Infections are a significant cause of morbidity and mortality in cancer patients (mortality is estimated at around 3%). Febrile neutropenia often leads to the hospitalisation of cancer patients, increasing the risk of nosocomial infection, as well as health costs due to the hospital admission.
MethodsAn ambispective (01 July 2015–12 July 2018) observational study was conducted on all episodes of chemotherapy-induced febrile neutropenia in a paediatric population. A record was made of age, gender, weight percentile (WHO), length of hospital stay (days), temperature (°C), microbial isolation, infectious source, antibiotic or antifungal prophylaxis, haemoglobin (g/dl), platelets (/mm3), neutrophils (/mm3), lymphocytes (/mm3), monocytes (/mm3), CRP (mg/L) and procalcitonin (PCT) (ng/ml) on admission, and days with neutropenia<500/mm3. Statistical analysis was performed using the SPSSv.23 program.
ResultsThe study included 69 patients, and 101 episodes were recorded. The mean stay was 7.43 days (median 6 days). Microbial isolation was found in 44.6% of the episodes, with no infectious source identified in 36% of them. An inverse correlation was found between haemoglobin, platelets, and lymphocytes on admission and the hospital stay (−0.356: P=.001, −0.216: P=.042, and −0.216: P=.042, respectively). The mean stay was greater if there was a CRP >90mg/L (10.94 vs. 6.66 days, P=.017), if PCT>1ng/ml (16.50 vs. 6.77 days, P=.0002), if ≤100 neutrophils (8.27 vs. 5.04 days P=.039) on admission, and if there was microbe isolation (9.54 vs. 5.78 days P=.006)
ConclusionThe relationship between haemoglobin, platelets, and lymphocytes on admission and the mean stay is inversely proportional. In addition, those patients with ≤100 neutrophils, CRP>90mg/L, and PCT>1ng/ml on admission had a longer hospital stay.
Las infecciones son una causa importante de morbimortalidad en los pacientes con cáncer (mortalidad estimada en 3%). La neutropenia febril conlleva con frecuencia el ingreso hospitalario de los pacientes oncológicos, incrementando el riesgo de infección nosocomial así como los costes sanitarios por ingresos.
MétodosEstudio observacional ambispectivo (01/07/2015–31/12/2018) de los episodios de neutropenia febril post-quimioterapia en población pediátrica. Se recogieron edad, sexo, percentil de peso(OMS), estancia hospitalaria(días), temperature (°C), aislamiento de germen, foco infeccioso, profilaxis o no antibiótica y antifúngica, cifras de hemoglobina(g/dl), plaquetas(/mm3), neutrófilos(/mm3), linfocitos(/mm3), monocitos(/mm3), proteína C reactiva (PCR)(mg/L) y procalcitonina(PCT)(ng/ml) al ingreso y días con neutropenia <500/mm3. El análisis estadístico se realizó con el programa SPSSv.23.
ResultadosDe 69 pacientes, se registraron 101 episodios. La estancia media fue de 7,43 días (mediana 6 días). Se aisló germen en un 44.6% de los episodios, no identificándose foco infeccioso en un 36% de los mismos. Se halló correlación inversa entre hemoglobina, plaquetas y linfocitos al ingreso con la estancia hospitalaria (−0,356 (p0,001); −0,216 (p0,042) y −0,216(p0,042) respectivamente). La estancia media fue mayor si al ingreso presentaron PCR>90mg/L(10,94 vs.6,66 días p0,017), si PCT>1ng/ml (16,50 vs.6,77 días p0,0002), si ≤100neutrófilos(8,27vs.5,04 días p0,039) y si hubo aislamiento microbiológico (9,54vs.5,78 días p0,006).
ConclusiónLa relación entre hemoglobina, plaquetas y linfocitos al ingreso con la estancia media es inversamente proporcional. Además, aquellos pacientes con ≤100 neutrófilos al ingreso, PCR>90mg/L y PCT>1ng/ml presentaron mayor estancia media. Estos factores podrían ser importantes en el manejo de la neutropenia febril en el paciente con cáncer infantil.
Febrile neutropenia is a frequent complication in children that receive chemotherapy.1 Up to one third of episodes of neutropenia after chemotherapy manifest with fever.2 This corresponds to 0.76 episodes of fever per 30 days of neutropenia. Several studies have reported that the infection is severe in up to 25% of episodes, with an overall mortality of approximately 3%.3
The available evidence suggests that early administration of appropriate antibiotherapy decreases mortality due to bacterial infection.4 On the other hand, delayed administration of antibiotherapy has been associated with poorer outcomes.5
For this reason, patients with febrile neutropenia after chemotherapy endure long hospitalizations and are given broad-spectrum antibiotics.3–5 The prolonged lengths of stay have a significant impact on the quality of life of these patients and their families.6 As health professionals, it is essential that we know how to correctly manage these episodes both in the emergency department and in the subsequent hospitalization.
Blood cancers,7 the duration of neutropenia,7 sepsis,8 low blood pressure,8 non-white race9 and age more than 12 years9 have been identified as risk factors for an increased mean length of stay.
On the other hand, the use of granulocyte-colony stimulating factor (G-CSF) has been associated with a significantly lower mean length of stay (1–2 days).10,11 In the paediatric population, current guidelines recommend using G-CSF for primary or secondary prophylaxis or for treatment only in patients classified as high-risk.12
In addition, postchemotherapy febrile neutropenia episodes place a considerable financial burden on the national health system8,13 in terms of both direct and indirect costs.
In light of the above, identifying the factors associated to prolonged lengths of stay is of the essence.
The main objective of our study was to identify the risk factors associated with an increased length of stay in episodes of febrile neutropenia associated with chemotherapy in our hospital over a 3-year period.
The secondary objective was to describe the distribution of microbiological isolates and foci of infection in our patients.
MethodsWe conducted a retrospective and prospective observational study (01/07/2015–31/12/2018) of the episodes of febrile neutropenia associated to chemotherapy in paediatric patients managed in a tertiary care hospital.
The inclusion criteria were age 0–18 years, delivery of chemotherapy by the Department of Paediatric Oncology and Haematology, an axillary temperature of 38°C or higher and an absolute neutrophil count of 500/mm3 or lower.
The exclusion criteria were age more than 18 years, neutropenia of any aetiology unrelated to chemotherapy, an absolute neutrophil count of more than 500cells/mm3 (moderate or mild neutropenia not requiring hospital admission).
We collected data for the following variables: age, sex, weight percentile, body temperature (°C), pathogen isolation (blood culture, urine culture, stool culture, throat culture, rapid respiratory syncytial virus [RSV] and influenza A and B tests [Alere BinaxNOW ® RSV and BinaxNOW ® Influenza A & B]), administration or lack of administration of antibiotic and/or antifungal prophylaxis, haemoglobin concentration (g/dL), platelet count (/mm3), neutrophil count (/mm3), lymphocyte count (/mm3), monocyte count (/mm3), C-reactive protein (CRP) (mg/L) and procalcitonin (PCT) (ng/ml) levels at admission, days with neutropenia with a neutrophil count of less than 500/mm3, focus of infection and length of stay in days.
We calculated the Pearson r to analyse the correlation between the length of stay and the weight percentile, temperature, haemoglobin concentration, platelet, neutrophil, lymphocyte and monocyte counts, levels of CPR and PCT and days with neutropenia with less than 500 neutrophils/mm3.
We also made analyses by subgroups using the Student t test, comparing the mean length of stay of patients based on whether they had a neutrophil count of 100/mm3 or less at admission, a CPR level of 90mg/L or greater, a PCT level of 1ng/mL or greater, microbial isolation, the focus of infection, and use antibiotic and/or antifungal prophylaxis.
We used the personal data of participants in adherence with current legislation and safeguarded patient confidentiality. No report or publication will therefore include any identifiable data. The study was approved by the Clinical Research Ethics Committee.
The analysis was carried out with the statistical software SPSS version 23. We defined statistical significance as a p-value of less than 0.05 in any of the tests.
ResultsIn the period under study, 69 patients met the inclusion criteria, corresponding to a total of 101 episodes of postchemotherapy febrile neutropenia.
The mean length of stay was 7.38 days (median, 6 days). The remaining median values were age 6 years, weight on the 25th percentile, fever of 38.2°C, haemoglobin concentration of 8.9g/dL, platelet count of 54 000/mm3, neutrophil count of 100/mm3, lymphocyte count of 200/mm3, monocyte count of 0/mm3, CRP level of 46mg/L, PCT level of 0.26ng/mL, 3 days with neutrophil count of less than 500/mm3.
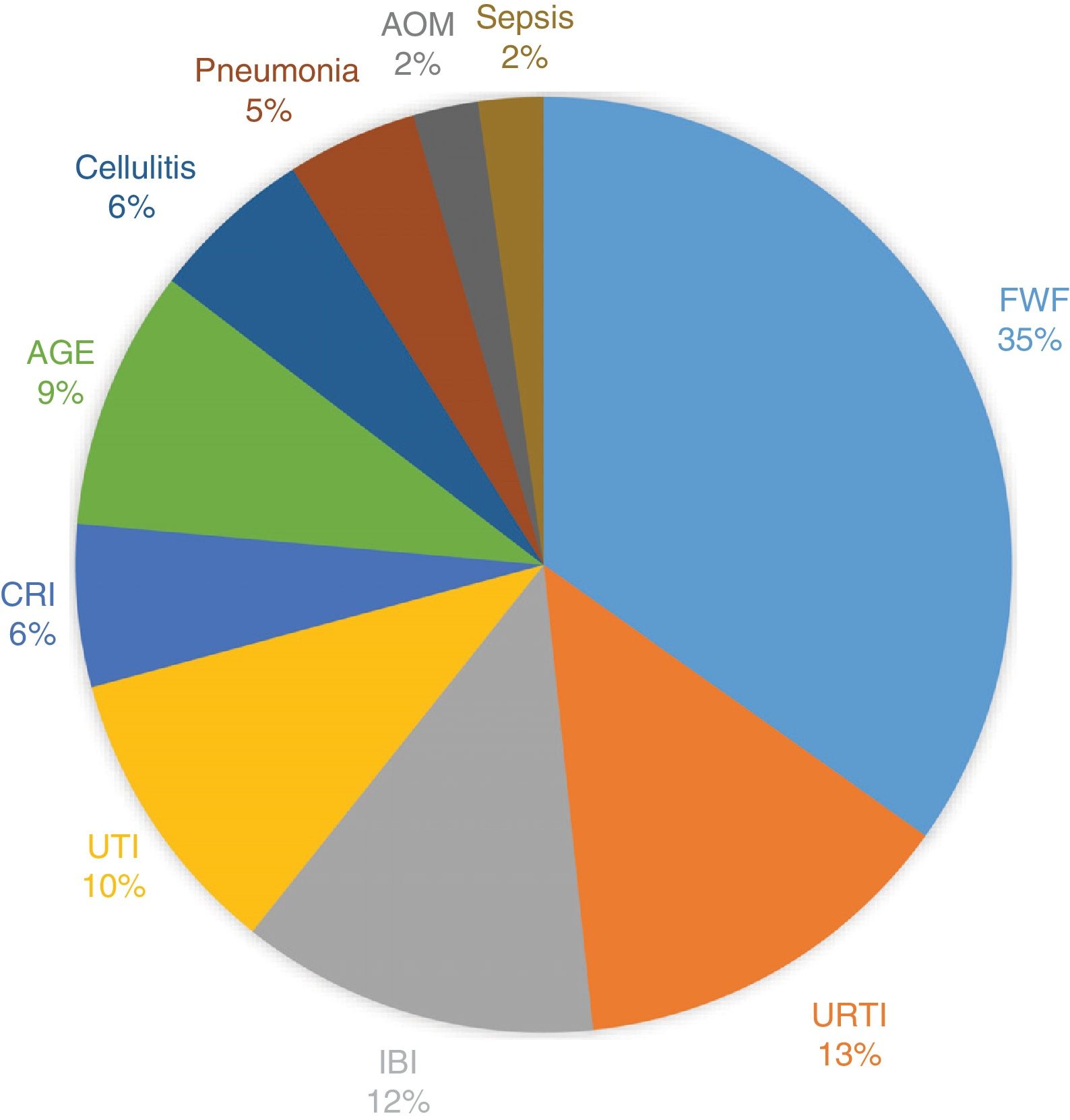
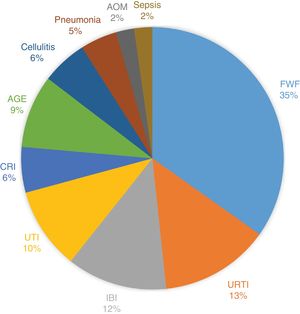
A microbial isolate was obtained in 45 episodes (44.6%). Fig. 1 presents the distribution of the foci of infection.
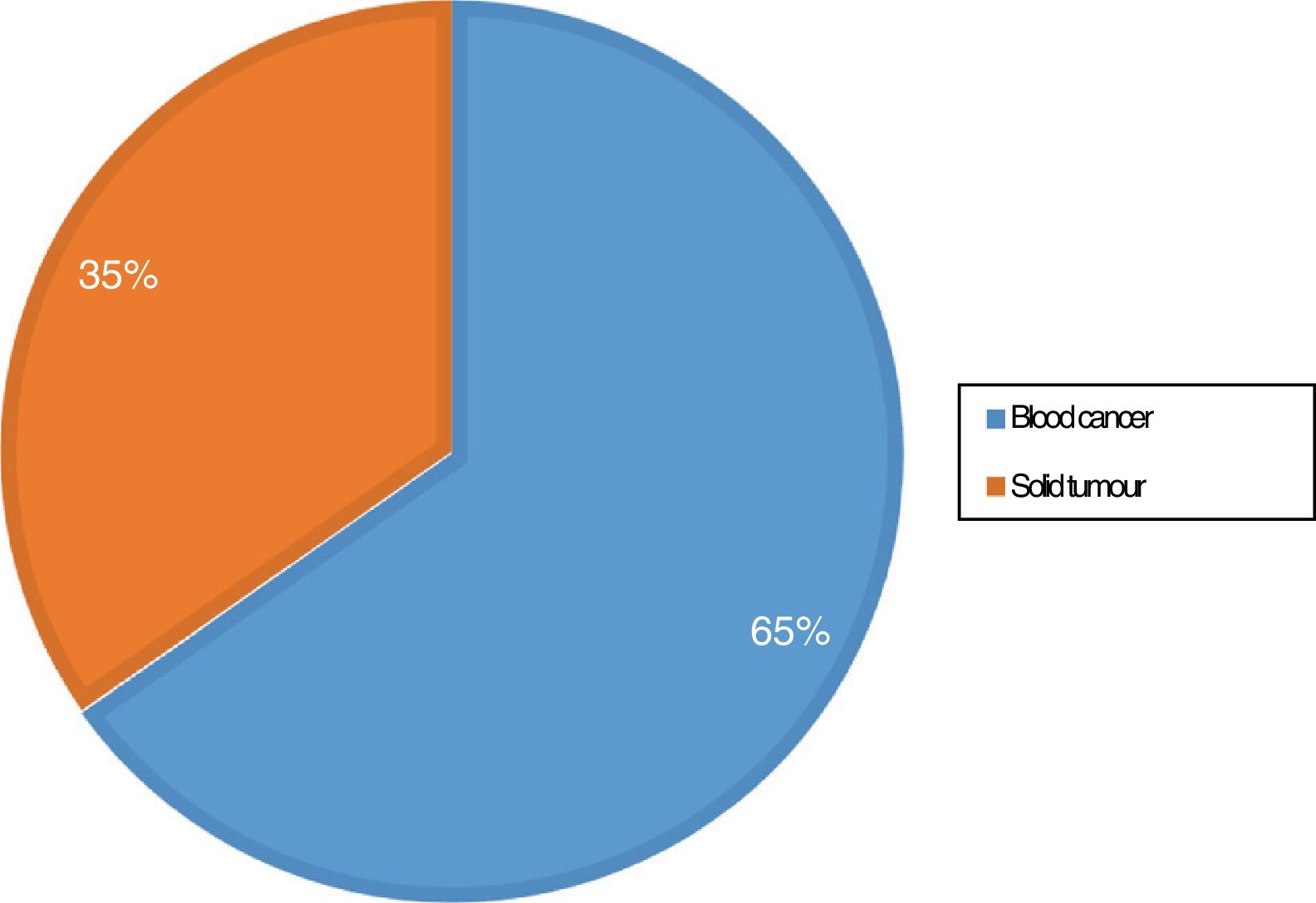
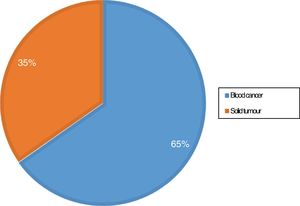
Fig. 2 presents the distribution of patients by type of tumour.
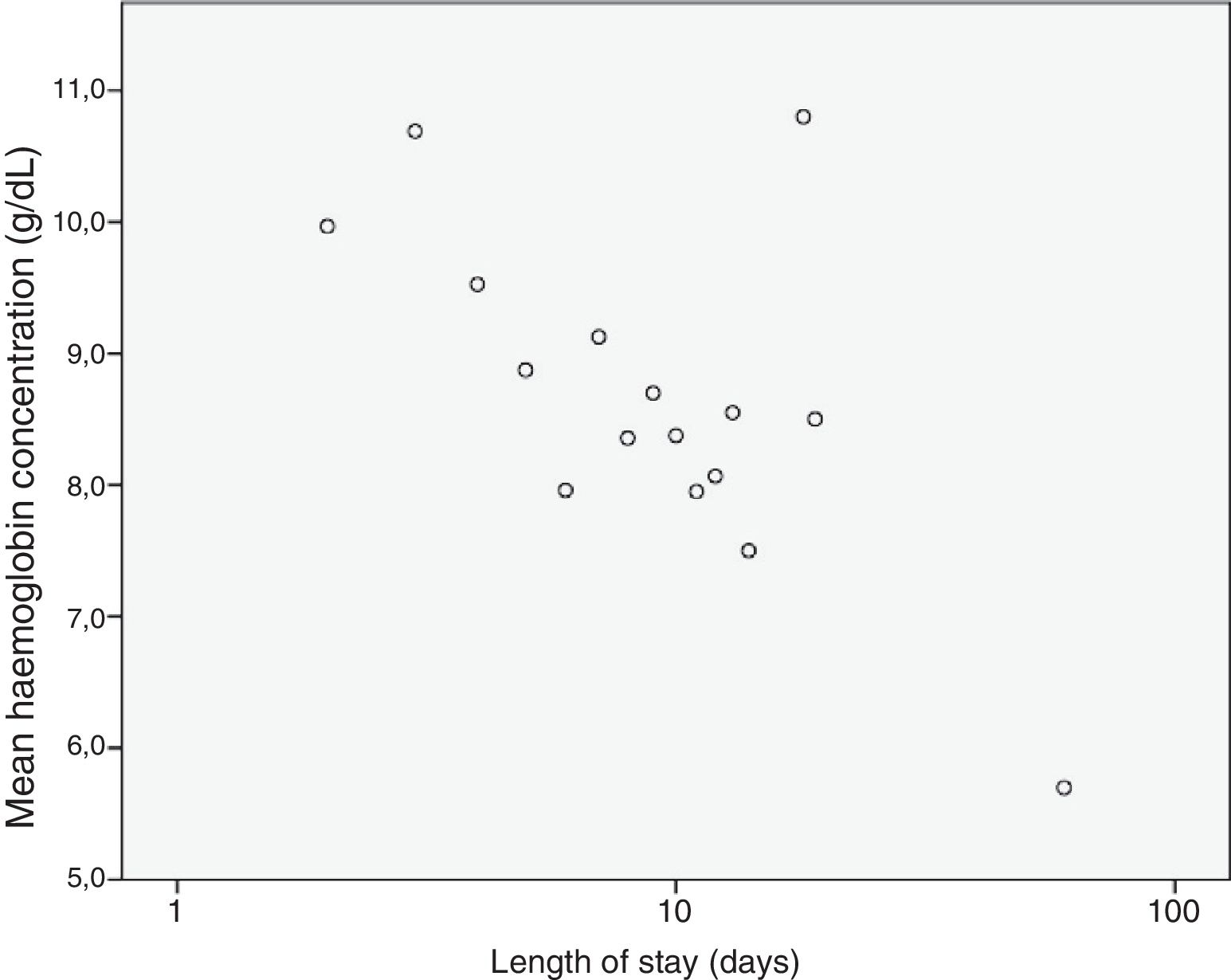
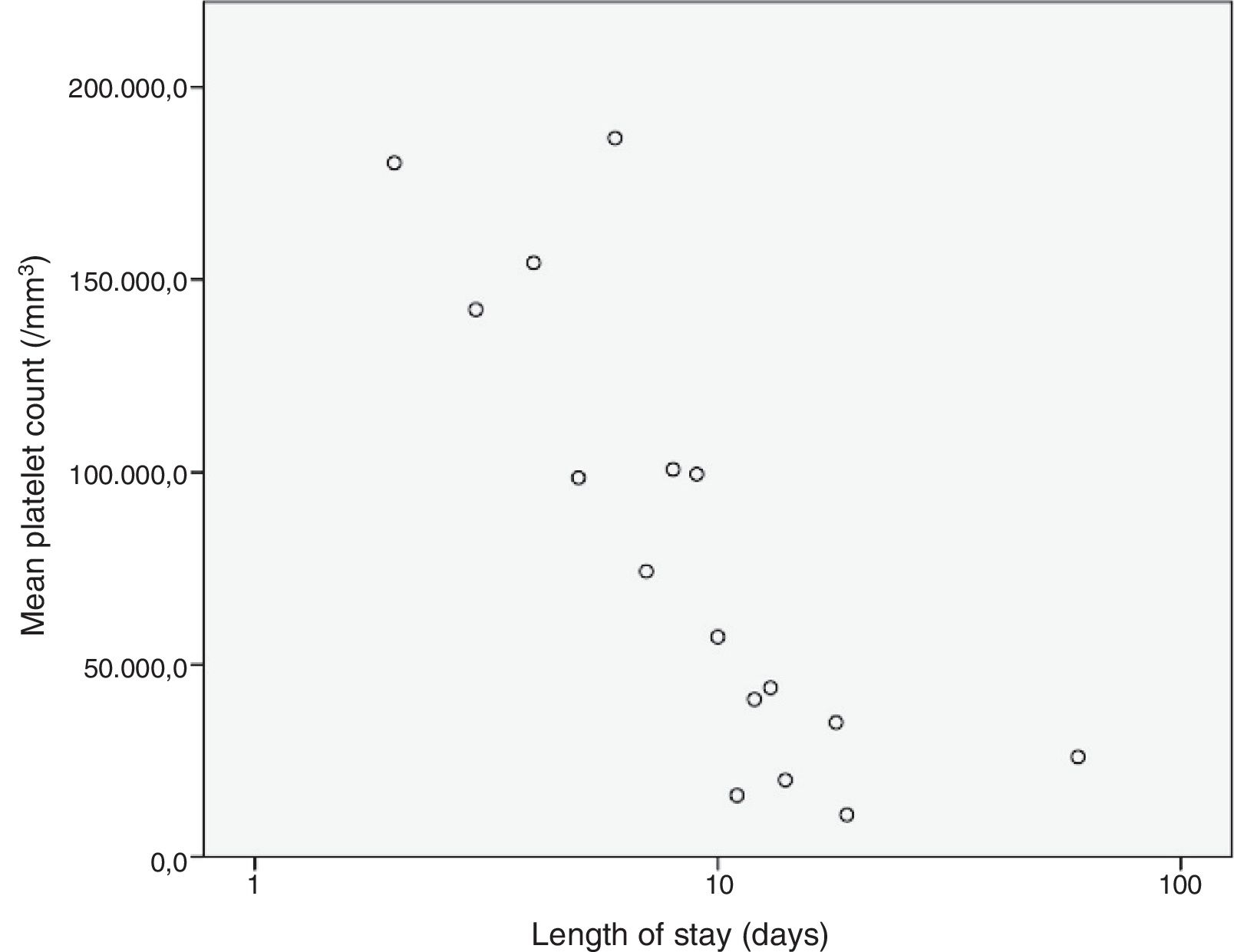
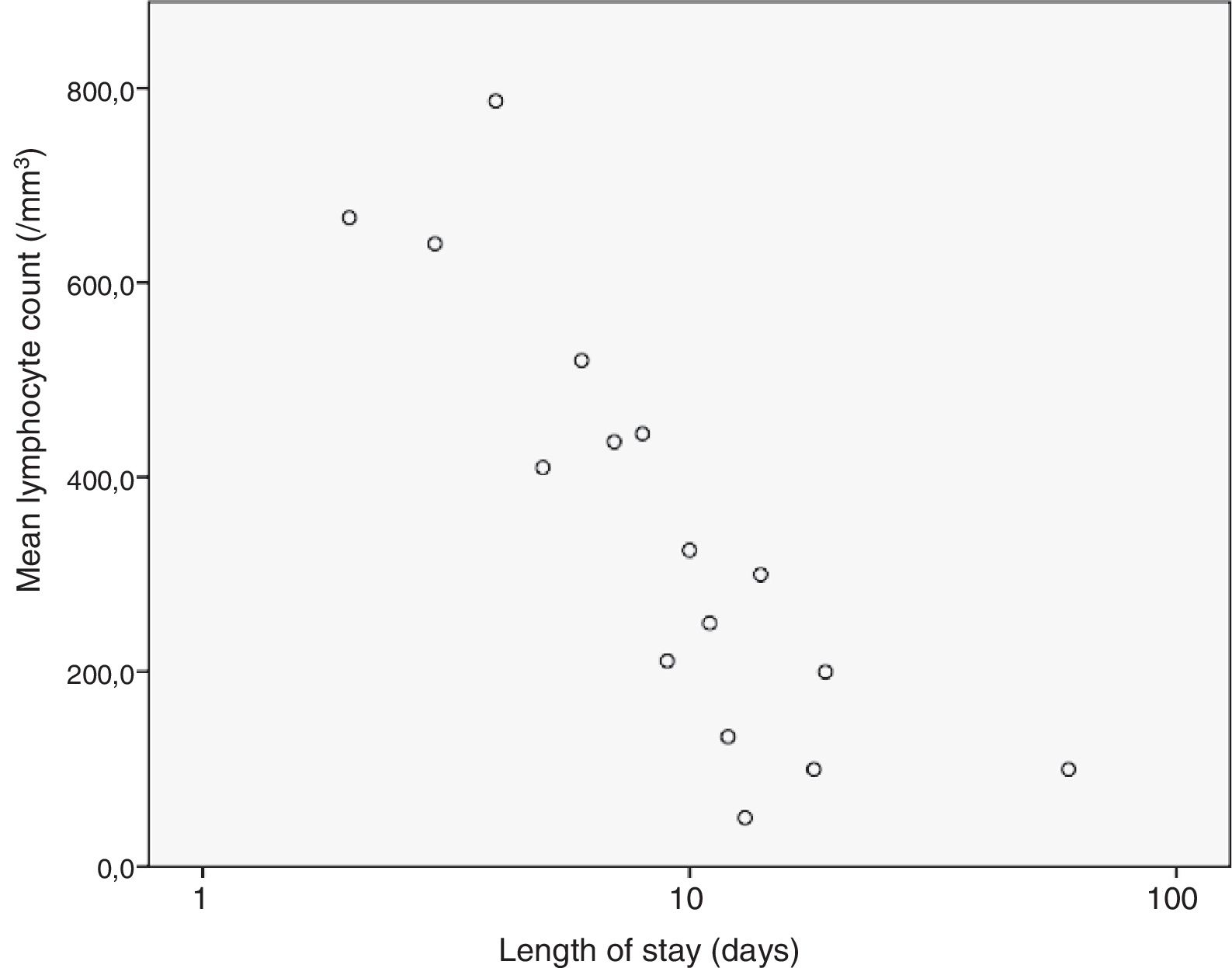
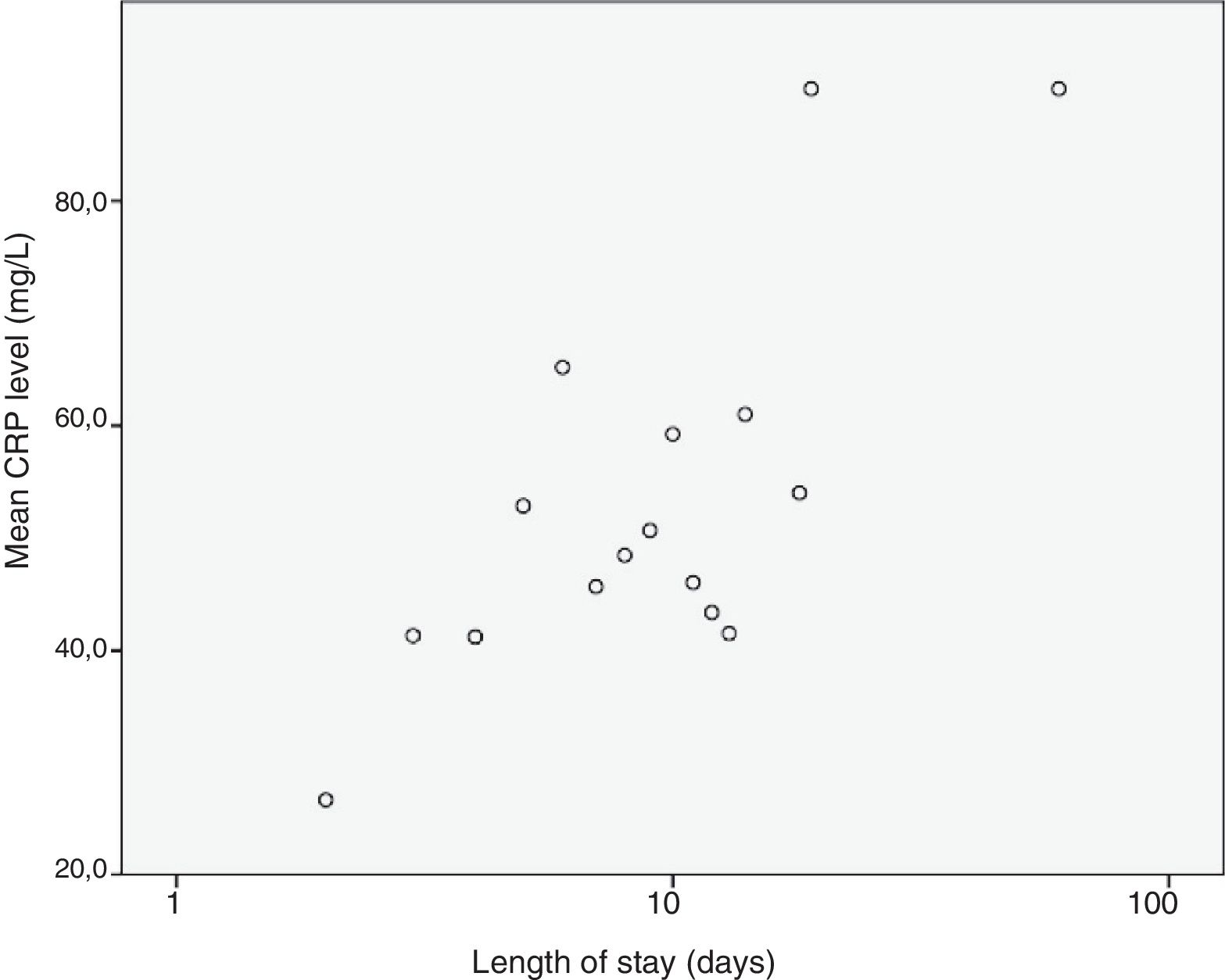
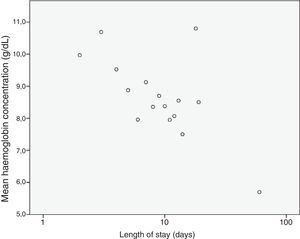
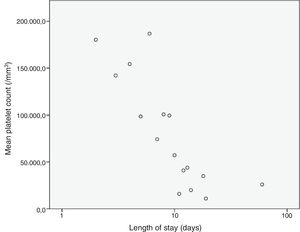
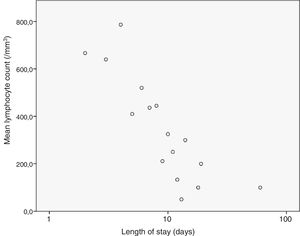
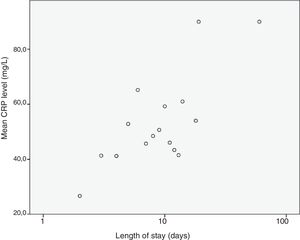
We analysed the correlation of the length of stay to the rest of the quantitative variables under study, and found a statistically significant correlation with the haemoglobin concentration (–0.307; P=.002), the platelet count (–0.215; P=.031) and the lymphocyte count (–0.205; P=.04) at admission and the CPR level (0.204; P=.041), results that are represented in Figs. 3 to 6. The correlations with the remaining variables were not statistically significant, although the p-value corresponding to the neutrophil count at admission neared the threshold of significance (–0.191; P=.056).
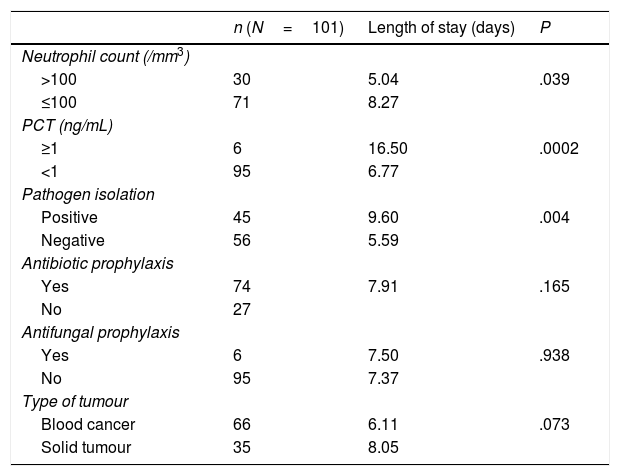
The remaining results of the analysis can be found in Table 1.
Analysis of mean length of stay by group (Student t test).
| n (N=101) | Length of stay (days) | P | |
|---|---|---|---|
| Neutrophil count (/mm3) | .039 | ||
| >100 | 30 | 5.04 | |
| ≤100 | 71 | 8.27 | |
| PCT (ng/mL) | .0002 | ||
| ≥1 | 6 | 16.50 | |
| <1 | 95 | 6.77 | |
| Pathogen isolation | .004 | ||
| Positive | 45 | 9.60 | |
| Negative | 56 | 5.59 | |
| Antibiotic prophylaxis | .165 | ||
| Yes | 74 | 7.91 | |
| No | 27 | ||
| Antifungal prophylaxis | .938 | ||
| Yes | 6 | 7.50 | |
| No | 95 | 7.37 | |
| Type of tumour | .073 | ||
| Blood cancer | 66 | 6.11 | |
| Solid tumour | 35 | 8.05 |
The mean stay reported in the literature ranges between 5 and 19.7 days per episode,7–9,13,14 depending on the case series. The mean found in our sample fell within this range and was consistent with most published studies.8,9,13,14
In our sample, the percentage of cases in which a pathogen was isolated was slightly greater compared to the literature, in which reported proportions range from 10% to 40%.2,15,16 This may be explained in part by viruses causing a substantial percentage of infections in febrile neutropenia episodes (44–57%),17 and thus in our hospital we perform rapid tests for RSV and influenza during the epidemic season.
On the other hand, the distribution of cases by focus of infection was consistent with the literature18: 32% of episodes are of fever without a focus (35% in our sample), and 20% are episodes of bacteraemia (12% cases of invasive bacterial infection and 6% cases of central catheter-related infection).
We ought to highlight that the length of stay for episodes in which a causative pathogen was identified was 4 days longer (a statistically significant difference). This could be due to a greater severity of disease or to an intent to ensure completion of the duration of antibiotherapy required by each infection.
When it came to the factors associated with an increased length of stay, our results suggested a negative correlation with the haemoglobin concentration, the platelet count and the lymphocyte count, factors that had not been previously described. We also found a positive correlation between the mean length of stay and the CPR levels at admission, which seems logical and is consistent with the previous literature.
In addition, we found a statistically significant association between the PCT and neutrophil values at admission on one hand and an increased length of stay on the other. These factors have been previously described in the literature as predictors of poor outcomes,19,20 but not of prolonged lengths of stay. These results agree with previous findings, as episodes with poor outcomes may be associated with longer lengths of stay.
Although we did not find a statistically significant association between the neutrophil count at admission and the length of stay, the p-value neared the threshold of significance, so it is likely that this association would be significant if analysed in a larger sample.
One of the main limitations of our study was the small sample size. In addition, in most patients we were unable to determine whether they received G-CSF, which has been associated with shorter mean lengths of stay and may have had an impact on the results. Another limitation is that the time elapsed to administration of the first dose of antibiotherapy in the emergency department was not recorded, although the previous literature suggests that this variable is not associated with length of stay.21,22
Identifying these factors as new indicators of an increased length of stay may help guide clinical decision-making in these episodes and optimise the use of available resources, as well as plan the management of patients to try to minimise the impact to their quality of life.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-Heras Í, Raynero-Mellado RC, Díaz-Merchán R, Domínguez-Pinilla N. Neutropenia febril posquimioterapia. Estancia hospitalaria y experiencia en nuestro medio. An Pediatr (Barc). 2020;92:141–146.