The gluten-free diet has traditionally been accepted as a healthy diet, but there are articles advocating that it may have some nutritional deficiencies. The current study assesses whether there was any change in the contribution of calories, essential elements, proportion of fatty acids, vitamins, minerals and fibre in children who were diagnosed with celiac diseases, on comparing the diet with gluten prior to one year after diagnosis with the diet without gluten at the year of diagnosis. The level of clinical or analytical impact that nutritional deficits could have was also assessed.
Materials and methodsA prospective, descriptive, observational study was conducted in which information was collected from a dietary survey; anthropometric and analytical data were collected at pre-diagnosis of celiac disease and following a gluten diet and one year after celiac disease diagnosis, under gluten-free diet.
ResultsA total of 37 patients meet the study criteria. A decrease in the intake of saturated fatty acids was found, with an increase of monounsaturated fatty acids and an increase in the intake of phosphorus in the diet without gluten. A deficient intake of vitamin D was found in both diets. Clinically, at year of gluten-free diet there was an improvement in weight and size. Analytically, there was an improvement in haemoglobin, ferritin, vitamin D, and parathyroid hormone in plasma.
ConclusionThe gluten-free diet has minimal deficiencies, similar to those present in the diet with gluten, with an improvement in the lipid profile by increasing the proportion of monounsaturated fatty acids to the detriment of saturated fatty acids.
Clásicamente, se ha presentado la dieta sin gluten como una dieta sana, pero existen artículos que defienden que puede presentar algunas deficiencias nutricionales. En el presente estudio se valoró si existía algún cambio en los aportes de calorías, principios inmediatos, proporción de ácidos grasos, vitaminas, minerales y fibra en los niños que eran diagnosticados de celiaquía, comparando la dieta con gluten previa al diagnóstico con la dieta al año del diagnóstico sin gluten. También se valoró el grado de repercusión clínico o analítico que podrían tener los déficits nutricionales.
Material y métodosEstudio observacional, descriptivo y prospectivo en el cual se recogieron los datos de encuesta dietéticas, antropometría y analítica previas al diagnóstico de celiaquía siguiendo dieta con gluten y al año del diagnóstico, con dieta sin gluten de los pacientes diagnosticados de enfermedad celíaca.
ResultadosTreinta y siete pacientes reúnen criterios de estudio. Se encontró una disminución en la ingesta de ácidos grasos saturados, con un aumento de monoinsaturados, un aumento en la ingesta de fósforo en la dieta sin gluten y un ingesta deficitaria de vitamina D en ambas dietas. Clínicamente, al año de dieta sin gluten hay mejoría en el peso y la talla. Analíticamente, hay mejoría en las cifras de hemoglobina, ferritina, vitamina D y parathormona plasmáticos.
ConclusiónLa dieta sin gluten presenta mínimas deficiencias, similares a las presentes en la dieta con gluten, con una mejoría en el perfil lipídico, aumentando la proporción de ácidos grasos monoinsaturados en detrimento de los ácidos grasos saturados.
Coeliac disease is a systemic immune disease caused by gluten and related prolamines in genetically susceptible individuals, and characterised by the presence of a variable combination of clinical manifestations that depend on gluten intake, specific antibodies, the HLA-DQ2 or HLA-DQ8 haplotypes, and enteropathy.1 The treatment of coeliac disease requires a life-long diet with exclusion of all foods containing gluten or related prolamines. The gluten-free diet has traditionally been declared healthy, but there are studies that suggest that it may be associated to some nutritional deficiencies due to the exclusion of gluten-containing cereals, which are rich in iron, fibre and B-group vitamins.2,3 Thus, the literature includes reports of decreased intakes of group-B vitamins, calcium, vitamin D, magnesium, iron, folic acid and fibre, which could have an impact on blood levels, with decreased concentrations of vitamin B6, vitamin B12 and vitamin D, and in the development of anaemia and osteopaenia. This deficient intake is partly due to the lower fibre, iron, folate, thiamine, riboflavin and niacin content of gluten-free foods.3–5 When it comes to macronutrients, the literature has descriptions of higher intakes of lipids and lower intakes of carbohydrates, which may be attributable to processed gluten-free foods usually being rich in fats and sugars with a high glycaemic index.3,5 This fact may have clinical repercussions in the form of an increased incidence of overweight or obesity in coeliac children on such a diet,4,6 as well as the presence of a serum fatty acid (FA) profile with a predominance of saturated and monounsaturated FAs and low concentrations of polyunsaturated FAs.7
The aim of our study was to analyse whether there were any changes in the intake of energy, essential nutrients, proportion of FAs, vitamins, dietary elements (iron, calcium, zinc, phosphorus) and fibre in the diet of children diagnosed with coeliac disease. Our secondary goal was to assess whether the gluten-free diet can be deficient in any nutrients for coeliac children, and the extent to which such deficits may impact the patients.
Materials and methodsWe conducted an observational, descriptive and prospective study in which we collected data for the patients diagnosed with coeliac disease in the paediatric digestive diseases unit over 2 years, from April 1, 2011 to March 31, 2013. For each patient, we collected data corresponding to one year. A food questionnaire was completed on 3 alternating days (one of them on a holiday or weekend) before the start of the gluten-free diet, and again one year after diagnosis, when the patient was on a strict gluten-free diet. We directed the parents or guardians of the children to document with the utmost possible accuracy the amounts of food ingested, how the foods were prepared, and the brands of the products consumed. We evaluated the following: energy intake and percentage of calories consumed relative to the patient's energy requirements calculated by means of the Schofield equation for weight, height and level of activity (the level of activity was estimated based on the information gathered from the parents in the clinical interview at the time of diagnosis); the percentage of carbohydrates, proteins, lipids and FA composition of the total consumed; the percentage of vitamins and dietary elements consumed in relation to the dietary reference intakes (DRIs) of the National Academy of Sciences of the United States8–13; and the daily amount of fibre consumed. We calculated these values using the software application Dietsource junior®. In addition to the dietary assessment, we collected anthropometric data (weight, height, body mass index [BMI], Waterlow weight-for-height classification) at the beginning of the study and a year later. The data for these variables were collected by a nurse before the visit, using the same scale (accurate to 0.1kg) and stadiometer (accurate to 0.1cm). The weight, height and BMI values were expressed as standard deviations using the tables of Fernández et al. as a reference.14 We defined overweight and obesity as a BMI at or above the 85th percentile (z≥1.28) and at or above the 95th percentile (z≥1.65), respectively, based on the recommendations of the Comité de Nutrición (Committee on Nutrition) of the Asociación Española de Pediatría (Spanish Academy of Pediatrics).15 We also collected data from blood tests performed at diagnosis and a year after, concurrent with the administration of the food questionnaire. We assessed the following parameters: haemoglobin, haematocrit, serum iron, transferring saturation index (TSI), IgA, IgA anti-tissue transglutaminase and antigliadin (IgG anti-tissue transglutaminase and antigliadin in patients with IgA deficiency), IgA or IgG antiendomisyum if required, HLA (only at diagnosis), folic acid, vitamin B6, vitamin B12, homocysteine, calcium, phosphorus, parathyroid hormone and vitamin D. We also tested for parasites in 3 samples taken on alternating days to rule out parasitic disease at diagnosis.
The study was approved by the committee on ethics and clinical research of our hospital. We established the following inclusion criteria:
- –
Age: 0–13 years.
- –
Diagnosed with coeliac disease, based on the criteria of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition,1 during the period under study.
- –
Followed up at the paediatric digestive diseases unit.
The exclusion criteria were the following:
- –
Children 14 years of age or older.
- –
Diagnosed with coeliac disease at a time outside the period under study.
- –
Children with coeliac disease already undergoing treatment for this condition.
- –
Presence of a chronic underlying condition other than coeliac disease.
- –
Undergoing chronic treatment (more than 1 month of duration) with some type of drug, hormone, or calcium, iron or vitamin D supplement.
- –
Persistence of positive coeliac disease markers a year after initiation of the gluten-free diet.
- –
Lack of a signed informed consent.
- –
Following some type of exclusion diet in addition to the gluten-free diet for more than one month.
We performed the statistical analyses with the software IBM SPSS 19.01, assessing changes in mean values with the Wilcoxon test, with the level of statistical significance set at P<.05.
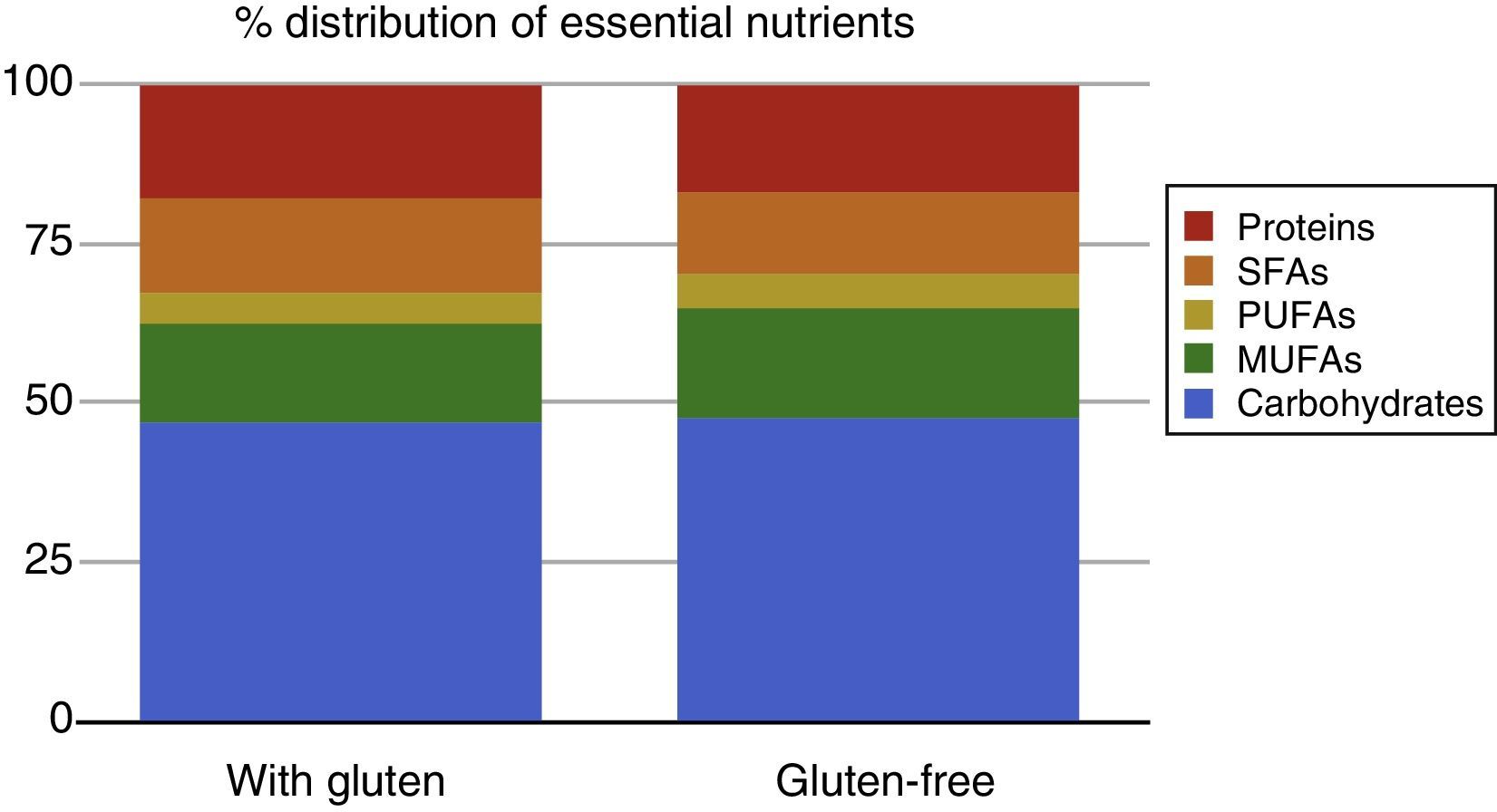
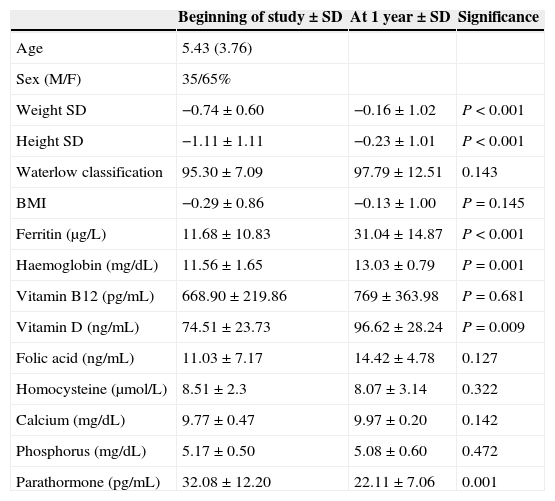
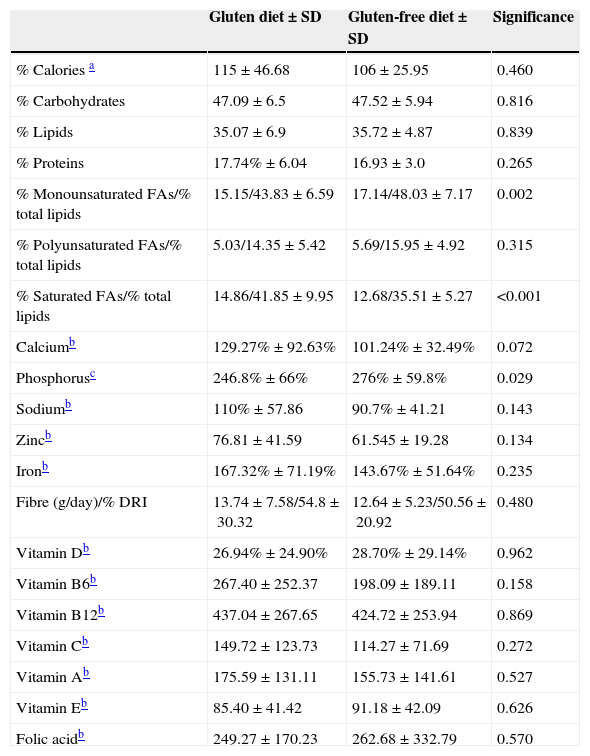
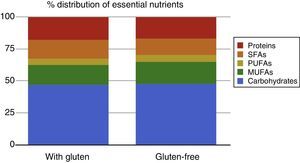
ResultsWe recruited a total of 69 patients with coeliac disease; 49 of them submitted the food questionnaire at the time of diagnosis, of which 37 submitted another food questionnaire a year after. The remaining 12 patients are currently in follow-up, as it has not yet been a year since they started the gluten-free diet. The final sample comprised a total of 37 patients, of whom 35% were male and 65% female. Their ages ranged between 1 and 13 years, with a mean of 5.43 years and a median of 4.5 years (Table 1). We did not find significant differences in the percentages of energy intake relative to the estimated energy requirements for age, sex, and daily physical activity (115% vs 106%). We also found no differences in the intake of the different essential nutrients: carbohydrates (47.6% vs 47.42%), lipids (35.57% vs 35.6%) and proteins (18.24% vs 16.93%) (Table 2 and Fig. 1).
Patient characteristics.
| Beginning of study±SD | At 1 year±SD | Significance | |
|---|---|---|---|
| Age | 5.43 (3.76) | ||
| Sex (M/F) | 35/65% | ||
| Weight SD | −0.74±0.60 | −0.16±1.02 | P<0.001 |
| Height SD | −1.11±1.11 | −0.23±1.01 | P<0.001 |
| Waterlow classification | 95.30±7.09 | 97.79±12.51 | 0.143 |
| BMI | −0.29±0.86 | −0.13±1.00 | P=0.145 |
| Ferritin (μg/L) | 11.68±10.83 | 31.04±14.87 | P<0.001 |
| Haemoglobin (mg/dL) | 11.56±1.65 | 13.03±0.79 | P=0.001 |
| Vitamin B12 (pg/mL) | 668.90±219.86 | 769±363.98 | P=0.681 |
| Vitamin D (ng/mL) | 74.51±23.73 | 96.62±28.24 | P=0.009 |
| Folic acid (ng/mL) | 11.03±7.17 | 14.42±4.78 | 0.127 |
| Homocysteine (μmol/L) | 8.51±2.3 | 8.07±3.14 | 0.322 |
| Calcium (mg/dL) | 9.77±0.47 | 9.97±0.20 | 0.142 |
| Phosphorus (mg/dL) | 5.17±0.50 | 5.08±0.60 | 0.472 |
| Parathormone (pg/mL) | 32.08±12.20 | 22.11±7.06 | 0.001 |
BMI, body mass index; SD, standard deviation.
Mean intake values for different diets.
| Gluten diet±SD | Gluten-free diet±SD | Significance | |
|---|---|---|---|
| % Calories a | 115±46.68 | 106±25.95 | 0.460 |
| % Carbohydrates | 47.09±6.5 | 47.52±5.94 | 0.816 |
| % Lipids | 35.07±6.9 | 35.72±4.87 | 0.839 |
| % Proteins | 17.74%±6.04 | 16.93±3.0 | 0.265 |
| % Monounsaturated FAs/% total lipids | 15.15/43.83±6.59 | 17.14/48.03±7.17 | 0.002 |
| % Polyunsaturated FAs/% total lipids | 5.03/14.35±5.42 | 5.69/15.95±4.92 | 0.315 |
| % Saturated FAs/% total lipids | 14.86/41.85±9.95 | 12.68/35.51±5.27 | <0.001 |
| Calciumb | 129.27%±92.63% | 101.24%±32.49% | 0.072 |
| Phosphorusc | 246.8%±66% | 276%±59.8% | 0.029 |
| Sodiumb | 110%±57.86 | 90.7%±41.21 | 0.143 |
| Zincb | 76.81±41.59 | 61.545±19.28 | 0.134 |
| Ironb | 167.32%±71.19% | 143.67%±51.64% | 0.235 |
| Fibre (g/day)/% DRI | 13.74±7.58/54.8±30.32 | 12.64±5.23/50.56±20.92 | 0.480 |
| Vitamin Db | 26.94%±24.90% | 28.70%±29.14% | 0.962 |
| Vitamin B6b | 267.40±252.37 | 198.09±189.11 | 0.158 |
| Vitamin B12b | 437.04±267.65 | 424.72±253.94 | 0.869 |
| Vitamin Cb | 149.72±123.73 | 114.27±71.69 | 0.272 |
| Vitamin Ab | 175.59±131.11 | 155.73±141.61 | 0.527 |
| Vitamin Eb | 85.40±41.42 | 91.18±42.09 | 0.626 |
| Folic acidb | 249.27±170.23 | 262.68±332.79 | 0.570 |
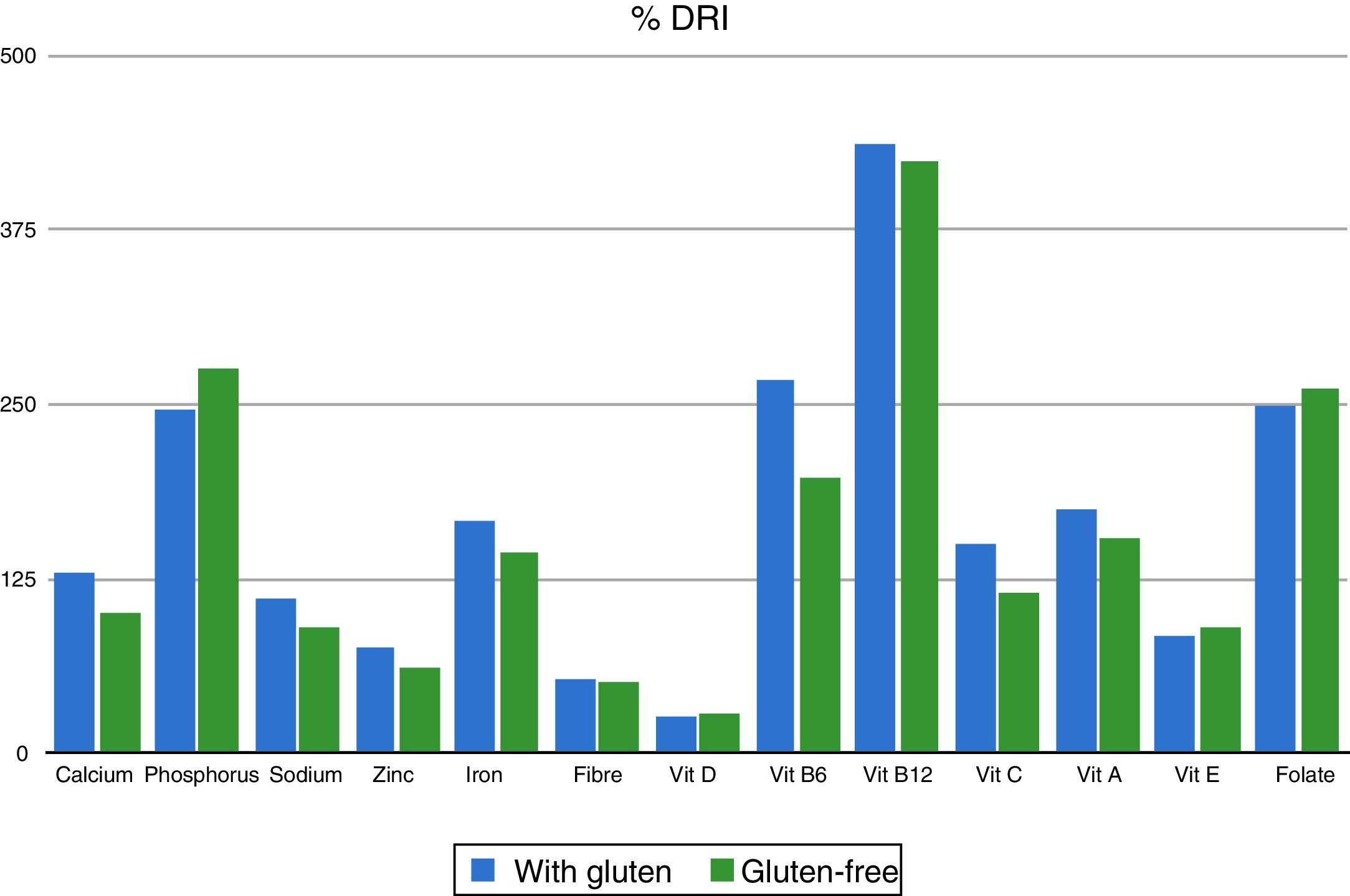
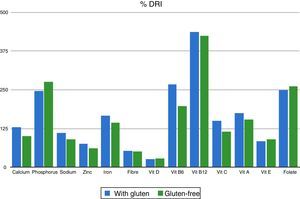
The analysis of the intake of different types of FAs did reveal significant differences, with an increase in the intake of monounsaturated FAs in the gluten-free diet (43.83% vs 48.03%; P=0.002) and a decrease in saturated FAs (41.85% vs 35.51%; P<0.001). When it came to vitamins, we found a deficient vitamin D intake both in the gluten-containing and the gluten-free diets, and no significant differences in its intake depending on the type of diet (26.94% vs 28.7%; P=0.962). As for dietary elements, we found a deficient zinc intake in both diets. We only found significant differences in the intake of phosphorus (246% vs 276% of the adequate intake; P=0.029), with normal intakes and no differences between both diets for sodium, calcium, iron, vitamins B6, B12, A and E, folic acid and fibre (Table 2 and Fig. 2).
In terms of anthropometric values, we observed a statistically significant increase in weight and height, while patients remained within normal ranges for BMI and Waterlow classification (Table 1).
At the beginning of the study, laboratory tests revealed low haemoglobin and ferritin values, which subsequently showed significant improvement. Vitamin B12, folic acid, homocysteine, calcium and phosphorus levels were within normal ranges, and showed no changes in the control performed at year 1. Vitamin D and parathyroid hormone levels were within the normal range at the beginning and at one year, although they did change in a statistically significant way, with the levels of vitamin D increasing and those of parathyroid hormone decreasing (Table 1).
DiscussionOur study aimed to assess the quality of the gluten-free diet in the paediatric age group and its impact on anthropometric and laboratory variables. We found that the elimination of gluten from the diet did not lead to changes in energy and essential nutrient intakes. Published case series that make overall assessments of the gluten-free diet found that the diet was normal (80–120% of the recommended energy intake) or hypercaloric (>121% of the recommended intake), with a high energy contribution of proteins and lipids.5,16–20 In our study, we observed a normal energy intake that was not above the past intake prior to elimination of gluten from the diet, with a high percentage of proteins and lipids and a slightly low carbohydrate intake. Traditionally, it was argued that the introduction of a gluten-free diet entailed an increase in lipid consumption as a result of a reduction in the intake of carbohydrates from the elimination of gluten-containing cereals from the diet.16,17 This did not happen in our study. One possible explanation is that more gluten-free products are now available for coeliac patients, including bread and cereals, which taste better and are more affordable, so that patients do not change their habits and continue consuming cereals as they used to. Another factor that may be at play is the commitment of the parents of these patients to complying correctly with the diet, which motivates many of them to prepare meals at home using foods with adequate macronutrient, micronutrient, vitamin and fibre contents, thus precluding the consumption of processed foods rich in lipids. The same reasons may account for the fact that the fibre intake, while below the recommended intake for age, did not change significantly. A low fibre intake is consistently found in the studies on the gluten-free diet2,4,16,17,19–21 and attributed to decreased consumption of gluten-containing cereals, which may contribute up to 35% of the daily fibre intake in children.19 A possible solution to this problem could be to promote the consumption of pseudocereals that are allowed but not as common, such as quinoa, amaranth or buckwheat, which have greater fibre and polyunsaturated FA contents than cereals like rice.3
The intake of dietary elements and vitamins in both types of diet was normal except for vitamin D and zinc, in contrast with other studies that show deficiencies in the intake of vitamin B6, iron or calcium.3,17,20,21 In regards to the insufficient intake of vitamin D both in the gluten-containing and the gluten-free diet, it is worth noting that while we did not find 1,25-(OH) vitamin D serum levels below the normal range at any point, we observed a significant increase in its serum levels accompanied by a decline in the parathyroid hormone levels. A possible explanation for the absence of low serum vitamin D is that the population under study is from a geographical area (Seville) with high amounts of sunlight, which is an important source of this vitamin. On the other hand, the improvement in vitamin D levels and the decrease in the levels of parathyroid hormone reflect a better homeostasis of vitamin D in coeliac patients, which may be due to mucosal recovery and increased absorption of vitamin D at the intestine. This finding deserves further analysis due to its potential repercussion on the bone mineral density of patients with coeliac disease, who have higher rates of osteopaenia than the general population22 and often receive vitamin D supplements since its levels are deemed deficient. Zinc intake is inadequate in both types of diet. There are studies that demonstrate the association between zinc deficiency, the gluten-free diet3,5,19 and a greater severity of villous atrophy, although the actual repercussions of an insufficient zinc intake are still not known.4,23,24
We did find a change in the intake of the different types of FAs, with a decrease in the intake of saturated FAs and an increase in the intake of monounsaturated FAs. Hopman et al., Öhlund et al. and other authors have observed high levels of FA consumption (12% and 14.5%, respectively) based on the current intake recommendations of less than 10%, as was the case in our study (14.86%). The high intake of saturated FAs was accompanied by an insufficient intake of polyunsaturated FAs (5.03%), which has also been reported in other case series.2,17,19 We believe that this finding reflects that both the gluten-free and the gluten-containing diets in our patients are significantly impacted by the consumption of animal fats while being low in vegetable oils or fish rich in polyunsaturated FAs.
The improvement on anthropometric parameters is similar to that found in other studies of paediatric patients.24,25 Mariani et al. reported a 72% rate of overweight in adolescents on a gluten-free diet18 that has not been found in other studies, which estimate overweight in coeliac patients at 12–38%.17,19,21,23,26,27 In our study, we did not find high rates of overweight (2.9% at diagnosis vs 2.8% after one year without gluten) or of obesity, either at diagnosis or at the 1-year control (4.34% at diagnosis and 5.55% with the gluten-free diet), figures that diverge considerably from those published by the Spanish Ministry of Health for the population of Spanish children, of 18.26% for overweight and 15.15% for obesity,28 compared to which we found a significant difference at the beginning of the study (P=0.0093; 95% confidence level) and at one year (P=0.02; 95% confidence level). The fact that there is no increase in the distribution and contribution to the total energy intake of the different macronutrients leads us to believe that the weight and height recovery is mostly due to recovery from the enteropathy suffered by these patients rather than to increases in energy intake.
When it came to laboratory findings, we observed no deficiencies in vitamin A, vitamin B6, vitamin E, vitamin C and vitamin B12 or folic acid. The data on vitamin B12 and folic acid in the literature is contradictory, ranging from series documenting vitamin B12 and folic acid deficiencies in 11–41% and 4.7–31% of cases, respectively, to series with normal values for these micronutrients.2,5,17,19,24 The mechanism leading to these deficiencies in the published series remains unclear, as the sites of absorption for vitamin B12 and folic acid are the ileum and the jejunum, respectively, both areas – especially the former – that are usually less affected by coeliac disease, so we should probably explore possible concomitant factors other than mucosal involvement or nutritional deficits in the development of these deficiencies in coeliac patients. The most common laboratory abnormality was the presence of iron-deficiency anaemia, found in 27.27% of the patients, which is characteristic of newly diagnosed coeliac disease24 even with an adequate intake of iron. This anaemia resolved within the year, which illustrates the considerable problems in iron absorption experienced by coeliac patients.
One of the limitations of the study was the use of the 3-day questionnaire completed by patients or more commonly by their parents. This type of questionnaires may underestimate energy intake due to errors in data collection and changes in dietary habits during the assessment period, during which there is a tendency to have a “healthier” nutrition. Another potential source of error is the lack of complete information for some food products for coeliac individuals, which poses challenges to the assessment of total nutrient intakes.
ConclusionsThe data obtained in our study show, on one hand, that the intake of energy and different essential nutrients remains similar despite the switch to a gluten-free diet. The deficiencies and flaws observed in the gluten-free diet were similar to those found in gluten-containing diets (insufficient intakes of vitamin D intake and zinc, diet rich in fats and poor in fibre), and there was an improvement in lipid profiles, with a decrease in saturated FAs and an increase in monounsaturated FAs.
The few changes detected in terms of nutrition suggest that the key to catch-up growth and recovery from complications such as iron-deficiency anaemia in coeliac patients is adequate compliance with the exclusion of gluten from the diet, rather than potential changes in the nutrients consumed. We believe that the gluten-free diet is a healthy diet that, overall, has the same flaws and benefits as the usual diet of children in Spain. Monitoring the diet allows for the correction of any potential lacks, so that any deficiencies found in the child at diagnosis can be remedied, and an optimal health and nutrition status can be maintained throughout life.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Salazar Quero JC, Espín Jaime B, Rodríguez Martínez A, Argüelles Martín F, García Jiménez R, Rubio Murillo M, et al. Valoración nutricional de la dieta sin gluten. ¿Es la dieta sin gluten deficitaria en algún nutriente? An Pediatr (Barc). 2015;83:33–39.