Classic autoimmune hepatitis (AIH) is a progressive and chronic form of hepatitis of unknown aetiology characterised by an immune response that targets hepatocytes. It is diagnosed based on laboratory findings (elevated aminotransferase levels, hypergammaglobulinaemia and presence of antibodies) and compatible findings of liver biopsy: interface hepatitis, plasma cell infiltrate, rosette formation (microacinar transformation of hepatocytes) and/or fibrosis, necrosis and cirrhosis.
In recent years, a new form of disease has been described, seronegative AIH, on which few data have been published in the paediatric literature.1,2 It is similar to classic AIH, but is characterised by the absence of antibodies and may present in association with other autoimmune diseases.2,3 It manifests with clinical and biochemical signs of chronic hepatitis in the absence of features indicative of other aetiologies (infectious, metabolic, toxic, etc.). Blood tests usually reveal elevated transaminase levels and absence of antibodies, with additional absence of hypergammaglobulinaemia in up to 25% of cases. Liver biopsy reveals features compatible with AIH, and affected patients respond well to immunosuppressive therapy, as do patients with classic AIH.4,5
Considering this newly described form, we reviewed 2 cases of chronic hepatitis of unknown aetiology manifesting with fibrosis on liver biopsy managed in our paediatric gastroenterology clinic, with the purpose of determining whether they may fit the criteria for seronegative AIH.
The first case corresponded to a male patient aged 12 years referred to our clinic for investigation of persistent elevation of serum transaminases of 2 years’ duration (serum glutamic oxaloacetic transaminase [SGOT], 62–325IU/L; serum glutamic pyruvic transaminase [SGPT] 100–430IU/L) detected by chance during a routine blood test. The second corresponded to a female patient aged 6 years that had received a diagnosis of coeliac disease 3 years earlier; she had elevated serum transaminases before diagnosis that persisted in the follow-up blood tests (SGOT, 80–630IU/L; SGPT, 90–820IU/L) despite normalisation of serological markers of coeliac disease.
In both cases, the investigation of the elevation of serum transaminases failed to identify its aetiology: the chemistry and metabolic panels revealed normal iron metabolism, with negative serological markers of coeliac disease (in the second case, initially positive with normalisation after removal of gluten from the diet), absence of clotting abnormalities, normal thyroid function and normal immunoglobulin levels. The patients had no history of exposure to hepatotoxic drugs, and the investigation ruled out infection, classic AIH (due to negative antibody tests), alpha-1 antitrypsin deficiency, Wilson disease, lysosomal acid lipase deficiency and muscle and metabolic disorders. Both patients underwent repeated ultrasound examinations and a magnetic resonance cholangiography, the findings of which were normal. Given that all tests gave negative results while serum transaminases remained elevated, a liver biopsy sample was obtained for histopathological examination, resulting in a diagnosis of idiopathic liver fibrosis in both cases.
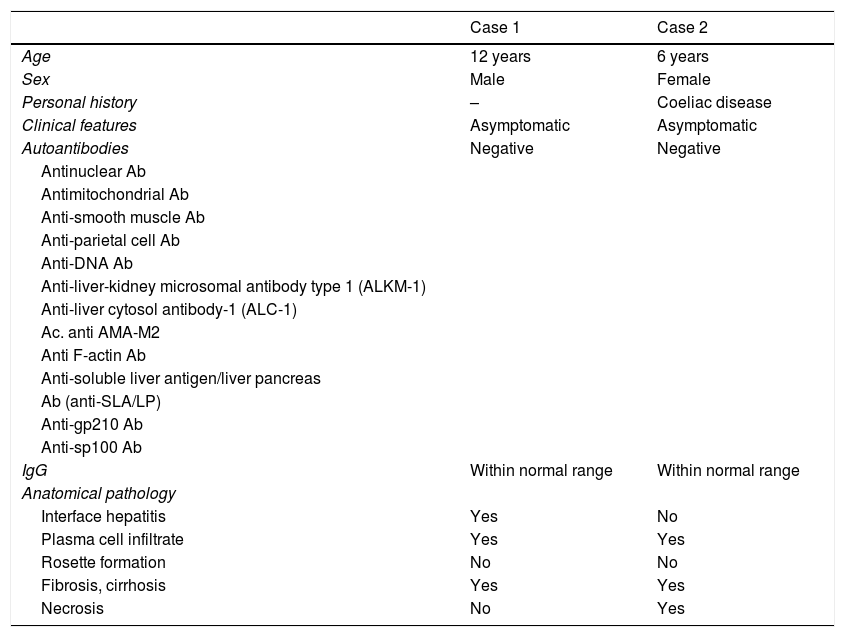
We contacted the anatomical pathology department and suggested the possibility of seronegative AIH, which led to performance of a targeted review of the histological features of both cases. The examination revealed cirrhosis and plasma cell infiltration, interface hepatitis in the first case, and necrosis in the second case. Rosettes were not found in either case. Based on these findings, the pathology report indicated that the cases were compatible with seronegative AIH. Table 1 summarises the anatomical pathology findings and the clinical characteristics of these 2 patients.
Clinical characteristics and histological features found in our 2 patients.
| Case 1 | Case 2 | |
|---|---|---|
| Age | 12 years | 6 years |
| Sex | Male | Female |
| Personal history | – | Coeliac disease |
| Clinical features | Asymptomatic | Asymptomatic |
| Autoantibodies | Negative | Negative |
| Antinuclear Ab | ||
| Antimitochondrial Ab | ||
| Anti-smooth muscle Ab | ||
| Anti-parietal cell Ab | ||
| Anti-DNA Ab | ||
| Anti-liver-kidney microsomal antibody type 1 (ALKM-1) | ||
| Anti-liver cytosol antibody-1 (ALC-1) | ||
| Ac. anti AMA-M2 | ||
| Anti F-actin Ab | ||
| Anti-soluble liver antigen/liver pancreas | ||
| Ab (anti-SLA/LP) | ||
| Anti-gp210 Ab | ||
| Anti-sp100 Ab | ||
| IgG | Within normal range | Within normal range |
| Anatomical pathology | ||
| Interface hepatitis | Yes | No |
| Plasma cell infiltrate | Yes | Yes |
| Rosette formation | No | No |
| Fibrosis, cirrhosis | Yes | Yes |
| Necrosis | No | Yes |
In light of the histopathological findings, and since other aetiologies had been ruled out previously, we proposed the diagnosis of seronegative AIH and, in agreement with the family, decided to initiate treatment in both patients with glucocorticoids at a dose of 2mg/kg/day to be tapered to a maintenance dose of 2.5mg every other day, with introduction of azathioprine on day 15 at a dose of 0.5mg/kg/day, increasing the dose gradually until reaching 2mg/kg/day.
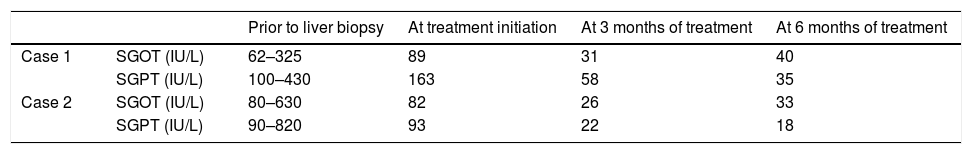
In both patients, the serum transaminase levels (SGOT and SGPT) had normalised at 3 months of treatment, and they remained within the normal range at 6 months with the patients receiving minimum doses of glucocorticoids. Table 2 shows the evolution of serum transaminase levels in the 2 patients.
In our experience, histological examination by a pathologist with a focus on seronegative AIH in two cases of unspecified fibrosis led to a new diagnosis and allowed effective treatment in both patients.
Seronegative AIH is a newly defined disease for which little data is available in the paediatric age group. At the moment, the possibility of an autoimmune aetiology should be considered in idiopathic cases of chronic hepatitis, especially in patients with a history of other autoimmune diseases such as coeliac disease,2,3 even if antibody detection tests are negative. We recommend performance of a liver biopsy in such cases and, should the results be compatible with autoimmune disease, early initiation of immunosuppressive therapy to halt the progression of liver disease.
Please cite this article as: Lahílla Cuello L, Ros Arnal I, García Romero R, Hörndler Argarate C. Hepatitis autoinmune seronegativa, descripción de 2 casos en edad pediátrica. An Pediatr (Barc). 2018;88:285–286.