Infection by respiratory syncytial virus (RSV) is the most common cause of hospital admission in infants aged less than 1year in Spain, and severe forms requiring hospitalization in newborns and infants aged less than 3 months and lower respiratory tract infections in infants resulting a high volume of primary care and emergency department visits are particularly frequent.1 It is also associated with the development of recurrent episodes of wheezing in infants that may compromise breathing in the medium term and with the development of asthma in individuals with no prior history of allergy.
For more than 20 years, effective prophylaxis against RSV infection has been achieved in the populations defined as being at high risk of severe or very severe disease due to RSV—clearly defined by the Sociedad Española de Neonatología (Spanish Society of Neonatology)—with the administration of a monoclonal antibody, palivizumab, which is very costly and has a short half-life.
The development of a new monoclonal antibody with a longer half-life and of demonstrated efficacy and safety, nirsevimab, presents the opportunity to offer passive immunoprophylaxis universally to all healthy newborns to prevent these forms of disease in the period that they are most at risk of severe lower respiratory tract infection, chiefly in the first year of life.2–6
The authorisation of nirsevimab for use in the European Union on November 3, 2022 has allowed its broad use in the subsequent 2023–2024 epidemic season in Spain for the first time. Nirsevimab was also recently approved by the United States Food and Drug Administration (July 17, 2023) and guidelines for its use have been published by both the Ministry of Health of Spain, through the expert group of the Directorate General of Public Health, and by the Centers for Disease Control and Prevention of the United States. The summary of product characteristics contemplates its use in healthy infants to prevent severe infection by RSV in the first season after birth and recommends administration according to official indications.
In light of the above, our Society recommends the use of nirsevimab for prophylaxis in the upcoming 2023–2024 RSV season in the groups of patients listed in Table 1, taking into account the additional considerations presented in Table 2.
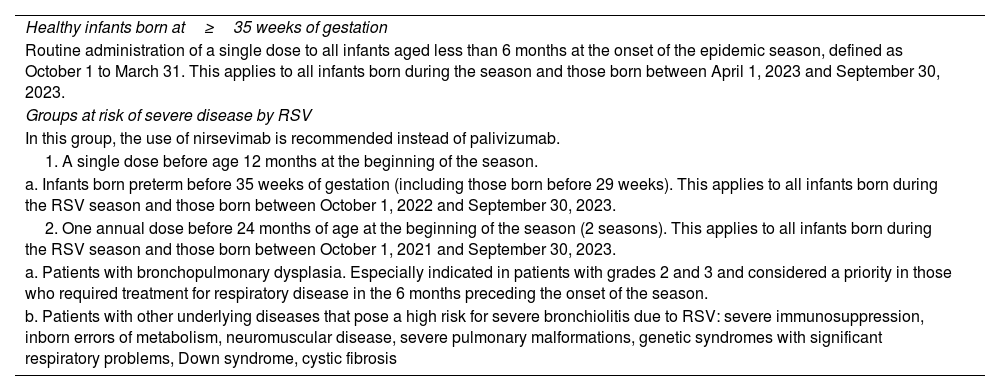
Indication for immunoprophylaxis against severe RSV infection with nirsevimab, 2023-2024 season.
| Healthy infants born at≥35 weeks of gestation |
| Routine administration of a single dose to all infants aged less than 6 months at the onset of the epidemic season, defined as October 1 to March 31. This applies to all infants born during the season and those born between April 1, 2023 and September 30, 2023. |
| Groups at risk of severe disease by RSV |
| In this group, the use of nirsevimab is recommended instead of palivizumab. |
| 1. A single dose before age 12 months at the beginning of the season. |
| a. Infants born preterm before 35 weeks of gestation (including those born before 29 weeks). This applies to all infants born during the RSV season and those born between October 1, 2022 and September 30, 2023. |
| 2. One annual dose before 24 months of age at the beginning of the season (2 seasons). This applies to all infants born during the RSV season and those born between October 1, 2021 and September 30, 2023. |
| a. Patients with bronchopulmonary dysplasia. Especially indicated in patients with grades 2 and 3 and considered a priority in those who required treatment for respiratory disease in the 6 months preceding the onset of the season. |
| b. Patients with other underlying diseases that pose a high risk for severe bronchiolitis due to RSV: severe immunosuppression, inborn errors of metabolism, neuromuscular disease, severe pulmonary malformations, genetic syndromes with significant respiratory problems, Down syndrome, cystic fibrosis |
RSV, respiratory syncytial virus.
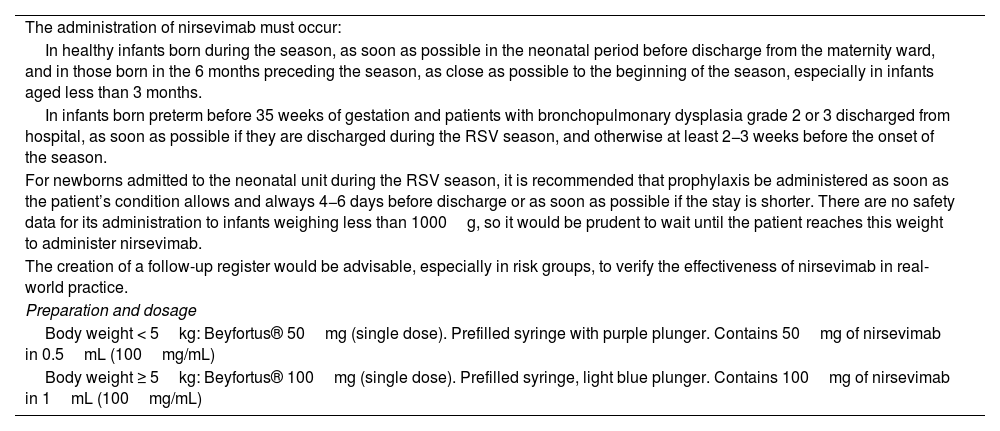
Additional considerations for immunoprophylaxis against RSV with nirsevimab.
| The administration of nirsevimab must occur: |
| In healthy infants born during the season, as soon as possible in the neonatal period before discharge from the maternity ward, and in those born in the 6 months preceding the season, as close as possible to the beginning of the season, especially in infants aged less than 3 months. |
| In infants born preterm before 35 weeks of gestation and patients with bronchopulmonary dysplasia grade 2 or 3 discharged from hospital, as soon as possible if they are discharged during the RSV season, and otherwise at least 2−3 weeks before the onset of the season. |
| For newborns admitted to the neonatal unit during the RSV season, it is recommended that prophylaxis be administered as soon as the patient’s condition allows and always 4−6 days before discharge or as soon as possible if the stay is shorter. There are no safety data for its administration to infants weighing less than 1000g, so it would be prudent to wait until the patient reaches this weight to administer nirsevimab. |
| The creation of a follow-up register would be advisable, especially in risk groups, to verify the effectiveness of nirsevimab in real-world practice. |
| Preparation and dosage |
| Body weight < 5kg: Beyfortus® 50mg (single dose). Prefilled syringe with purple plunger. Contains 50mg of nirsevimab in 0.5mL (100mg/mL) |
| Body weight ≥ 5kg: Beyfortus® 100mg (single dose). Prefilled syringe, light blue plunger. Contains 100mg of nirsevimab in 1mL (100mg/mL) |
RSV, respiratory syncytial virus.
MSL has received fees for consultation services and scientific conferences funded by Sanofi and AstraZeneca. The rest of the authors have no conflicts of interest to disclose.