Introduction
Infectious endocarditis is still a rare infection in pediatrics 1-3. Recently, changes have been reported in incidence, agents and risk factors for endocarditis 4. In the past, rheumatic fever was a very frequent cause of endocarditis and has been disappearing in western countries. Congenital heart disease (with or without surgery) has remained the major risk factor for endocarditis in children. Other risk factors for endocarditis include serious systemic underlying illness and congenital and acquired immunodeficiency. There has been a steadily increase in the number of children with these problems who would also be at risk for endocarditis. In spite of progress in diagnostic techniques and treatment, infective endocarditis continues to be difficult to diagnose in children.
The first objective of this study was to evaluate the etiology, epidemiology, pathogens and evolution of a cohort of pediatric patients with endocarditis. The second objective was to compare their main characteristics to our previously published experience.
Material and methods
A retrospective cohort study was conducted. All children less than 18 years of age diagnosed with endocarditis at the CHU Sainte-Justine in Montreal, Canada, between January 1986 and December 2000 were included in the study. Seventy eligible patients with endocarditis were identified through medical records according to the codes of the 9th Revision of the International Classification of the Diagnosis. There were fourteen cases who did not fulfill the Durack's 5 criteria and were excluded. Patients who fulfilled Duke's 5 criteria for endocarditis at the time of discharge were included in the study.
Patient information was recorded retrospectively by a single investigator (GL) using a standardized case report form. Data collected included: demographic characteristics, symptoms, signs, previous medical condition, history of congenital heart disease, presence of a central venous catheter and diagnosis at the time of admission to the hospital. Other data included were: white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), blood culture(s) and echocardiography results. Antibiotic therapy, length of hospital stay, surgery and evolution of the disease were also noted.
When available, pathological and autopsy results were reviewed. In patients who underwent cardiac surgery or autopsy, diagnostic confirmation was done by direct observation of the cardiac injuries and vegetations. Material obtained was evaluated by anatomopathological, bacteriological study and culture.
Characteristics of the recent series of 1986-2000 were compared to our previous experience of 1960-1985 6.
Definitions
Anemia: haemoglobin less than 120 g/L. Leukocytosis: WBC > 15.0 x 10 9/L. Thrombocytopenia: platelets < 140 x x 10 9/L. Erythrocyte sedimentation rate (ESR): considered abnormal if > 20 mm/h. Transthoracic two-dimensional echocardiography has been used in our hospital since 1980. Transoesophageal and Doppler echocardiography were introduced later and used in some patients. Vegetation: mass adherent to a valve or to one cardiac structure that presented with different echogenic characteristics. Nosocomial infection: onset of endocarditis which appeared ≥ 72 hours after admission for another medical reason.
Results
Clinical and demographic characteristics
Fifty-six children with endocarditis were included in the study. Mean age was 7 years and ten months (range: 19 days to 18 years). Fifty-four percent of the patients were male. Risk factors for endocarditis are shown in figure 1. Clinical symptoms and signs are summarized in table 1. Nine children (16 %) did not have fever at the time of presentation of the infection: premature infants in neonatal intensive care (2 patients), immunodeficiency (3 patients), chronic disease (1 patient), congenital heart disease associated with other malformations (2 patients) and one healthy child. In our recent series, the incidence of fever, cutaneous and neurological signs were seen more frequently than in our past experience (84 % vs. 54 %, 32 % vs. 19 %, and 38 vs. 27 %, respectively). Fatigue and splenomegaly were less frequent (48 % vs. 95 % and 25 % vs. 46 %, respectively); the incidence of embolic phenomenon was similar (20 % vs. 19 %, respectively). The prevalence of endocarditis was 1.5 cases / year for the period 1960-1985 6 and 4 cases / year for the period 1986-2000.
Figure 1.Risk factors and underlying diseases in 56 patients with infectious endocarditis. RV: right ventricle; LV: left ventricle. Patients with immunodeficiency: nephrotic syndrome, third degree burns, lupus, leukemia, HIV, lymphoma, neoplasia, juvenile rheumatoid arthritis. Patients with chronic disease: massive telangiectasia, encephalopathy. av: atrioventricular.
Diagnosis
Of the 56 patients with endocarditis, 51 acquired the infection in the community and 5 were nosocomial. At the time of admission to hospital, endocarditis was suspected in 20 of the 51 patients (40 %) who had acquired the infection in the community. Other diagnosis at admission were bacteremia or fever of unknown origin (12 cases = 23.5 %), pneumonia-sinusitis (5 cases = 9.8 %), septic shock (4 cases = 7.8 %), meningitis (3 cases = 5.8 %), and others (5 cases = 9.8 %). A patient underwent surgery for suspected appendicitis; another one was treated for several months with an erroneous diagnosis of rheumatoid arthritis. Forty-four patients were diagnosed using clinical signs and cardiac echocardiography. Ten cases diagnosed on clinical grounds were also confirmed with pathologic examination after surgery. Two cases who were not initially suspected, were subsequently diagnosed based on pathologic examination. Median duration of time to confirm the diagnosis of endocarditis was one day.
Thirty-five patients had congenital heart disease (62.5 %) (fig. 1). Of those, 21 patients (60 %) had undergone cardiac surgery. Three children with congenital heart disease developed endocarditis in the early postoperative period within two months of the surgery. One patient had undergone cardiac catheterization two months before the diagnosis of endocarditis was made. Ten patients had a central venous catheter. A total of 16 patients had vascular prostheses (coils, Hancock, Gore-Tex, Dacron, animal or homologous graft). Four patients had pre-existing cardiac disease that was not diagnosed until they presented with endocarditis: three had aortic valve anomalies and one an aortic coarctation. These four patients have been included in the group of children with heart disease (fig. 1). The diagnosis of endocarditis was made following varicella in two patients and dental manipulation in five.
Hematology
Increased WBC was present in only 28.5 % of the patients. Anemia was documented in 67 % and thrombocytopenia in 38 % of patients. ESR was increased in 80 % of patients.
Microbiology
Blood cultures were positive in 50 patients (89 %). Cultures were sterile in six children. Five of those six patients were receiving antibiotics at the time the blood culture was obtained. An average of 3 blood cultures were collected from each patient (median of 2 and range: 0 to 13). The pathogens isolated in the patients are shown in table 2. Staphylococcus aureus was found in 12 patients (24 % of all positive blood cultures), and only one of those died. Four of the six healthy children had an infection with S. aureus (66.7 %). One patient hospitalized in the neonatal intensive care unit with a history of necrotizing enterocolitis and ileostomy had a positive blood culture for Candida albicans. Aspergillus was found on pathological study of a valve in a single patient. This patient had congenital heart disease and had been treated for osteomyelitis complicated with an endocarditis who did not respond to medical treatment. Enterococcus spp. alone was not responsible for any case of endocarditis in our series, but was associated with another pathogen (S. epidermidis) in a patient with endocarditis in the intensive care unit.
Echocardiography
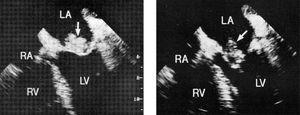
One patient with trisomy 18 and congenital heart disease, died before echocardiography was performed. Echocardiography was positive in 36 of the 55 patients who underwent this examination (65.4 %). During the time transesophageal echocardiography has been used, there were 28 cases of endocarditis and this technique was used in 46.4 % of the patients. At the time of the diagnosis of endocarditis, echocardiographic anomalies were located on the right side of the heart in 11 patients and on the left side in 18. In several cases, the vegetations were not present at the initial examination, but were seen on follow-up examinations. Thirty-one patients had obvious vegetation present on ultrasound. Three patients had vegetations in two valves. The mitral valve (fig. 2) was more frequently involved (13 patients). Anomalies in other structures were: tricuspid valve (6 patients), aortic valve (5 patients) (fig. 3), right atrium (4 patients), coronary sinus (1 patient) and pulmonary valve (1 patient). In four patients, anomalies were located in the ventricular septal defect. The six healthy children presented with anomalies located only in the left side of the heart.
Figure 2. Vegetation on mitral valve. RA: right atrium; LA: left atrium; RV: right ventricle; LV: left ventricle.
Figure 3. Vegetation on aortic valve. AV: right atrium; LA: left atrium; RV: right ventricle; LV: left ventricle.
Treatment and evolution
All patients were treated with intravenous antibiotics for an average of 43 days ± 15 (median of 42 days and range: 1 to 84 days). Thirteen patients completed antibiotic therapy at home after their medical condition had been stabilized. There were no recurrences.
Evolution was favorable in 30 patients who responded to medical treatment. Significant complications occurred in 26 patients (46 %) (table 3). Children who had risk factors either central venous catheters or valvular prostheses (20/26) preceding the diagnosis of endocarditis, developed more complications (p < 0.03) than those who did not. Complications secondary to endocarditis decreased significantly: from 85.7 % in 1960-1985 6 to 46.4 % in 1986-2000 (p < 0.001). Embolic phenomena were seen in 11 children (20 %). One child developed a central nervous system complication (cerebro-vascular accident) secondary to a mycotic aneurism. Three patients developed respectively, cardiac tamponnade, acute tubular necrosis, and nodules in the lungs and liver. Twelve patients (21 %) needed surgery during the initial hospitalization, including valvular surgery in six children, removal of vegetation in four, and replacement of vascular patch or fistula in two. Of the six healthy children without pre-existing heart disease, five developed complications: three had a mycotic aneurism and two cerebral emboli. Three of these patients needed surgery.
Mortality secondary to endocarditis decreased significantly: from 27.0 % in 1960-1985 6 to 12.5 % in 1986-2000. Seven children died; all were older than six years of age (table 3). Four patients died of early complications of their endocarditis. Two children died in the pediatric intensive care unit with multiple organ failure. One patient died with trisomy 18 and congenital heart disease. Three of the patients who died had congenital heart disease (3/35, 8.5 % mortality rate), three had another systemic underlying disease other than cardiac pathology and only one patient was healthy with normal cardiac anatomy.
According to Duke's 5 criteria, the cases of infectious endocarditis were considered either definitive (24 patients) or possible (32 patients). According to the modified criteria by Li 7, the patients would have been classified as definitive endocarditis (24 patients), possible (29 patients) and three cases would have been rejected. These three patients had complex congenital heart disease. Two of them had had previous cardiac surgery and one had undergone cardiac catheterization. These three patients presented with only two minor criteria: heart disease and prolonged fever; they were treated as possible endocarditis.
Discussion
Despite being a rare infection, our recent experience shows an increased prevalence of endocarditis; this is in agreement with other authors 6,8. In addition to an increased survival following cardiac surgery, there are other risk factors considered as predisposing conditions for infective endocarditis 4. Improvement of resuscitation methods and newer technologies introduced in intensive care units for newborns and very ill children, have created a new group of patients with an increased risk of endocarditis 3,4. Twenty-five percent of the patients had a serious systemic underlying disease or underlying malignancy. Patients with immunodeficiency can present without fever. Central venous catheters increase the risk of endocarditis and are a frequent cause of nosocomial infections 9-12. Healthy children, without pre-existing heart disease or other risk factor, constitute 8-10 % of the cases of endocarditis in the literature 3; in our series, it was 10.7 %. Frequently, in these cases, the endocarditis is secondary to bacteremia with S. aureus and has a worse prognosis 3. Dental alterations or manipulations were important risk factors in our first series (17 cases = 46 %), as compared to the present study (5 cases = 9 %), probably secondary to better dental follow-up.
In our recent study, congenital heart disease continues to be the most common risk factor for endocarditis (before or after surgery) when tissues weaves or prosthesis have been implanted. As in the literature 13, tetralogy of Fallot and transposition of the great vessels continue to be the most frequent cyanotic heart disease involved in endocarditis. In the non cyanotic heart diseases, ventricular septal defect and left ventricular outflow tract obstruction are the most important underlying conditions 13.
The clinical presentation continues to be non specific and the diagnosis is difficult. The extra-cardiac manifestations that are frequent in adults are rare in children, with the exception of embolic, neurologic and cutaneous phenomena. The pediatrician must have a great index of suspicion for endocarditis in children with fever and underlying cardiac abnormalities. The presence of a pathologic heart murmur in a child who presents to the emergency room with fever should rise the possibility of endocarditis; however, absence of an heart murmur does not rule out this diagnosis 14.
The WBC is non specific for the diagnosis of endocarditis. In our experience, 71 % and 33 % of our patients had a normal WBC and hemoglobin, respectively. The erythrocyte sedimentation rate was elevated in a significant proportion of patients with endocarditis; nevertheless, it can be normal at the time of the initial visit or admission to the hospital. In our center, we obtained an average of three blood cultures, in concordance with the recommendations of the literature 3,15. In 89 % of patients, the blood cultures were positive; a similar rate has been reported in the litterature 3. Some authors report that S. aureus causes 12 % of endocarditis cases, with a mortality of 40 % 12. Recently, Fowler 16 and colleagues published a study of 1800 adult patients from 16 different countries, reporting that S. aureus was the pathogen in 31.4 % of their cases of endocarditis. In our series, twelve children were infected with S. aureus (24 %) and only one of these patients died. In our study, Streptococcus viridans continues to be the most frequent pathogen (30 %). Another recent study 17 reports that S. viridans is the most frequent pathogen of endocarditis in adults.
Echocardiography was positive in 64 % of our patients, similar to what has been reported in the literature 18. Sensitivity of transthoracic echocardiography in pediatric patients is 86 % for general cardiac examination and 93 % to identify vegetation 18. The heart ultrasound must be repeated to demonstrate vegetation; sometimes on the first examination an echogenic mass is seen, and in a later examination, the vegetation is evident 18. A transoesophageal echocardiography must be considered in pediatric patients with sub optimal transthoracic window or when vegetations are not detected by conventional ultrasound 18,19.
In our series, the diagnosis and treatment were established for most patients within the first 24 hours after admission, as mentioned in the literature 14. There were some patients who had a delayed diagnosis, up to two months demonstrating that endocarditis diagnosis can still be difficult 13. Risk factors for complications mentioned in the literature include type of infectious pathogen, location and size of the vegetation, previous cardiac conditions, heart with a pre-existing normal anatomy, and children less than 2 years of age 3. The complications were statistically more frequent only in patients with risk factors preceding the diagnosis of endocarditis. In our experience (table 3), complications related to endocarditis have decreased over time: from 85.7 % in 1960-1985 6 to 46.4 % in 1986-2000.
Theyjeh 17 et al reported a thirty year study in which the incidence of endocarditis and mortality remained stable. Children less than 2 years of age had an increased risk of mortality compared to older children 20,21. In our experience (table 3), mortality related to endocarditis has drastically decreased over the years: from 27 % in 1960-1985 6 to 12.5 % in 1986-2000. According to Coward 22 et al, mortality in children with congenital heart disease is now 12.5 % and according to Li 13 et al of 2-9 %; in our recent experience it has been 8.5 %. Mortality in healthy children without pre-existing heart disease has dropped from 55.6 % 6 to 16.7 %.
In conclusion: Endocarditis is a rare infection. The pediatrician must know that children with immunodeficiency or central venous catheters have an increased risk of developing endocarditis. Healthy children can have significant complications. In the recent series, complications and mortality have diminished considerably because of better echocardiographic techniques, efficient use of antibiotics and improved supportive measures during the course of the infection.