In recent years, there has been an increase in Spain in the consumption of methamphetamine hydrochloride (MA), also known as shabu, mainly associated with the Filipino community.
The manufacturing of stimulants has grown considerably, and at present their consumption constitutes a serious problem worldwide.1–4
Methamphetamine is most frequently smoked, and acts on the central nervous system (CNS) by the release of amines and the inhibition of catecholamine reuptake, which produces its main desired effects: heightened energy and alertness, euphoric mood and decreased appetite.1,3
Foetal exposure to MA is associated with physical abnormalities such as prematurity, low weight, short stature and reduced head circumference (HC), neurobehavioural abnormalities (irritability, hypertonia and in some cases lethargy) and long-term sequelae.1,5 More studies are needed to broaden these results.
Consumption of MA during pregnancy is an alarming health problem in developed countries.1,2 Its vasoconstrictive effects contribute to placental dysfunction, and its ready diffusion through the placental barrier can have a significant impact on the foetus.1,5 Nevertheless, cases with associated malformations have not been reported.
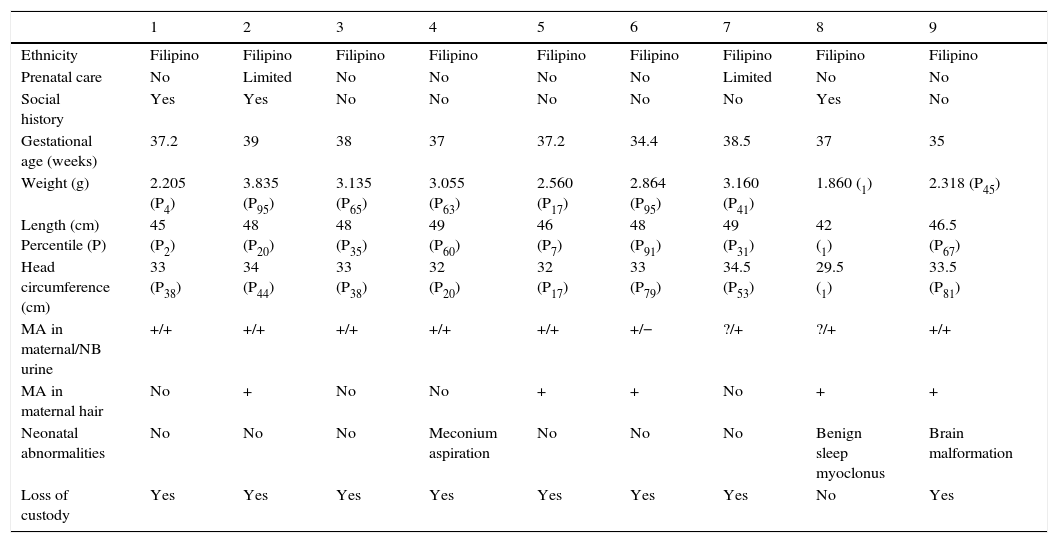
We describe nine cases of children born to mothers that used shabu observed in our neonatal unit between June 2013 and March 2016 (Table 1).
Case summary.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Ethnicity | Filipino | Filipino | Filipino | Filipino | Filipino | Filipino | Filipino | Filipino | Filipino |
| Prenatal care | No | Limited | No | No | No | No | Limited | No | No |
| Social history | Yes | Yes | No | No | No | No | No | Yes | No |
| Gestational age (weeks) | 37.2 | 39 | 38 | 37 | 37.2 | 34.4 | 38.5 | 37 | 35 |
| Weight (g) | 2.205 (P4) | 3.835 (P95) | 3.135 (P65) | 3.055 (P63) | 2.560 (P17) | 2.864 (P95) | 3.160 (P41) | 1.860 (1) | 2.318 (P45) |
| Length (cm) Percentile (P) | 45 (P2) | 48 (P20) | 48 (P35) | 49 (P60) | 46 (P7) | 48 (P91) | 49 (P31) | 42 (1) | 46.5 (P67) |
| Head circumference (cm) | 33 (P38) | 34 (P44) | 33 (P38) | 32 (P20) | 32 (P17) | 33 (P79) | 34.5 (P53) | 29.5 (1) | 33.5 (P81) |
| MA in maternal/NB urine | +/+ | +/+ | +/+ | +/+ | +/+ | +/− | ?/+ | ?/+ | +/+ |
| MA in maternal hair | No | + | No | No | + | + | No | + | + |
| Neonatal abnormalities | No | No | No | Meconium aspiration | No | No | No | Benign sleep myoclonus | Brain malformation |
| Loss of custody | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
MA, methamphetamine; NB, newborn.
We found some common risk factors in the cases in our series: Filipino ethnicity, little to no pregnancy care, and serious social problems (some cases had a relevant previous social history). In five cases, chronic use throughout pregnancy could be proven by the detection of MA in the mother's hair, and we did not find the use of any other abused substances in any case, probably because in this population, MA is not used recreationally, but to endure long work shifts. Table 1 presents the perinatal results of our study. We would like to highlight the last case, a newborn with a severe brain malformation (bilateral ventriculomegaly with mass effect in the posterior fossa, abnormal development of the right cortex, thinned left cortex and possible absence of the corpus callosum) that required neurosurgical intervention. Exposure to MA could account for this malformation, as any insult in the first trimester, for example, of a vascular nature, can lead to severe anomalies in cortical development, but due to the lack of prenatal ultrasound scans, we could not determine the time at which the lesion developed.
It is worth noting that in spite of MA being highly addictive, none of the newborns manifested neurobehavioral symptoms or lethargy in the first days of life, including those in whom there was evidence of chronic exposure throughout gestation. The use of shabu was a red flag that led to the detection of underlying social problems of such severity that they led to child custody loss in all cases, except for one child that remains in the home under followup by social services.
Methamphetamine is one of the most addictive abused drugs, and is associated with multiple psychosocial and economic disadvantages that interfere with the development of an appropriate environment for raising and caring for an infant.4,6
The use of MA during pregnancy is associated with low socioeconomic status, increased risk of legal problems, a higher prevalence of single-parent households and maternal perception of low quality of life. It usually occurs in the context of substance abuse in the social and family environments.4,6
Women that use MA during pregnancy are also more frequent consumers of other teratogenic substances that must be taken into account, such as alcohol, tobacco and cannabis.1,4–6 We found an increased prevalence of psychiatric comorbidity: depression, paranoid ideation, insomnia and aggressiveness.3,4,6
The main problem associated with MA use during pregnancy is inadequate or absent prenatal care, making it difficult to connect with social and mental health services.2,4
We also found evidence of low health care use in the postnatal period leading to instances of child neglect and abuse in these households, with an increased frequency of child custody loss.2,3
We present the first study on prenatal exposure to MA in the Filipino community conducted in Spain, which includes the case of one newborn with a CNS malformation, with evidence of serious social problems in all cases that were not detected before birth due to non-use of prenatal care.
This article is intended as a warning call to promote the identification of these at-risk populations and the implementation of multidisciplinary prenatal care involving obstetrics, psychological support and social services. With this approach, we could strive to work with this collective during pregnancy to manage their addiction, prevent its adverse effects in newborns, and strengthen family bonds.
Please cite this article as: Manzano Varo C, López-Vílchez MÁ, Román Eyo L, García García J, Mur Sierra A. Exposición prenatal a metanfetamina «shabú». An Pediatr (Barc). 2017;86:96–97.
Previous presentation: This study was presented as a poster at the XXV Congreso de Neonatología y Medicina Perinatal de la SEN-V Congreso de Enfermería Neonatal; May 20–22, 2015; Seville, Spain.