Gastroschisis is a malformation of the abdominal wall whose management is complex.1 In low-income countries, the mortality reaches up to 90% due to increased risk of sepsis associated with the use of mechanical ventilation or central venous access lines.2 We describe the technique of bedside staged reduction without sutures or general anesthesia for simple gastroschisis. After patient stabilization and administration of morphine and paracetamol for analgesia, the bowel is examined and the Gastroschisis Prognostic Score (GPS) calculated. If the GPS is 0 or 1, the colon is decompressed and the staged reduction initiated, placing the irreducible herniated bowel loops in a surgical retractor (Fig. 1). In patients with a GPS of 4, a silo is placed over the bowel without manipulation (Fig. 2). Staged reductions are then performed under sedation and analgesia followed by closure with alginate dressings (Appendix B video). This approach has been found to reduce the duration of parenteral nutrition from 27 to 21 days and of mechanical ventilation from 100% to 57%, with a decrease in mortality from 22% to 2% and in the incidence of sepsis from 70% to 37% and no increase in length of stay.3 Thus, the use of a preformed silo and sutureless closure is feasible and safe, even in patients with a GPS of 4, and may offer additional advantages given that it does not require tracheal intubation or general anesthesia.
Patient with a Gastroschisis Prognostic Score (GPS) of 0. Following neonatal stabilization and placement of a nasogastric tube, under analgesia with intravenous morphine and paracetamol, the bowel is assessed (adherences, size of the defect, atresia, GPS). If the GPS is 0 or 1, the colon is totally decompressed with enemas and the absence of volvulus and congenital bands in the small bowel verified. If possible, the stomach and colon are reduced, leaving the bowel loops outside the abdomen and placing them in a surgical retractor serving as a preformed silo. In patients with a GPS of 0 or 1, the loops closest to the wall defect can be reduced first.
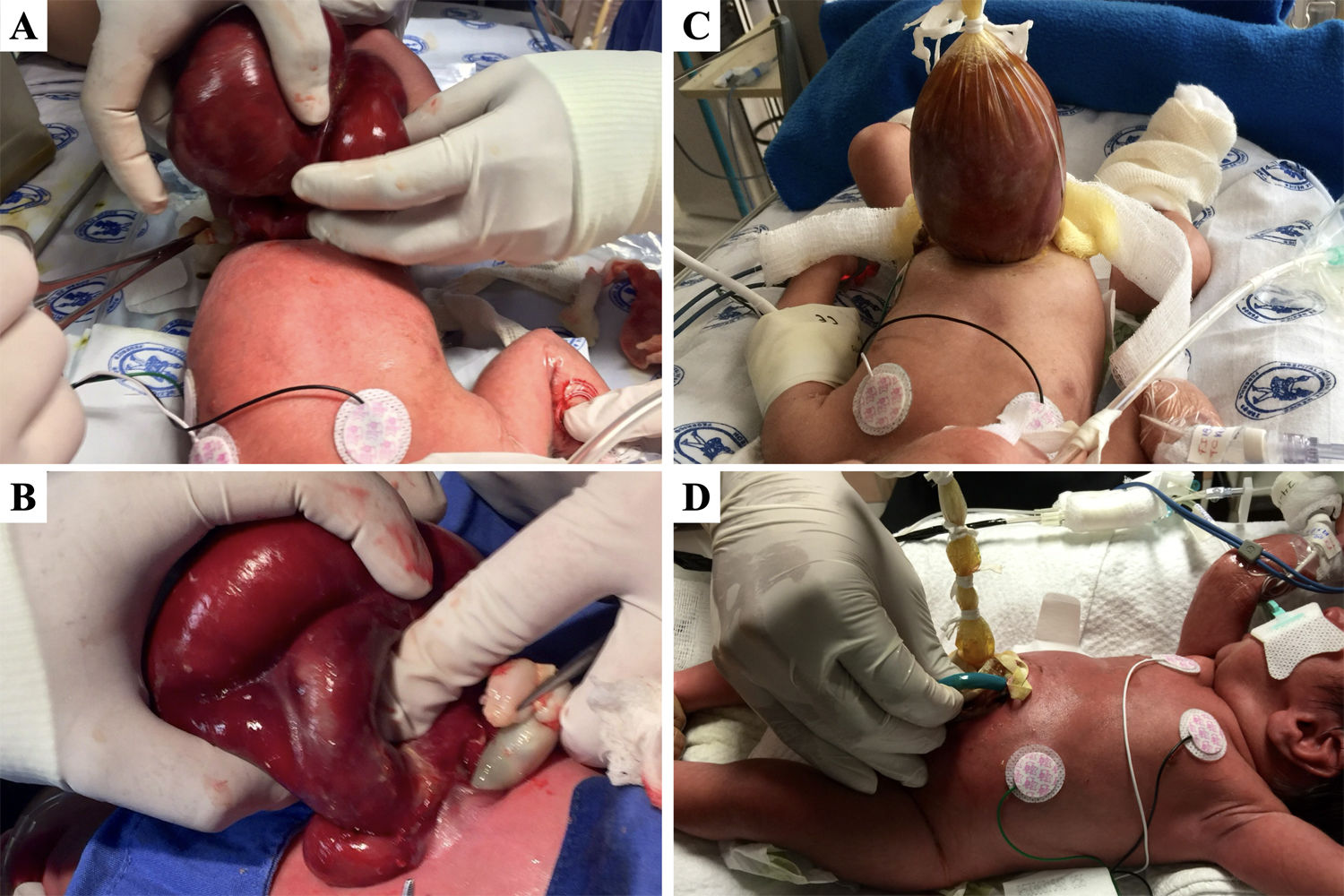
In patients with a Gastroschisis Prognostic Score of 4 (A, B), the silo is placed over the loops without bowel manipulation (C) and staged reductions performed from the top using cotton tape (D). At this time, if central venous access is unavailable, vascular access is established, preferably with a peripherally-inserted central catheter. Staged reductions are performed twice a day, based on the condition of the neonate, under sedation and analgesia with morphine. This is followed by sutureless closure with alginate dressings. Enteral nutrition starts after three days of progressive nasogastric tube clamping when drainage is less than 40 mL/day. Feeds start at 20 mL/kg/day, preferably with breast milk, for 3 days.