Pectus carinatum is the second most common anterior chest wall deformity following pectus excavatum. In the past few decades, the mildest cases have been managed conservatively with dynamic compressive bracing, and various factors have been described in association with treatment outcomes.1,2 In our experience, poor results and abandonment are two common issues in the follow-up of these patients that contribute to treatment failure.
In order to describe the incidence of abandonment, the lack of correction and their possible association with epidemiological, clinical and motivational factors, we conducted a retrospective and descriptive study of the patients managed in our hospital over the 2018–2024 period. We analyzed (Student t test, χ2 test and multivariate analysis with the software SPSS, version 25) the characteristics of the deformity, the development of problems during brace therapy (skin problems, pain), the absence of deformity correction (initial correction pressure [IPS] > 2 for more than 6 months, lack of improvement in the deformity), mode of use (12 h a day, recommending overnight wearing), the season treatment was initiated and season it was abandoned for reasons related to the compression brace, as well as the level of motivation/discouragement and of satisfaction observed in the assessment conducted during trimestral clinical interviews.
We identified 24 patients (22 male and 2 female) with a median age of 13.5 years (12–15). Eight had pectus carinatum and16 chondrodysplasia. In the initial assessment, the mean surface area of the deformity was of 51.06 mm2 (SD, 12,09), the mean correction pressure was 5.37 pounds per square inch (PSI) (SD, 1.65) and the mean prescribed initial correction pressure was 2,34 PSI (SD, 0.52). The deformity was reduced in 79% (19/24) with a mean duration of treatment of 27.54 months (SD, 14,21). Signs of noncompliance were identified in 54% of the patients from the first trimester of treatment (lack of decrease in PSI, missing visits and/or manifest lack of motivation) with a mean duration of followup of 31.14 meses (±16,91). Nine patients (37%) completely abandoned therapy by a mean of 23.30 months of follow-up (SD, 12,06) and 4 exhibited partial noncompliance (17%) over 50.75 months (SD, 9.18). In the latter, adherence resumed after redefining the goals and expectations of treatment in the office. In the multivariate analysis, overnight use was the only factor that was significantly associated with the correction of the deformity (OR, 32; SE, 43; P < .05), adherence to treatment (OR, 26.21; SE, 43.94; P < .05) and shorter duration (difference of 23.68 months in the group with overnight brace use vs the group without overnight use; P < .05).
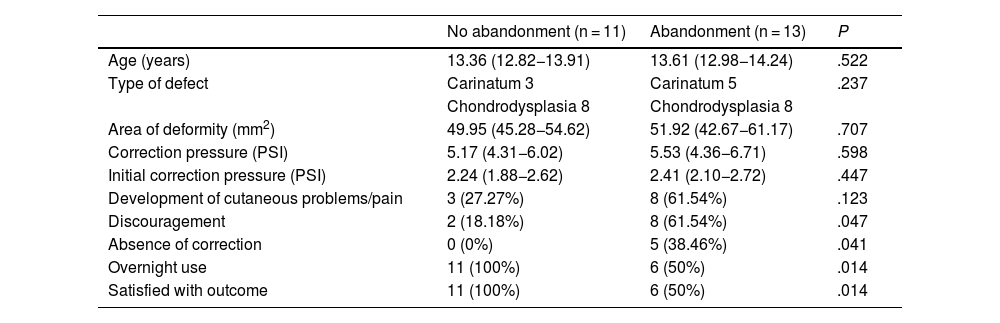
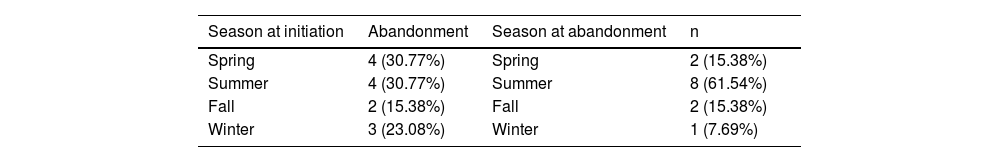
We did not find statistically significant differences in the physical characteristics of the deformity between the group patients that abandoned management with bracing and the group that did not, and both groups in the study were considered comparable (Table 1). We did not find statistically significant differences between the characteristics of the deformity and brace therapy abandonment, as previously described.3 Skin problems or discomfort, previously described4 as factors that limited the success of treatment, were not limiting factors in our case series3; however, waning or lack of motivation and absence of improvement seemed to be factors that limited adherence, as reported by Fraser et al.5 Overnight brace wearing can promote prolonged use, a factor that has proven key to success in other case series4 and made a difference in our series, as it was clearly associated with successful deformity reduction, patient adherence and a shorter duration of treatment. Although the attrition rate in our study was similar to the rates described by authors like Kang et al.3 (51.2%) or Dekonenko et al.4 (57%), it was different compared to the rate reported by Frey et al.6 (10%), which led us to exclude the possibility that weather conditions could have an impact as described by the latter; still, we found that abandonment peaked in summer (Table 2).
Characteristics at treatment initiation and during follow-up.
| No abandonment (n = 11) | Abandonment (n = 13) | P | |
|---|---|---|---|
| Age (years) | 13.36 (12.82−13.91) | 13.61 (12.98−14.24) | .522 |
| Type of defect | Carinatum 3 | Carinatum 5 | .237 |
| Chondrodysplasia 8 | Chondrodysplasia 8 | ||
| Area of deformity (mm2) | 49.95 (45.28−54.62) | 51.92 (42.67−61.17) | .707 |
| Correction pressure (PSI) | 5.17 (4.31−6.02) | 5.53 (4.36−6.71) | .598 |
| Initial correction pressure (PSI) | 2.24 (1.88−2.62) | 2.41 (2.10−2.72) | .447 |
| Development of cutaneous problems/pain | 3 (27.27%) | 8 (61.54%) | .123 |
| Discouragement | 2 (18.18%) | 8 (61.54%) | .047 |
| Absence of correction | 0 (0%) | 5 (38.46%) | .041 |
| Overnight use | 11 (100%) | 6 (50%) | .014 |
| Satisfied with outcome | 11 (100%) | 6 (50%) | .014 |
PSI, pounds per square inch.
Thus, our study did not identify any factors intrinsic to the deformity that significantly affect adherence to bracing; however, motivation and overnight use of the brace were identified as key factors to prevent treatment abandonment, which occurs in a considerable number of patients. Prospective studies could be useful to gain detailed knowledge on relevant aspects of orthotic device use and follow-up that may affect treatment outcomes.