor that was not evaluated in our study. The authors also mentioned direct contact with commercial vaporiser units or the jet of steam that they emit (10 patients) as an additional injury mechanism that was not observed in our case series. Another study by Murphy et al.7 discussed the risks of SIT and the scarcity of evidence supporting its beneficial effect on the course of respiratory illness. These authors presented data for 7 patients aged between 9 months and 10 years treated over a 6-month period for BRSIT involving a TBSA of 3–6% (one of whom required a skin graft), who in their study accounted for 9% of all paediatric admissions for burns.
It is apparent that regardless of how SIT is applied it carries a risk of burn injury. The usual technique of covering the head with a towel over a pan filled with hot water is dangerous due to the steam, the hot liquid, or even potential contact with the container. On the other hand, transporting or placing hot water near a child carries a considerable risk of burn injury, which is greater when the child is younger (especially in children younger than 3 years of age), as the data in our study seem to corroborate.
An important aspect to consider in BRSIT is that in many cases the use of steam had been recommended by health professionals to treat mild upper respiratory tract infections, or less frequently to treat other respiratory or non-respiratory conditions as observed in the study by Murphy et al.7 (2 cases). Although data concerning this factor were not collected systematically in our study, we found documentation that SIT was prescribed at the UQVH to the patient diagnosed with pertussis to treat a persistent cough lasting 10 days, and also to the patient corresponding to case 11 for the treatment of acne.
The risk of burn injury associated with SIT is compounded by the lack of evidence supporting its benefits, which results in an unfavourable cost-benefit ratio. A Cochrane review8 of 6 clinical trials showed that intranasal steam inhalation provided symptom relief, but the results were equivocal when it came to nasal congestion. The review also found no improvement in objective measures of disease like secretion viral loads or viral titres from nasal washings. Clinical trials studying the use of SIT in the treatment of croup did not show any benefits either. The authors of the review concluded that the use of SIT should be discouraged.
This study only included cases that required admission, leaving out all mild injuries that were treated in outpatient services or outside the UQVH, which could be considered a limitation. Nevertheless, we believe that this case series included a significant number of patients (15 patients, somewhere between the 7 patients in the Murphy series7 and the 27 of the Wallis series6) and that the data it provides are clear and can be interpreted as a warning sign.
To conclude, it is apparent that steam therapy, usually applied by means of containers filled with hot water, brings no benefit and can also cause severe indirect burns. We believe that health professionals who deliver care to children, especially paediatricians, must strive to prevent these burns by refraining from recommending this type of therapy, and educating parents not to apply steam therapy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Belmonte JA, Domínguez-Sampedro P, Pérez E, Suelves JM, Collado JM. Quemaduras graves relacionadas con la terapia inhalatoria con vahos. Anales de Pediatría. 2015;82:95–99.
The content of this work has been presented in preliminary form of communication poster in the eighteenth Annual Meeting of the Societat Catalana of Pediatrics (Figueres, Girona, May 2012).