Understanding the underlying factors that influence the approach to overweight and obesity in children is basic to best support families searching a solution to this important public health problem.
ObjectiveTo assess attitudes and feelings of paediatric staff in addressing overweight and childhood obesity to parents, exploring perceived barriers and facilitators, for an effective care.
Participants and methodQualitative study by means of individual semi-structured questionnaires of paediatric staff (paediatricians and paediatrician nurses; n = 57; 68% female) of primary health care centres and hospitals in Mallorca. Thematic analysis was done.
ResultsThree themes emerged from the data: “Parents’ attitude in childhood obesity” (sub-themes “The conscience of parents”, “The parents ask for help”), “Paediatric staff and childhood obesity” (sub-themes “Approaching to the problem: The interview with parents”, “Looking together for the solution”), and “System barriers” (sub-themes “Improving teamwork and health policy”, “Family participation in addressing childhood obesity”).
ConclusionsPaediatric staffs know how to treat childhood obesity, but demand training on motivation. Effectivity on therapy of childhood obesity will be obtained after parents/carers recognize the problem and establish a trustful relationship with paediatric staff. The health system is still a barrier to the activity of paediatric personnel.
Comprender los factores que influyen en el tratamiento del sobrepeso y la obesidad infantil es crucial para ofrecer el mejor apoyo a las familias y solucionar este grave problema de salud pública.
ObjetivoDescribir las actitudes y sentimientos del personal de pediatría al tratar con los padres el sobrepeso y la obesidad de sus hijos, explorando los facilitadores y las barreras percibidas, a fin de realizar una atención efectiva.
Sujetos y métodoEstudio cualitativo por cuestionarios individuales semiestructurados de personal pediátrico (pediatras y enfermeras pediatras; n = 57; 68% mujeres) de centros de atención primaria y hospitales de la isla de Mallorca, sobre las que se aplicó un análisis temático.
ResultadosSe identificaron 3 temas: “La actitud de los padres en la obesidad infantil” (subtemas “La conciencia de los padres”, “Los padres piden ayuda”), “El personal pediátrico y la obesidad infantil” (subtemas “Aproximación al problema: La entrevista con los padres”, “Buscando juntos la solución”) y “Barreras del Sistema” (subtemas “Mejorar el trabajo en equipo y la política de salud”, “Participación familiar al abordar y estudiar la obesidad infantile”).
ConclusionesEl personal pediátrico sabe tratar la obesidad infantil, pero demanda entrenamiento en motivación. La terapia de la obesidad infantil será efectiva cuando los padres/cuidadores reconocen el problema y establecen confianza con los equipos pediátricos. El sistema de salud aún es una barrera a la actividad del personal pediátrico.
In the paediatric age group, obesity is the most frequent noncommunicable chronic disease and nutritional and metabolic disorder.1 Obese children and adolescents are 5 times more likely to be obese in adulthood compared to their non-obese peers.2 A recent systematic review found substantial differences in the frequency of overweight and obesity between European countries, with a tendency towards stabilization, although the growing prevalence in some Mediterranean countries, including Spain, is alarming.3 Based on data from the 2015 ALADINO study, 18.1% of children aged 6 to 9 years are obese and 23.2% overweight.4 The same trend is found in the Balearic Islands, with a prevalence of obesity of 10.4% and a prevalence of overweight of 14.7%.5 Since obesity is associated with serious noncommunicable diseases,6–10 strategies must be implemented to reverse the obesity epidemic in children. Without intervention, infants and young children with obesity may continue to be obese through childhood, adolescence and adulthood.2
Despite the importance of addressing overweight and obesity from the earliest possible age, previous qualitative evidence obtained in other countries shows that health professionals feel that childhood overweight and obesity are subjects that are difficult to broach with parents.11–13 One of the main challenges identified by clinicians in relation to this health problem is parental awareness and sensitivity. Parents frequently fail to recognise overweight or obesity in their children,14,15 or may feel guilty, unhappy or concerned when informed by paediatricians of the presence of excess weight in their children, which is an added difficulty in the management of childhood obesity.16–21 Even if parents are aware of excess weight in their children, they may be reluctant to control their weight, as they may feel confident that this excess is natural and that it will resolve spontaneously and effortlessly.22 When parents themselves are overweight or obese, addressing the subject is all the more complicated.18 As a result, paediatric health care workers may feel uncomfortable discussing excess weight in children with their parents or caregivers.18 In fact, paradoxically, it is frequent for both health care workers and parents to be waiting for the other party to broach the subject.23 All of these factors result in delays in the treatment of childhood obesity, which has evident repercussions on the current and future health of affected children.
Thus, understanding the factors at play in the approach to childhood overweight and obesity is essential to be able to offer the best possible support to families in the search of the solution to this important public health problem. Therefore, the objective of our study was to describe the attitudes and feelings of health care workers in discussing overweight and obesity in children with their parents, exploring perceived barriers and facilitators with the ultimate goal of providing effective care.
Sample and methodsWe conducted a qualitative study in paediatric health care workers (paediatricians and paediatric nurses) employed in primary care centres and hospitals in the island of Majorca (n = 320), who were informed of the purpose of the study and sent a semi-structured individual questionnaire developed based on the findings of a previous survey of paediatric nurses in Sweden.16 The items were developed to assess the experiences and feelings of paediatric health care staff in addressing the presence of childhood overweight and obesity with parents and children and the barriers and facilitators they perceived in the management of childhood obesity. Workers that chose to participate (n = 57; 68% female) submitted the completed questionnaires by email to the 3 authors detailed in the Author contributions section. We also collected data on the sociodemographic characteristics, professional category and years of experience of participants (paediatrician or nurse), the type of community (rural or urban) and care setting (primary care or hospital) where respondents worked, the age range of the children they referred to in their responses and the degree of overweight or obesity of these patients based on the International Obesity Task Force (IOTF) criteria,24 and the educational attainment of their parents (primary education or no formal education, vocational training, secondary education, university degree).
The study adhered to the principles of the Declaration of Helsinki, and all procedures were approved by the Clinical Research Ethics Committee of the Balearic Islands (Palma de Mallorca, ref. IB/3814/18PI). Paediatric health care workers provided informed consent to participation on completing the questionnaire.
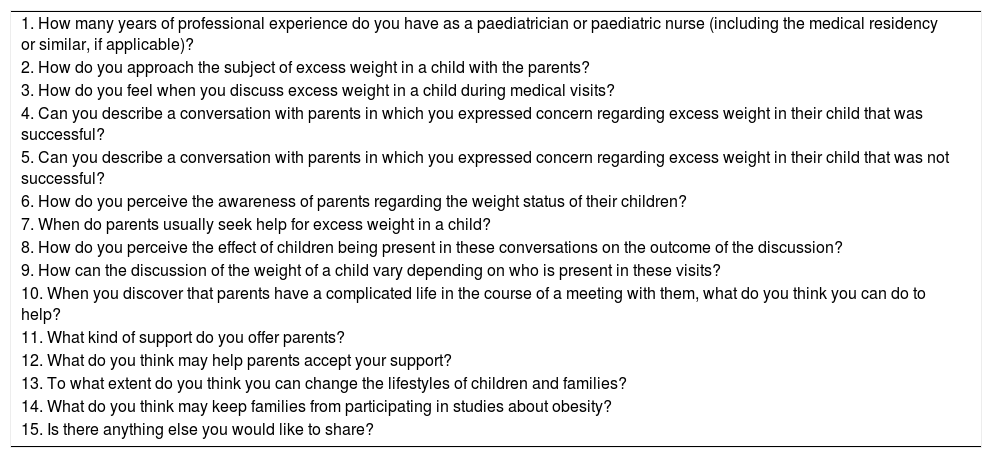
Thematic analysisTable 1 presents the text and subjects addressed in the semi-structured questionnaire. We performed a thematic analysis of the responses,25 a method used to identify, organise and describe different ideas contained in qualitative datasets. Themes represent important common elements in the responses of surveyed individuals and reveal patterns in the data that allow their description and interpretation. Thus, we coded questionnaire contents with an inductive approach and without the bounds of a pre-set coding system. The responses we received (text extracts relevant to the research questions) allowed us to identify specific issues and assign codes or concepts inferred from these extracts, for which purpose we only assigned codes to concepts expressed by at least 40% of participants. We grouped codes in different subthemes and themes based on the semantic similarity of the concepts they represented. The reporting of the findings adhered to the Consolidated Criteria for Reporting Qualitative Research (COREQ)26 (see Appendix B, supplemental material).
Semi-structured questionnaire completed individually by each paediatric health care worker.
| 1. How many years of professional experience do you have as a paediatrician or paediatric nurse (including the medical residency or similar, if applicable)? |
| 2. How do you approach the subject of excess weight in a child with the parents? |
| 3. How do you feel when you discuss excess weight in a child during medical visits? |
| 4. Can you describe a conversation with parents in which you expressed concern regarding excess weight in their child that was successful? |
| 5. Can you describe a conversation with parents in which you expressed concern regarding excess weight in their child that was not successful? |
| 6. How do you perceive the awareness of parents regarding the weight status of their children? |
| 7. When do parents usually seek help for excess weight in a child? |
| 8. How do you perceive the effect of children being present in these conversations on the outcome of the discussion? |
| 9. How can the discussion of the weight of a child vary depending on who is present in these visits? |
| 10. When you discover that parents have a complicated life in the course of a meeting with them, what do you think you can do to help? |
| 11. What kind of support do you offer parents? |
| 12. What do you think may help parents accept your support? |
| 13. To what extent do you think you can change the lifestyles of children and families? |
| 14. What do you think may keep families from participating in studies about obesity? |
| 15. Is there anything else you would like to share? |
We have expressed parametric data as mean and standard deviation (SD) and analysed the contents of the semi-structured questionnaire by means of the χ2 test with the statistical software SPSS, version 25 (SPSS Inc., Chicago, IL, USA).
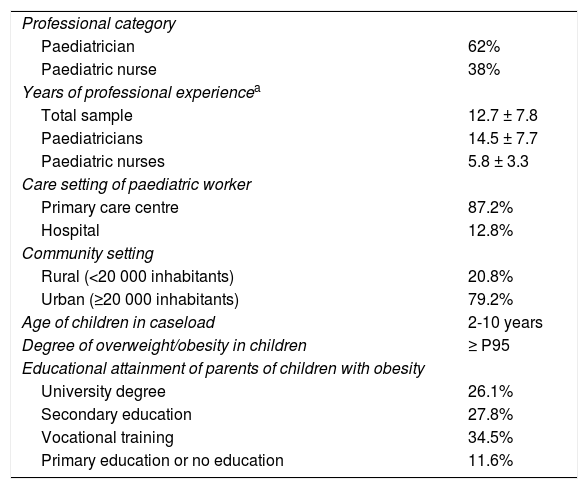
ResultsThe surveyed health care workers (62% paediatricians and 38% paediatric nurses) had worked in paediatric care settings for a mean of 12.7 years (SD, ±7.8), with a slightly longer experience in paediatricians compared to nurses. Table 2 presents the sociodemographic characteristics of the respondents. The community setting where the paediatric care teams conducted their work was urban (population ≥20 000 inhabitants) in 79.2% of cases and rural (population <20 000 inhabitants) in 20.8%. Most respondents worked in primary care centres (87.2% of the total). The age of the children that respondents referred to ranged from 2 to 10 years, and in every case these patients had a body mass index (BMI) at or above the 95th percentile. Many fathers and mothers had an educational attainment at the primary education or vocational education level.
Sociodemographic characteristics of respondents (n = 57).
| Professional category | |
| Paediatrician | 62% |
| Paediatric nurse | 38% |
| Years of professional experiencea | |
| Total sample | 12.7 ± 7.8 |
| Paediatricians | 14.5 ± 7.7 |
| Paediatric nurses | 5.8 ± 3.3 |
| Care setting of paediatric worker | |
| Primary care centre | 87.2% |
| Hospital | 12.8% |
| Community setting | |
| Rural (<20 000 inhabitants) | 20.8% |
| Urban (≥20 000 inhabitants) | 79.2% |
| Age of children in caseload | 2-10 years |
| Degree of overweight/obesity in children | ≥ P95 |
| Educational attainment of parents of children with obesity | |
| University degree | 26.1% |
| Secondary education | 27.8% |
| Vocational training | 34.5% |
| Primary education or no education | 11.6% |
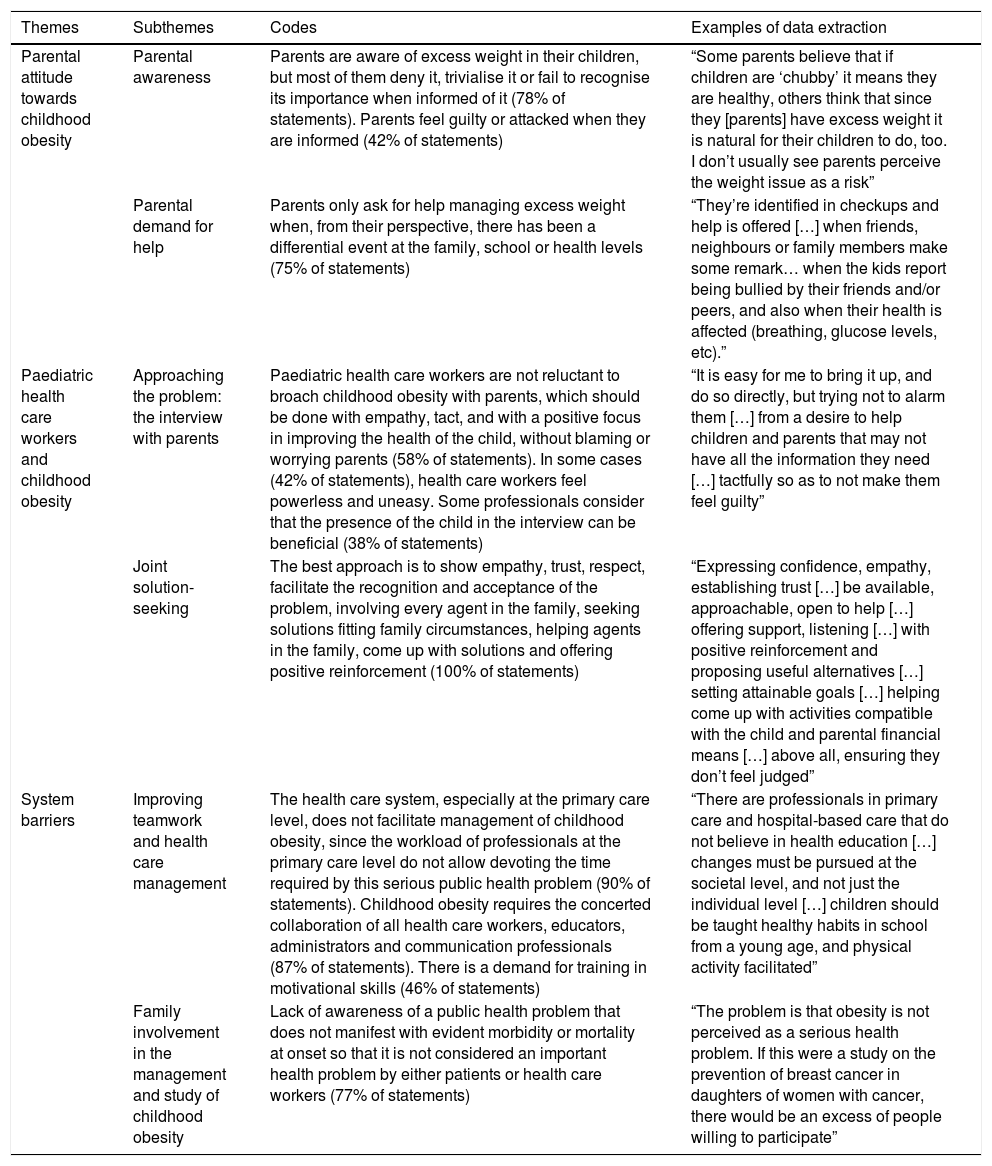
We identified three main broad themes in the perceptions of the paediatric health care workers that responded regarding their approach to childhood overweigh or obesity in their clinical practice (Table 3): (1) The attitude of parents toward excess weight in children; (2) paediatric health care workers and childhood obesity; and (3) system barriers. Overall, these themes coincided with the dimensions/main topics of the semi-structured questionnaire, although the themes were not restricted to a present coding scheme.
Thematic analysis.
| Themes | Subthemes | Codes | Examples of data extraction |
|---|---|---|---|
| Parental attitude towards childhood obesity | Parental awareness | Parents are aware of excess weight in their children, but most of them deny it, trivialise it or fail to recognise its importance when informed of it (78% of statements). Parents feel guilty or attacked when they are informed (42% of statements) | “Some parents believe that if children are ‘chubby’ it means they are healthy, others think that since they [parents] have excess weight it is natural for their children to do, too. I don’t usually see parents perceive the weight issue as a risk” |
| Parental demand for help | Parents only ask for help managing excess weight when, from their perspective, there has been a differential event at the family, school or health levels (75% of statements) | “They’re identified in checkups and help is offered […] when friends, neighbours or family members make some remark… when the kids report being bullied by their friends and/or peers, and also when their health is affected (breathing, glucose levels, etc).” | |
| Paediatric health care workers and childhood obesity | Approaching the problem: the interview with parents | Paediatric health care workers are not reluctant to broach childhood obesity with parents, which should be done with empathy, tact, and with a positive focus in improving the health of the child, without blaming or worrying parents (58% of statements). In some cases (42% of statements), health care workers feel powerless and uneasy. Some professionals consider that the presence of the child in the interview can be beneficial (38% of statements) | “It is easy for me to bring it up, and do so directly, but trying not to alarm them […] from a desire to help children and parents that may not have all the information they need […] tactfully so as to not make them feel guilty” |
| Joint solution-seeking | The best approach is to show empathy, trust, respect, facilitate the recognition and acceptance of the problem, involving every agent in the family, seeking solutions fitting family circumstances, helping agents in the family, come up with solutions and offering positive reinforcement (100% of statements) | “Expressing confidence, empathy, establishing trust […] be available, approachable, open to help […] offering support, listening […] with positive reinforcement and proposing useful alternatives […] setting attainable goals […] helping come up with activities compatible with the child and parental financial means […] above all, ensuring they don’t feel judged” | |
| System barriers | Improving teamwork and health care management | The health care system, especially at the primary care level, does not facilitate management of childhood obesity, since the workload of professionals at the primary care level do not allow devoting the time required by this serious public health problem (90% of statements). Childhood obesity requires the concerted collaboration of all health care workers, educators, administrators and communication professionals (87% of statements). There is a demand for training in motivational skills (46% of statements) | “There are professionals in primary care and hospital-based care that do not believe in health education […] changes must be pursued at the societal level, and not just the individual level […] children should be taught healthy habits in school from a young age, and physical activity facilitated” |
| Family involvement in the management and study of childhood obesity | Lack of awareness of a public health problem that does not manifest with evident morbidity or mortality at onset so that it is not considered an important health problem by either patients or health care workers (77% of statements) | “The problem is that obesity is not perceived as a serious health problem. If this were a study on the prevention of breast cancer in daughters of women with cancer, there would be an excess of people willing to participate” |
Most respondents stated that parents could perceive obesity in their children, but were in denial of it. The different aspects (codes) related to this theme were classified into 2 subthemes: “parental awareness” and “parental demand for help”.
Parental awarenessMost surveyed paediatric health care workers stated that most parents were fully aware of excess weight in their children, but were in denial of it, trivialised it or did not consider it important (78% of statements) or felt guilty or attacked when informed about excess weight in their children (42% of statements). This response stemmed from parents being confronted with the failure of the care they had devoted their children with the best of intentions, which produced a state of denial or numbness. In parents that had excess weight themselves, this response was intensified. In addition, parents generally considered the excess weight as a sign of health. Some representative examples of the extract are:
“If the subject is not brought up the right way, parents feel guilty, as they believe that they have been doing what is best for their children” (Respondent [R] 1; referred to from this point as R1). “I think that there are 2 kinds of parents: those that are very worried, and those that deny the problem; in general, the second group corresponds to parents with more excess weight” (R4). “Parents often associate weight with being healthy or strong and the self-perception of good care” (R12).
Some respondents (25% of statements) noted that parents tended to exhibit much more concern when their children were thin as opposed to overweight, as carrying a few extra pounds was rather perceived as a sign of good health. This attitude changed based on parental educational attainment, as the lower the attainment, the more likely they were to deny or minimise excess weight or even to perceive it as a source of pride. The following sentence is a good example: “There are parents of overweight children that say that their kids are all right and that they barely eat, others that say that the child has an adequate weight, but does not exercise, and is chubby, has a bit of a belly, is a bit flabby…Others (a minority) are more realistic. It all depends to a great extent on the physical condition of the parents, the level of overprotection of their children, their educational level and the family lifestyle (which they consider normal)” (R19).
Parents do not usually seek help for excess weight in their children except when a differential event takes place (75% of statements). This event may consist of parents noticing pronounced weight gain in their children after a routine checkup or some type of health problem (difficulty breathing, especially after physical activity, or hyperglycaemia) or, in most cases, comments from relatives or friends or episodes of bullying at school or in the peer group of the child, especially in preadolescents. If the message came from more than one source, parents were more likely to seek and accept the help of the paediatric care team. Some examples of the most representative sentences in the data extraction process were: “When something happens in school (for instance, someone has told them something), when children express their aversion…” (R3). “They rarely come. It usually happens when there is an abrupt change in weight” (R5). “It commonly happens when a member of the family has excess weight and has a serious health problem, other times because children comment that they come at them, so the dimension of the problem changes, it is not the weight itself, but the consequences of obesity that children start to experience” (R6). “Usually it is in preadolescent kids, when we measure the weight and fear it may be the tendency seen in the future. Other times they are anxious about food or engage in secretive eating, or other people are told that the child is obese” (R22).
Other times, the search for help was motivated by observations made by the parents themselves, for instance, noticing episodes of anxiety in the child related to food, that the self-esteem of the child was being affected or that they were overwhelmed in their attempt to manage the excess weight problem. The following sentence provides an example: “When they are overwhelmed by the situation, for instance, due to problems secondary to obesity, anxiety associated with eating, etc” (R20).
This section explored how paediatric care teams broached the subject of childhood obesity with parents. The codes were classified into 2 subthemes: “approach to the problem: the interview with the parents” and “joint solution-seeking”.
Approach to the problem: the interview with parentsFifty-eight percent of paediatric health care workers reported they usually had no problems openly addressing the issue of overweight or obesity in a child with the parents or caregivers; each case is a challenge they are willing to take on and always with the intention of helping parents and children. The subject is brought up with empathy and tact, from a positive angle emphasising the improvement of the child’s health and facilitating engagement in the issue, trying not to create guilt or anxiety. A representative sentence in data extraction was: “I don’t have an issue discussing obesity, but I try to use euphemisms (depending on the case) so that they do not feel ‘attacked’, because in my experience, referring bluntly to obesity may alienate the family” (R23).
Twenty-one percent of paediatric professionals approach the issue of overweight and obesity mainly based on body weight and reference growth charts, trying to make parents aware of the potential impact in their child’s health of maintaining a healthy weight. The following is an example of a representative sentence in the extract: “After assigning a child an excess weight category based on the percentile table, I explain to the family that the child has excess weight and its potential impact on present and future health, and try to go over the dietary patterns, physical activity…” (R21).
Sometimes (42% of statements), paediatric health care workers feel powerless due to how awkward and difficult it is to bring up the subject, as parents are yet unaware of the problem and become upset and stuck in facing the issue. Some of the most representative sentences in the extract were: “One mother came to the office for a different reason, and when she was told that her child was in the high percentile range, she felt offended that we were calling her child fat” (R11). “It’s harder, because there are parents that are not aware that the child has excess weight and may even consider their weight healthy, so approaching these cases may be really complicated. Some parents are even offended when they’re told their child has excess weight. However, there are other cases in which parents themselves consult about their child’s weight, and then it is easier to manage” (R14).
These attitudes in parents or caregivers do not in any way contradict the open and positive attitude manifested by paediatric health care workers in their approach to the problem.
Some health professionals (38% of statements) considered that the presence of children in the interview had a positive effect, as they could be actively involved and propose solutions to the problem; however, their presence could also have a negative impact on the interview, either by generating tension or by inhibiting free expression in parents and children, possibly introducing or exacerbating guilt in the child or blaming the child. In any case, it is important to avoid using jargon the child cannot understand and, above all, hurting the child’s self-esteem. Some representative sentences in the extract were: “There are parents who try to conceal things by speaking lower, whispering answers, winking. Others blame their children in front of the health care staff and make them feel really bad, it impacts their self-esteem above all” (R3). “Sometimes you can tell that the child is uncomfortable, and other times you see that the child is actively engaged in the conversation and suggests small changes that he or she could make” (R20).
The optimal attitude described by paediatric health care workers (100% of statements) that managed children with excess weight involved empathy, trust, respect, a lack of superiority, support and active listening, communicating without judgment or pressure, without forbidding or blaming, to promote awareness and acceptance of the problem, involving every agent in the family and, above all, helping them come up with possible solutions and offering positive reinforcement to their suggestions. Respondents considered addressing the individual responsible for shopping and cooking in the household essential. When all these aspects were fulfilled, management could be successful. The following are examples of the most representative sentences in the extract: “I think that empathy, respect, establishing a horizontal communication pattern rather than presenting ourselves as being in charge, can also be helpful in working with caregivers” (R15). “The presence of the adult that lives with the child, or primary caregiver, who plans and prepares the main meals of the day, is important” (R22). “Changing lifestyle habits is very difficult, and are only possible with adequate motivation and positive reinforcement. From the clinic, we can offer support and provide that positive reinforcement, but the motivation of patients and families is key” (R23).
Most surveyed paediatric care workers highlighted the organizational barriers in the health care system, including the limited time allotted to visits, the insufficient cooperation with other health professionals and the lack of family involvement. We classified the different aspects on this topic (codes) into 2 subthemes: “improving teamwork and health care management” and “family involvement in the management and study of childhood obesity”.
Improving teamwork and health care managementThe health care system, especially at the primary care level, does not facilitate the management of childhood obesity. The large caseloads at this level keep paediatric health care workers from devoting the time required by this serious public health problem (90% of statements). Since childhood obesity is a global problem, 87% of surveyed paediatric health care workers believe that its solution requires the participation of other health professionals (endocrinologists, family physicians, nurses, dietitians-nutritionists, pharmacists, etc), educators, managers and the mass media. The following are some of the most representative sentences used in data extraction: “We need more educational resources, and more stringent regulation on food products and related advertising” (R9). “It is important that we continue working on this issue and involve all of society (health care facilities, schools, towns…) to tackle this problem from every possible angle and work together” (R11).
Since the trust of patients and families in paediatric health care workers is essential, these professionals (46% of statements) demand more training, not on clinical knowledge but rather on motivational skills. One of the most representative sentences used in data extraction was: “In this century, health professionals should know how to perform motivational interviewing, we should know how to investigate and address social determinants of health in these patients, because that is where 80% of the health problems of individuals concentrates, something that is much more evident when it comes to childhood overweight and obesity. Primary care is meant to be comprehensive, and our job is to work on everything surrounding our patients” (R15).
In addition, 10% of paediatrics professionals believed that developing complementary activities in health care centres or coordinating such activities from those sites would also be essential. The following are some of the most representative sentences used in data extraction: “Children must be taught, from an early age, about healthy habits at school, in addition to facilitating physical activity” (R20). “Aware of the poor dietary habits, and motivated by this problem, we have been developing ‘healthy breakfasts’ in schools for years, which has eventually evolved into a ‘healthy day’, but also involving parents in these activities, although it is hard for them to attend” (R21).
Seventy-seven percent of respondents stated that the lack of awareness about childhood obesity, a health care problem that, given that it does not immediately manifest with clear morbidity and is not directly associated with mortality, is not considered a serious health problem by patients (parents/caregivers and children/adolescents) or health professionals. In addition, 25% of respondents considered that the cultural level of the family was an important determinant, as a higher educational attainment corresponded to greater involvement and willingness to act. Some of the most representative sentences in the extract were: “There is little awareness of this problem in Spain, not only in patients but also in the health care community, and there are also social and economic barriers due to their direct and indirect impact” (R1). “The educational level of families is very important” (R7).
In addition, 38% of surveyed professionals considered that it was individuals with more severe degrees of excess weight that were the least likely to acknowledge it. Making lifestyle changes is difficult for families, mainly for reasons related to family organization and logistics, such as parents or caregivers not having time. The following was the most representative sentence about this aspect in the extract: “This requires additional involvement, due to time and logistics constraints. It is very difficult for parents of young children to find the time to attend medical visits or meetings on a regular basis. This is especially the case if they do not have someone with whom they can leave the children or work with. Making it possible to bring the children to these meetings, making the logistics easier, could help a great deal” (R5).
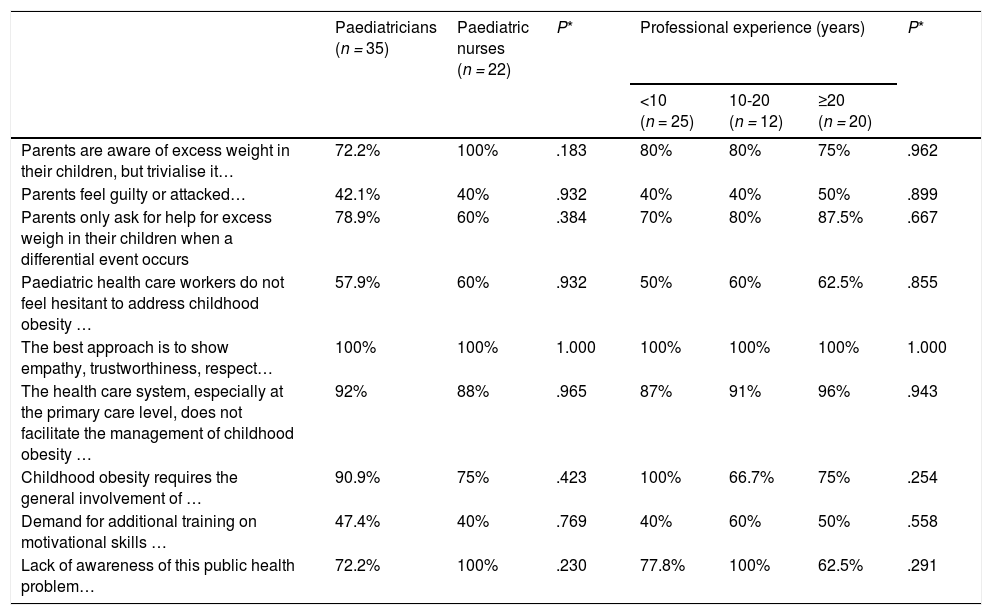
We did not find differences based on type of professional (paediatrician vs paediatric nurse) or the years of professional experience (Table 4).
Codes by professional category and years of professional experience.
| Paediatricians (n = 35) | Paediatric nurses (n = 22) | P* | Professional experience (years) | P* | |||
|---|---|---|---|---|---|---|---|
| <10 (n = 25) | 10-20 (n = 12) | ≥20 (n = 20) | |||||
| Parents are aware of excess weight in their children, but trivialise it… | 72.2% | 100% | .183 | 80% | 80% | 75% | .962 |
| Parents feel guilty or attacked… | 42.1% | 40% | .932 | 40% | 40% | 50% | .899 |
| Parents only ask for help for excess weigh in their children when a differential event occurs | 78.9% | 60% | .384 | 70% | 80% | 87.5% | .667 |
| Paediatric health care workers do not feel hesitant to address childhood obesity … | 57.9% | 60% | .932 | 50% | 60% | 62.5% | .855 |
| The best approach is to show empathy, trustworthiness, respect… | 100% | 100% | 1.000 | 100% | 100% | 100% | 1.000 |
| The health care system, especially at the primary care level, does not facilitate the management of childhood obesity … | 92% | 88% | .965 | 87% | 91% | 96% | .943 |
| Childhood obesity requires the general involvement of … | 90.9% | 75% | .423 | 100% | 66.7% | 75% | .254 |
| Demand for additional training on motivational skills … | 47.4% | 40% | .769 | 40% | 60% | 50% | .558 |
| Lack of awareness of this public health problem… | 72.2% | 100% | .230 | 77.8% | 100% | 62.5% | .291 |
Our study explored the attitude and feelings of paediatric health care workers as regards childhood obesity, a serious public health problem that is not sidestepped by paediatric health professionals, but confronted openly, despite their awareness of the complexity of its management and the limited tools they have available to address it.
The survey of paediatric health care workers allowed us to identify 3 broad themes: “parental attitude toward obesity in their children” (subthemes: “parental awareness”, “parental demand for help”), “paediatric health workers and childhood obesity” (subthemes: “approach to the problem: the interview with parents” and “joint solution-seeking”) and “system barriers” (subthemes: “improving teamwork and health care management”, “family involvement in the management and study of childhood obesity”). We found that addressing childhood obesity is no easy task, as it requires that parents be aware of the problem and, above all, the establishment of rapport between the paediatric care team and patients and their families. In turn, both aspects may be influenced by many other factors, such as parental educational attainment, the structural situation of families and external conditions, such as parents or caregivers lacking time or the difficulty of introducing changes in household habits, and the health care and motivational skills of paediatric health care workers.
Parental awareness of the problem. The failure of parents or children to recognise excess weight is one of the main barriers to the management and resolution of childhood overweight and obesity.12,27–32 Previous studies have demonstrated that parents tend to underestimate their children’s weight,14,33 especially parents with excess weight12,32 and parents of young children,34 which contributes to the neglect of excess weight in children.32 There is evidence that 70.8% of children and 64.9% of parents in Spain do not generally perceive excess weight as a health problem.35 This denial may also stem from feelings of guilt for not knowing how to adequately care for the child, a fear of being judged by others36 or the stigma associated with excess weight that may affect both them and their children.19–21 When parents notice excess weight in their children, they tend not to worry, as it is more likely to become a problem when they reach school age, mainly on account of potential bullying or social exclusion.32,37 Parents and children accept help from health professionals after their concerns related to the excess weight reach a certain threshold.38 Motivating patients and families should be one of the first steps taken by paediatric care teams and is actually the first medical intervention required to successfully treat excess weight in children.12,32
Addressing the problem. Once trust between parents/children and the paediatric care team has been established, respondents considered important to show respect, refraining from authoritarian attitudes, offer support and active listening listening, without judging, scaring, prohibiting or blaming to facilitate the recognition and acceptance of the problem, adapting to the circumstances and health literacy of the family and offering different options, establishing short-term and attainable goals, and allowing parents to come up with possible solutions. Effective communication between the paediatric care team and parents and children is the cornerstone of treatment of childhood obesity12,39 that make it possible for the usual interventions (changes in diet and lifestyles habits, promotion of physical activity, changes in family habits, reduction of sedentary activity) to be truly effective, as they will have served to establish rapport with parents and children, overcoming the usual social and family-related barriers (lack of motivation, lack of involvement in management, blaming or mutual blaming of parents/children, quitting).12,35 It is also important to identify and speak to the person responsible for shopping and cooking in the household, as the diet of the child and family depends on this person. Approximately one third of paediatricians believed that children should be present in the conversations, even if it means that the discussion is less smooth or its contents get narrowed down, as they can come up with solutions and, in doing so, become more motivated to improve their weight.
How do paediatric health care workers feel? The sensitive nature of excess weight in children makes many professionals uncomfortable in broaching the subject, which is consistent with the findings of previous qualitative research.12,17 However, most of the health care workers surveyed in our study reported feeling comfortable and confident, no hesitation to bring up the subject and considerable willingness to intervene, mainly on account of their health care skills, which was consistent with the previous literature12,35,40 showing that previous training of paediatric care teams on the subject of obesity was essential to address this problem and overcome barriers. This attitude of paediatric health care workers in Spain, who feel capable of approaching this problem, stands in contrast to the findings in other countries, where professionals wait for the other party to bring up the subject of excess weight in children.16 Our findings also differ compared to those of another study conducted in Spain in 2008 in which 28.7% of professionals reported having little experience in the management of obesity,35 something that could be explained by the fact that the risk factors for obesity, both at the individual and social levels, have since been well defined, and there are now treatment guidelines to apply.12,41 This knowledge has been documented extensively and is available to paediatric health care workers in Spain. The adequate training of Spanish paediatric care staff differs substantially from the situation described by paediatric care workers in Sweden, where paediatric nurses, the professionals who are usually in charge of managing and monitoring children with overweight or obesity, report deficient training on both obesity and communication and motivational skills,16 educational deficits that have also been described by paediatric care professionals in other countries, who have openly expressed the need to improve training on childhood obesity.42–44
However, both physicians and nurses agree on the need for training in motivational skills that would unquestionably facilitate the development of rapport between them and parents and children and above all reinforce trust, which, as we noted above, are essential to the success of therapeutic interventions in this area.12 Along these lines, our research group recently found that a multi-session programme for management of preschool-age children with obesity that applied motivational techniques improved both the attitude of parents in relation to overweight and obesity in their children and the lifestyle and habits of children toward healthier patterns, while also achieving significant reductions in the BMI of the children.45,46 Other studies conducted in Australia, although not in the early childhood period, had similar outcomes, although with a lesser reduction in BMI.47,48
Improving the system. Despite the excellent disposition and qualifications for care delivery of paediatric health care workers, the system does not facilitate the management of childhood obesity. The health care system is a barrier in itself, due to the lack of time and excessive workloads of paediatric health care staff, the lack of educational materials, the limited access to specialists, the lack of collaboration with other health care professionals and the lack of awareness on the part of administrators of the importance of the problem.35 Still, the health care system cannot fight childhood obesity in isolation, as this is a global problem that requires the involvement of all social agents, including the education system, the administration and the mass media, as established in the official Strategy for Nutrition, Physical Activity and Obesity Prevention (NAOS).49 Therefore, the need to develop complementary activities as an intrinsic part of paediatric care must be acknowledged and efforts toward that end redoubled, so that they are integrated in primary care delivery with the collaboration of other social agents, such as teachers, exercise and sports professionals (individual or group coaching) and the mass media. In addition, health care administrations should encourage, facilitate and improve the participation of paediatric health professionals in studies on childhood obesity with the involvement of parents and caregivers, which would undoubtedly improve our knowledge of the effectiveness of therapeutic interventions used for management of obesity and also increase social awareness of this important public health problem, as lack of awareness is one of the greatest barriers faced by paediatric health care workers in their approach to the management of childhood obesity.
Lastly, we ought to comment on the homogeneity of the perceptions and attitudes of paediatric health care workers, independently of their professional category and their years of experience.
Strengths and limitations. This is one of the few studies conducted in Spain on the attitudes and perceptions of paediatric health care workers regarding childhood obesity and related barriers and conditions. A second strength is that since the questionnaire used consisted of open-ended questions, participants were able to explain their personal perspective on the issue without restrictions. A third strength was the methodological approach, thematic analysis, a flexible method that allows the systematic analysis and interpretation of large amounts of data, 25 including a careful analysis of the questionnaire responses, data extraction and subsequent discussion until a consensus is reached for definition of thematic categories and perceptions. Another strength is that we have contributed to the published evidence on the communication between paediatric health care workers and the parents or caregivers of children with excess weight, which is generally relevant. Among the limitations of the study were those intrinsic to its qualitative methodology, although the number of interviews performed (n = 57) exceeded the minimum established as necessary to achieve an integral understanding of the subject of interest (n = 16) but did not result in an excessively large amount of data, which would have made an exhaustive analysis difficult.50,51 Another limitation is the geographical scope of the study, as it was limited to the island of Mallorca, due to which the extrapolation of the data would require performance of additional studies with the same exact methodology in other areas. Yet another is that the health care workers that chose to participate may have been those most interested in childhood obesity, so that the sample may not be representative. We also did not investigate variables related to clinical practice, as that was not the objective of the study.
ConclusionsPaediatric health care workers feel confident in approaching childhood obesity, as they have been trained to manage this problem, although motivational skills are also required, for it is essential that parents recognise the problem and, above all, that good rapport is established between health care workers and parents/children. Effective communication between the paediatric care team and parents and children is the foundation of the management of childhood obesity and necessary for applied interventions to be effective. The health care system poses barriers to the activity of paediatric care teams that must be addressed.
FundingThis study was conducted in the framework of the STOP project (The Science and Technology in Childhood Obesity Policy) funded by the Horizon 2020 research and innovation programmeof the European Commission (ref. 774548), and the health care research fund(Fondo de Investigación en Salud, FIS) of the Instituto de Salud Carlos III through the Department of Health, cofunded by the European Regional Development Fund(ERDF) through project PI17/01827 and the CIBEROBN research network (CB12/03/30038), as well as competitive research grants including grant 35/2011 from the Government of the Balearic Islands and the European Cooperation in Science and Technology(EU-COST) programme (COST action CA16112). CB received a Fernando Tarongí Bauzàdoctoral grant. The above funding institutions were not involved in the design of the study, data collection and analysis or the writing of the manuscript.
Author contributionsEA, CB and JAT contacted paediatric care teams with the collaboration of all other authors, carried out the interviews and contributed to their analysis. EA, CB and JAT wrote the initial draft of the manuscript. All authors reviewed and approved the final manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank paediatric teams for their participation in the interviews.
Please cite this article as: Argelich E, Alemany ME, Amengual-Miralles B, Argüelles R, Bandiera D, Barceló MA, et al. Los equipos de pediatría ante la obesidad infantil: un estudio cualitativo dentro del proyecto STOP. An Pediatr (Barc). 2021;95:174–185.