In recent years, the increasing demand for dermatological consultations in the Emergency Department has resulted in the publication of a variety of studies on this subject. However, most of them deal with the general population, without taking into account the changes in frequencies found in young children (ages 0–14).
ObjectivesTo determine the frequency of various dermatological diagnoses made by the on-call paediatrician in the Emergency Department, and after referral to paediatric dermatology.
Materials and methodsFirstly, a descriptive retrospective study was performed that included all patients aged between 0 and 14 years old who were seen after being referred to the emergency paediatric dermatologist by the on-call paediatrician from June 2010 to December 2013. Secondly, an analytical study was carried out by calculating the kappa index calculus, in order to establish the diagnostic concordance between the emergency paediatrician and the paediatric dermatologist.
ResultsA total of 861 patients, with a mean age of 4.5 years were included. More than half of the skin disorders analysed were eczema (27%) and infections (26%). The five main diagnoses were: atopic dermatitis (16%), acute prurigo simplex (5%), tinea (5%), pyogenic granuloma (4%), and molluscum contagiosum (4%). Additional tests were only required in 16% of the cases. The kappa index obtained was 0.206 (95% CI: 0.170–0.241).
ConclusionsThe dermatology consultations in the Emergency Department were shown to be frequent and mostly involved minor diseases. Collaboration between paediatricians and dermatologists resulted in a high treatment success rate, leading to a low percentage of additional tests required and a high rate of discharges.
En los últimos años, la elevada demanda de asistencia en los servicios de urgencias por enfermedad cutánea ha motivado la realización de diversos estudios al respecto. Sin embargo, la mayoría están referidos a población general, sin tener en cuenta las modificaciones en las frecuencias de las enfermedades que se producen en edad pediátrica.
ObjetivosDeterminar la frecuencia de los distintos diagnósticos dermatológicos derivados por el pediatra de guardia y atendidos en la consulta de dermatología pediátrica urgente.
Material y métodosEstudio retrospectivo descriptivo que incluyó todos los pacientes de 0 a 14 años atendidos tras citación por el pediatra de guardia en las consultas de dermatología infantil urgente desde junio de 2010 hasta diciembre de 2013. En segundo lugar, se realizó un estudio analítico que consistía en el cálculo del índice kappa para establecer la concordancia diagnóstica entre el diagnóstico del pediatra de Urgencias y el de Dermatología.
ResultadosSe atendió a un total de 861 pacientes con una edad media de 4,5 años. Más de la mitad de toda la enfermedad atendida se debió a eccemas (27%) e infecciones (26%). Los 5 diagnósticos principales fueron: dermatitis atópica (16%), prurigo simple agudo (5%), tiña (5%), granuloma piógeno (4%) y molluscum contagiosum (4%). Solo en un 16% de los casos se solicitaron pruebas complementarias. El índice kappa obtenido fue de 0,206 (IC 95%: 0,170-0,241).
ConclusionesLas consultas en urgencias pediátricas por motivos dermatológicos son frecuentes y gran parte está motivada por enfermedad banal. La colaboración entre pediatras y dermatólogos permitió una alta capacidad resolutiva, lo que se tradujo en un bajo porcentaje de pruebas complementarias solicitadas y un elevado número de altas directas.
In the last years, several studies have been published on dermatological emergencies in our area, all except one concerning the general population.1–8 The increasing interest in this issue is mainly derived from the progressive increase in the demand for assistance in hospital emergency services, up to the point that an annual increase of 10–20% is calculated for emergency assistance.9,10
This growth is mainly due to minor diseases. At the same time, emergency dermatological cases have not been the exception to that increasing trend. It is estimated that the emergency dermatological demand represents 8–10% of the total emergency cases at a general hospital, and up to 10.2% in the paediatric population.11,12
The main factors involved in this improper use of hospital emergencies are the lack of trust in primary care, lack of health education and waiting lists,9,13–15 with the added aspect in dermatology of the spectacular nature of skin signs and symptoms, which create huge anxiety in the patient or, more frequently during the paediatric age, their relatives.
The main goal of the study was to describe the profile of the user and determine the frequency of the various dermatological diagnoses referred by the paediatrician on duty and attended to the emergency paediatric dermatological office, since most prior studies refer to the general population1–8 and it is not possible to extrapolate the results to this subgroup, where we know there are changes in the frequencies of diagnoses.5 As a secondary goal, we aimed to analyse the resolution capacity of the dermatologist on duty, as well as the profitability of emergency paediatric dermatological consultation.
Materials and methodsThe study was carried out in a third-level hospital with 100 beds, 115 of those in the Children's Hospital, covering an area of 554,981 inhabitants, 16% of whom are the paediatric population.
This hospital has a dermatology resident on duty Mondays to Fridays to cover general dermatological emergencies, 3–8pm, and 2 days of the week, Mondays and Thursdays, with the help of a second resident (third or fourth year) for assistance at the dermatological emergency office, also 3–8pm. In this way, all patients 0–14 years old attending the Casualty Department for dermatological reasons are previously examined by the paediatrician on duty or paediatrics resident, who may, if necessary, call the dermatologist for urgent cases.
A retrospective study was designed based on the data collected from clinical records of all patients attending paediatric dermatological emergencies from June 2010 to December 2013, a total of 861 patients.
Emergency attendance sheets were reviewed as part of the work protocol when the patient is discharged and referred to dermatological emergencies, and the subsequent medical history at that consultation. The following data were gathered for each patient: name and surname, age, gender, date of attendance, supplementary evidence requested, destination upon discharge and diagnosis, both that of the paediatrician in the discharge report and the subsequent diagnosis by the Dermatology resident.
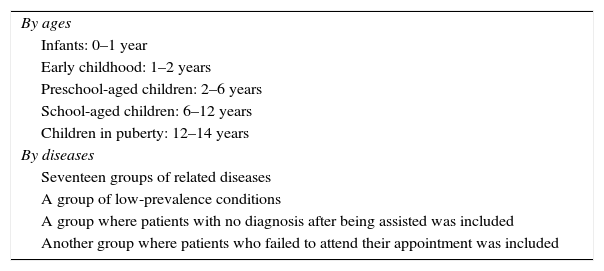
To facilitate the development of the study, the data were collected as stated in Table 1.
Grouping of data according to age and groups of diseases.
| By ages |
| Infants: 0–1 year |
| Early childhood: 1–2 years |
| Preschool-aged children: 2–6 years |
| School-aged children: 6–12 years |
| Children in puberty: 12–14 years |
| By diseases |
| Seventeen groups of related diseases |
| A group of low-prevalence conditions |
| A group where patients with no diagnosis after being assisted was included |
| Another group where patients who failed to attend their appointment was included |
First, a descriptive study of the observed characteristics of patients was carried out. For qualitative variables, the absolute frequency of each category and percentages were used; for quantitative variables, the mean, median, standard deviation and range were used. In contrast, if the quantitative variables followed a normal distribution, the Kolmogorov–Smirnov test was used. Secondly, an analytical study was carried out by preparing contingency tables and calculating the kappa index, to establish the diagnosis concordance between the diagnosis upon discharge previously issued at the General Paediatric Emergency Department and the dermatology diagnosis.
The statistical analysis was carried out using version 18.0 of the statistical software Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA). All confidence intervals calculated were at 95%, and all p values were calculated bilaterally, considering values below 0.05 as statistically significant.
ResultsDuring the period of the study, 861 patients were called to consultation, after excluding revisits (patients who attended again for the same reason they had been assessed for at the Casualty Department and the consultation at the Dermatological Emergency Department). A mean of 20 patients a month were attended to, observing a higher attendance volume during October (24.3 patients/month), April (24 patients/month) and May (24 patients/month).
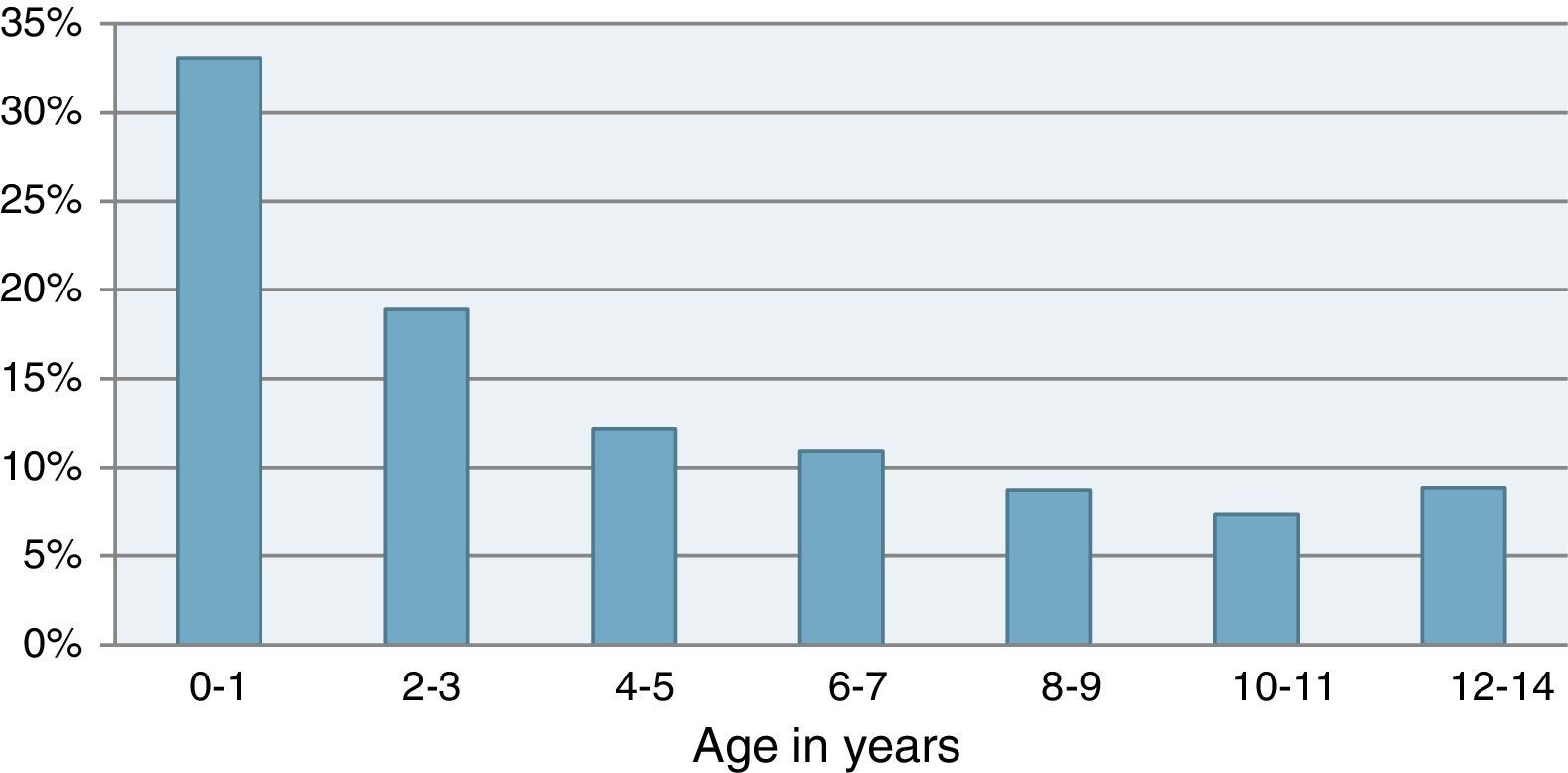
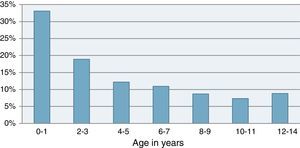
Of the 861 patients attended to, 466 (54%) were boys and 395 (46%) girls (there are no statistically significant differences). The mean age was 4.5±4 years, the median, 3 years, and the mode, 0 years (from birth to 11 months) (Fig. 1). Regarding the distribution by age groups, the population with the highest demand were pre-schoolers (31%), followed by school-aged children (27%), infants (18%), early childhood (15%) and lastly children in puberty (9%).
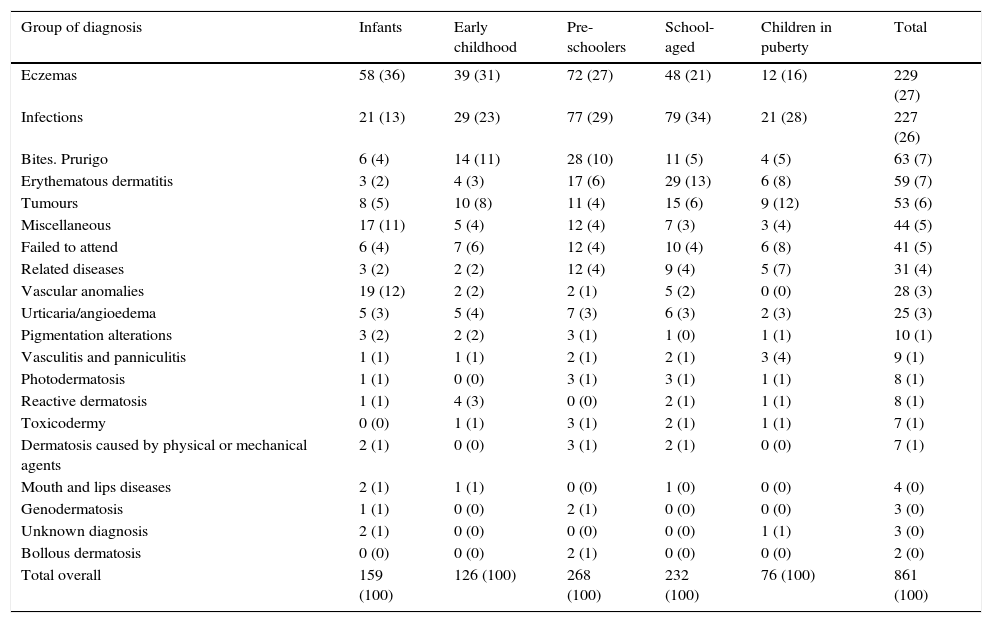
By diagnosis groups (Table 2), eczema (27%) and infections (26%) were the main reasons for consultation, together representing more than half the consultations. Following those in terms of frequency, erythematous dermatitis (7%), bites/prurigo simplex (7%), tumours (6%) and the miscellaneous group (5%). This last group included various diagnoses related to the paediatric age, such as mastocytosis, histiocytosis, enteropathic acrodermatitis and toxic erythema in the new-born. Forty-one patients (5%) did not attend their appointments at the Emergency Paediatric Dermatology Department and for three patients no diagnosis was issued after attendance.
Distribution of the groups of diseases according to age groups.
| Group of diagnosis | Infants | Early childhood | Pre-schoolers | School-aged | Children in puberty | Total |
|---|---|---|---|---|---|---|
| Eczemas | 58 (36) | 39 (31) | 72 (27) | 48 (21) | 12 (16) | 229 (27) |
| Infections | 21 (13) | 29 (23) | 77 (29) | 79 (34) | 21 (28) | 227 (26) |
| Bites. Prurigo | 6 (4) | 14 (11) | 28 (10) | 11 (5) | 4 (5) | 63 (7) |
| Erythematous dermatitis | 3 (2) | 4 (3) | 17 (6) | 29 (13) | 6 (8) | 59 (7) |
| Tumours | 8 (5) | 10 (8) | 11 (4) | 15 (6) | 9 (12) | 53 (6) |
| Miscellaneous | 17 (11) | 5 (4) | 12 (4) | 7 (3) | 3 (4) | 44 (5) |
| Failed to attend | 6 (4) | 7 (6) | 12 (4) | 10 (4) | 6 (8) | 41 (5) |
| Related diseases | 3 (2) | 2 (2) | 12 (4) | 9 (4) | 5 (7) | 31 (4) |
| Vascular anomalies | 19 (12) | 2 (2) | 2 (1) | 5 (2) | 0 (0) | 28 (3) |
| Urticaria/angioedema | 5 (3) | 5 (4) | 7 (3) | 6 (3) | 2 (3) | 25 (3) |
| Pigmentation alterations | 3 (2) | 2 (2) | 3 (1) | 1 (0) | 1 (1) | 10 (1) |
| Vasculitis and panniculitis | 1 (1) | 1 (1) | 2 (1) | 2 (1) | 3 (4) | 9 (1) |
| Photodermatosis | 1 (1) | 0 (0) | 3 (1) | 3 (1) | 1 (1) | 8 (1) |
| Reactive dermatosis | 1 (1) | 4 (3) | 0 (0) | 2 (1) | 1 (1) | 8 (1) |
| Toxicodermy | 0 (0) | 1 (1) | 3 (1) | 2 (1) | 1 (1) | 7 (1) |
| Dermatosis caused by physical or mechanical agents | 2 (1) | 0 (0) | 3 (1) | 2 (1) | 0 (0) | 7 (1) |
| Mouth and lips diseases | 2 (1) | 1 (1) | 0 (0) | 1 (0) | 0 (0) | 4 (0) |
| Genodermatosis | 1 (1) | 0 (0) | 2 (1) | 0 (0) | 0 (0) | 3 (0) |
| Unknown diagnosis | 2 (1) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 3 (0) |
| Bollous dermatosis | 0 (0) | 0 (0) | 2 (1) | 0 (0) | 0 (0) | 2 (0) |
| Total overall | 159 (100) | 126 (100) | 268 (100) | 232 (100) | 76 (100) | 861 (100) |
Data expressed as n (%).
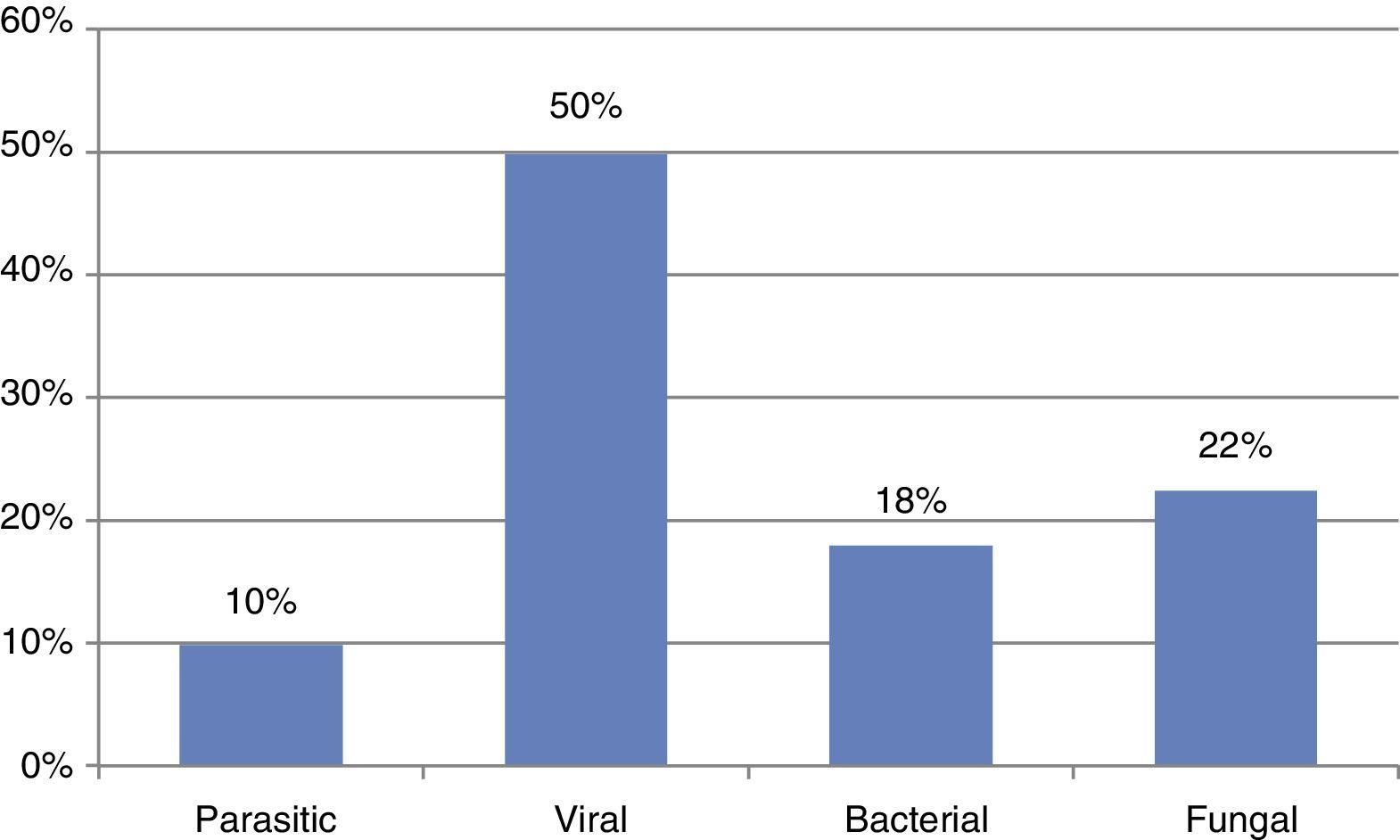
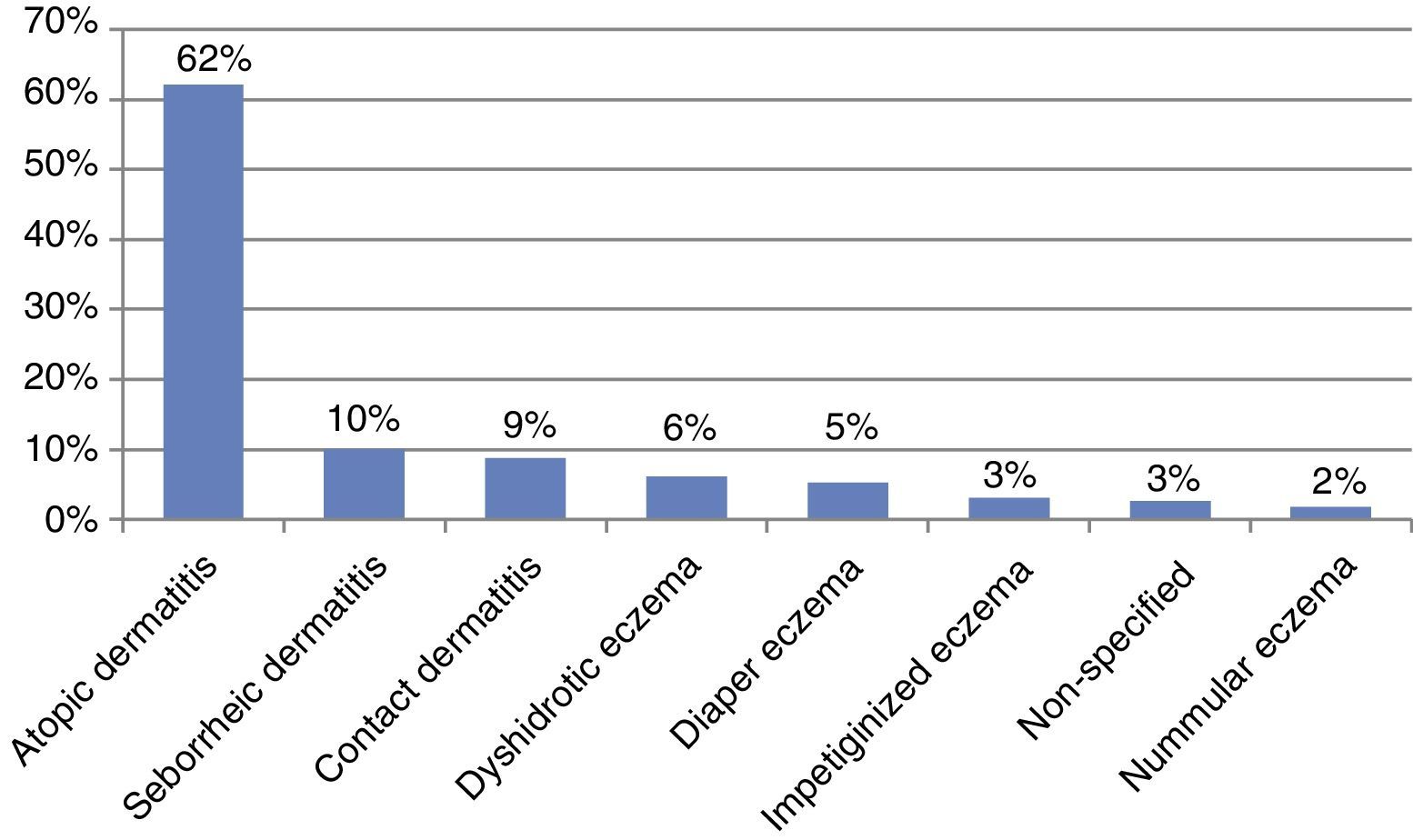
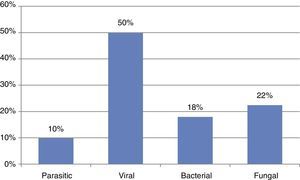
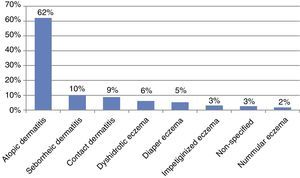
Within the infections group, 111 (50%) were of viral origin, 50 (22%) of fungal origin, 40 (18%) of bacterial origin, and, lastly, 22 (10%) of parasitic origin (Fig. 2), while in the eczema group, 141 (62%) were due to atopic dermatitis, followed in frequency by seborrheic dermatitis in 23 patients (10%) and contact dermatitis in 20 (9%) (Fig. 3).
As reflected in Table 2, these groups of diseases were also analysed based on the age groups, showing differences in the frequencies of the diseases within the different groups.
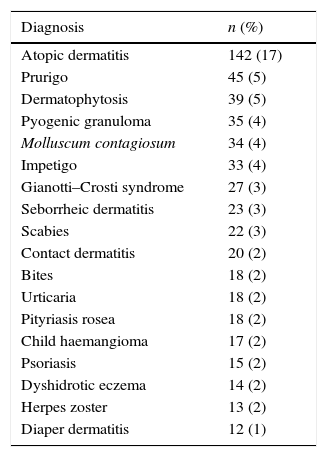
Regarding the diagnosis made, 66% of consultations were for 18 diseases (Table 3). However, a total of 108 different diagnoses were issued. Out of those, the main individual processes were: atopic dermatitis (16%), acute prurigo simplex (5%), dermatophytosis (5%), pyogenic granuloma (4%), molluscum contagious (4%) and impetigo (4%).
Main diagnoses issued at the Emergency room in general paediatric population.
| Diagnosis | n (%) |
|---|---|
| Atopic dermatitis | 142 (17) |
| Prurigo | 45 (5) |
| Dermatophytosis | 39 (5) |
| Pyogenic granuloma | 35 (4) |
| Molluscum contagiosum | 34 (4) |
| Impetigo | 33 (4) |
| Gianotti–Crosti syndrome | 27 (3) |
| Seborrheic dermatitis | 23 (3) |
| Scabies | 22 (3) |
| Contact dermatitis | 20 (2) |
| Bites | 18 (2) |
| Urticaria | 18 (2) |
| Pityriasis rosea | 18 (2) |
| Child haemangioma | 17 (2) |
| Psoriasis | 15 (2) |
| Dyshidrotic eczema | 14 (2) |
| Herpes zoster | 13 (2) |
| Diaper dermatitis | 12 (1) |
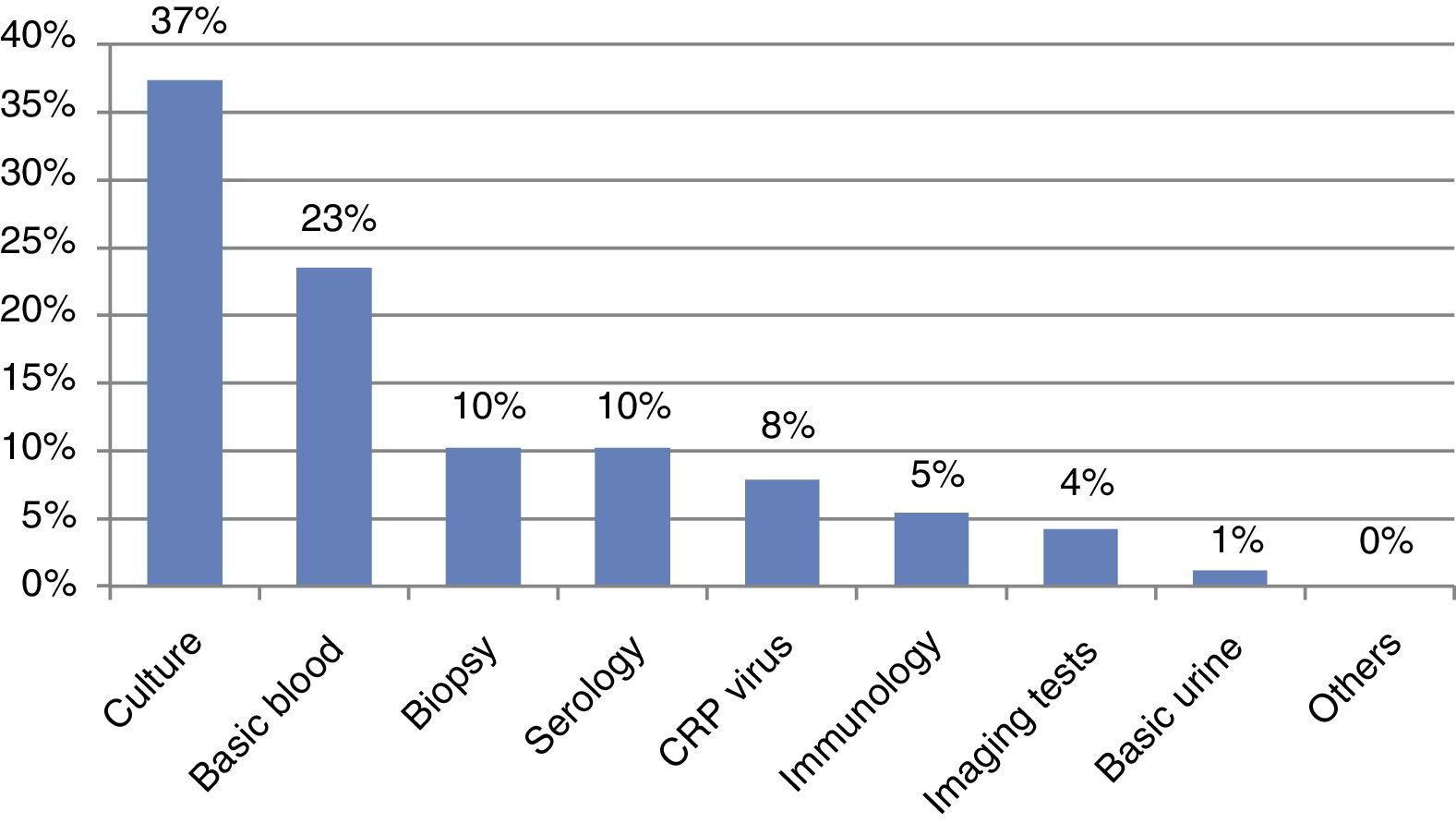
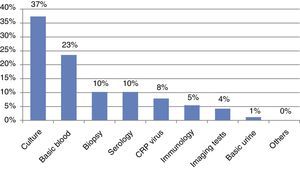
Regarding the consumption of supplementary tests, these were only required for 166 patients (16%); the one requested most frequently was microbiological culture (35%), followed by blood test with haemogram and biochemical (22%), serology (10%), skin biopsy (10%), CRP for herpesviridae (8%), immunology study (5%) and imaging tests (4%) (Fig. 4). In the group called “Others”, electrocardiograms and specific analytical determinations were included, such as cinquemia, serum triptase, etc.
Regarding destination after attendance, 48% of patients were directly discharged without the need for further consultations; 43% were referred to consultation to the ordinary Paediatric Dermatology Department; 6% of patients were referred by their GP and a later assessment by their dermatologist. In “other destinations” (2%), referrals to other consultants and their hospitals of reference were included. The resulting admission rate was 1% and included five children admitted with the following diagnoses: two due to infant haemorrhagic oedema, two due to eczema herpeticum and one due to disseminated herpes zoster in an immunocompromised patient.
When analysing all Casualty Department discharge reports of patients who were afterwards transferred to the Emergency Dermatology Department, it was observed that in 67% of the discharge there was a specific clinical judgement by the paediatrician, in 20% a descriptive diagnosis based on element lesions, and in 13% of the reports there was no dermatology diagnosis.
For the purposes of establishing diagnosis concordance among those cases where a specific clinical judgement was reached in the Casualty Department and afterwards assessment in the consultation by the Emergency Paediatric Dermatology Department, a contingency table was prepared whereby a kappa index of 0.206 was obtained (95% CI: 0.170–0.241).
DiscussionAlthough dermatology has been considered as a specialisation with no emergency service, it cannot be denied that the number of patients requesting immediate care in the Emergency Departments due to dermatological reasons represents a significant percentage of the total, with an estimated 8–10%.11,12 As expected, most of these consultations are not for truly serious diseases or diseases which may put the patient's life at risk.1–8 However, this increase in the demand for care in hospital Emergency Departments mainly due to minor complaints is not exclusive to dermatology, since it has been estimated that between one and two-thirds of the total consultations in Paediatric Emergency Departments are due to minor diseases.14,15
However, whether or not skin diseases are serious, there are other determinants leading the patient (or the relative, in this case) to attend the Casualty Department, such as the spectacular nature of the signs and symptoms (especially pruritus), the lack of information, doubts on whether the condition is transmissible, etc.
Due to the differences among health systems of each country, our discussion is based on prior studies carried out in Spain's public health system.1–8 Thus, the mean age obtained in our study (4.5 years) was lower than that found in the study carried out by Roca Saurina et al.5 and that stated by Colomés et al.,12 who refer the highest volume of attendance in ages 6 and 7. In fact, the patients with most consultations in our case were 0 to 1 year. Although the age groups created are heterogeneous as regard the period included (for instance, the group of infants includes from 0 to one year and the group of school-aged children 6–12 years), we think the information on the distribution of patients in the different stages is of interest, taking into consideration the large clinical and physiological variability in these relatively short periods of time (differences are evident between, for instance, an infant and a school-aged child).
As regards gender, studies on the general population have reported female predominance;6 however, in our study, as in the study by Roca Saurina et al.,5 no significant gender differences were shown.
When analysing the main diagnosis groups and comparing them with those obtained by other authors, we noted that infections were the main diagnosis groups in all studies, followed by eczema/dermatitis.1–8 In our case, the frequency of both groups was very similar, which we think is because in our study the mean age was lower and we attended to a larger number of infants, who often attend due to atopic dermatitis and other eczema.
The group of bites/prurigo was third in terms of frequency in children, as already described,5 while in the general population this position was occupied by the group of urticaria/angioedema.1–4,6
Regarding infections, the ones with the highest prevalence were those of viral origin (50% overall), matching the data obtained by Roca Saurina et al.5; but different from the data obtained in adults, where there is a predominance of bacterial origin.1–4,6 However, in our work fungal infections were second in terms of frequency (22%), followed by bacterial infections (18%), while in the work by Roca Saurina et al.5 bacterial infections were second in terms of frequency, followed by fungal infections. This difference may be due to the fact that in our case the dermatologist does not attend the Emergency room daily, and the patient has to be called to attend, and the paediatrician attends to the dermatological disease more frequently. In the case of eczema, both in our study and that carried out by Roca Saurina et al.,5 the most frequent cause is atopic dermatitis, while in adults it is contact dermatitis.6
As regards the distribution of diagnosis groups, it is noteworthy how the frequencies of the diseases are modified in the different intervals, in such a way that the group of infants was the one most different from the general population. As the age of the patient increased, the diagnoses were more and more similar to those of the general population.5 In fact, in the infants group, the percentage of eczema was much higher than in the other groups (36% overall in relation to 16% in children in puberty), mainly due to the higher frequency of atopic dermatitis in that population. It is noteworthy that 12% of the consultations in infants were due to vascular anomalies. In our study, unlike the earlier ones, we decided to differentiate this group, where vascular malformations and vascular tumours are included, mainly child haemangiomas and their complications, in the group of tumours because there are differences in management in relation to other tumours and because the centre has a specific Child Vascular Anomalies unit. The miscellaneous group was third in terms of frequency in this group, and included diseases typical of paediatric age, as already mentioned.
In early childhood (1–2 years) there is still a predominance, although less pronounced, of eczema (31% overall), and consultations due to infections almost doubled (23%). There was also a significant increase in this group of consultations due to bites and prurigo (11%), and a 2% drop in consultations due to vascular anomalies, as expected.
In pre-schoolers and school-aged children, infections and eczema continued to be the main causes of demand for care, but infections become more frequent than eczema. This inversion is due to the fact that, on the one hand, there was a decrease in some types of eczema, such as seborrheic dermatitis and atopic dermatitis, and, on the other, the increase in infections, mainly those of viral origin. In addition, the increase of consultations for other causes, such as erythematous dermatitis, with frequencies four times above those observed in the prior groups.
Lastly, in children in puberty infections continue to have predominance over eczema, but the frequency in both groups decreased and other groups become relevant, such as the tumours group (8% overall), with a large part of these consultations caused by pyogenic granulomas which may cause significant clinical symptoms, such as bleeding and rapid growth. It is worth noting the relevant difference obtained when comparing the frequencies of the urticaria and angioedema categories in the group of children in puberty according to the data published by Roca Saurina et al.5 and ours. In their case, urticaria/angioedema represented 30% of emergency consultations in this age group, while in our case it was 3%. We again attribute this marked difference to the system for calling patients to attend and the role of the paediatrician as a filter, who, except in atypical or torpid progression cases, usually has no trouble with the diagnosis and initial management of this disease.
As regards the resolution capacity of the dermatologist on duty, we noted how in our study the consumption of supplementary tests was low, data similar to those found by Grillo et al.6 Also, the most requested test was microbiological culture, a test that is easy to carry out, affordable and not at all aggressive. The percentage of skin biopsies was far below those carried out in adults.6 Almost half of the patients were directly discharged without the need for supplementary tests. Most cases transferred to child dermatology were carried out with a diagnosis and a treatment line already started.
The global concordance between the diagnoses issued by the family doctor and the dermatologist is, according to some studies, 40–60%.16,17 In our study the concordance percentage was 57% and the kappa index 0.206 (95% CI: 0.170–0.241), reflecting a scarce correlation. The interpretation of these data has a series of limitations, such as that only cases where both the paediatrician and the dermatologist have issued a diagnosis can be included, and that we only included cases attended to in the Emergency Paediatric Dermatology Department and who, therefore, have posed a question or enquiry to the paediatrician, and not all those who were actually assessed in the Casualty Department.
ConclusionsIt has been widely proven that pathological dermatology processes cause a large health care demand in Emergency Departments globally, and especially high during the paediatric age. Although most consultations were not due to serious diseases, these were perceived by parents as alarming, and there is a small percentage of diseases which do pose a real danger for the life of the child in the short term, such as eczema herpeticum or vasculitis, where the dermatologist on duty plays an important role both in the diagnosis and management. On the other hand, the dermatologist on duty offers a high resolution capacity regarding the low percentage of supplementary tests requested and the number of direct discharges. Lastly, carrying out epidemiology studies like the one presented would provide a better understanding of the clinical dermatological reality we attend to, and would allow us to prepare training plans for residents and paediatricians for the purpose of improving health care quality.
Conflict of interestsThe authors declare that there are no conflicts of interest.
Please cite this article as: Baquero-Sánchez E, Bernabéu-Wittel J, Dominguez-Cruz JJ, Conejo-Mir J. Urgencias dermatológicas pediátricas en un hospital de tercer nivel. An Pediatr (Barc). 2015;83:397–403.