A girl aged 2 years presented with progressive respiratory difficulty, fever, hypotonic and areflexic tetraparesis, lower limb dysesthesia and aphonia.
The cerebrospinal fluid (CSF) analysis revealed pleocytosis (110 cells/µL), slightly elevated protein levels (0.6 g/L) and a normal glucose level. The electrophysiology study showed a reduced compound muscle action potential amplitude and decreased of motor unit recruitment. The magnetic resonance imaging (MRI) scan of the head and spine showed a T2-hyperintense lesion in the medulla oblongata, myelitis from C3 to C4 to the conus medullaris, with marked anterior horn involvement and enhancement in cervical and conus medullaris segments—as well as radiculitis—and the ventral roots of the cauda equina (Figs. 1 and 2). Polymerase chain reaction (PCR) testing of the CSF and serum identified Epstein–Barr virus (EBV) DNA (2100 and 270 000 copies/mL). Other possible causes were ruled out. After treatment with three intravenous immunoglobulin (IVIg) cycles, steroid therapy and acyclovir, the serum EBV load decreased (35 000 copies/mL) and there was progressive clinical and radiological improvement.
Medullomyeloradiculitis, axial view. T2-weighted images showed 2 symmetric hyperintense foci in the posterior medulla oblongata (arrows in A), confirmed selective involvement of anterior horns of the spinal cord, shown at the cervical (arrows in B) and conus medullaris (arrows in C) levels, with enhancement of the ventral roots of the cauda equina in the post-contrast axial T1-weighted image (arrows in D).
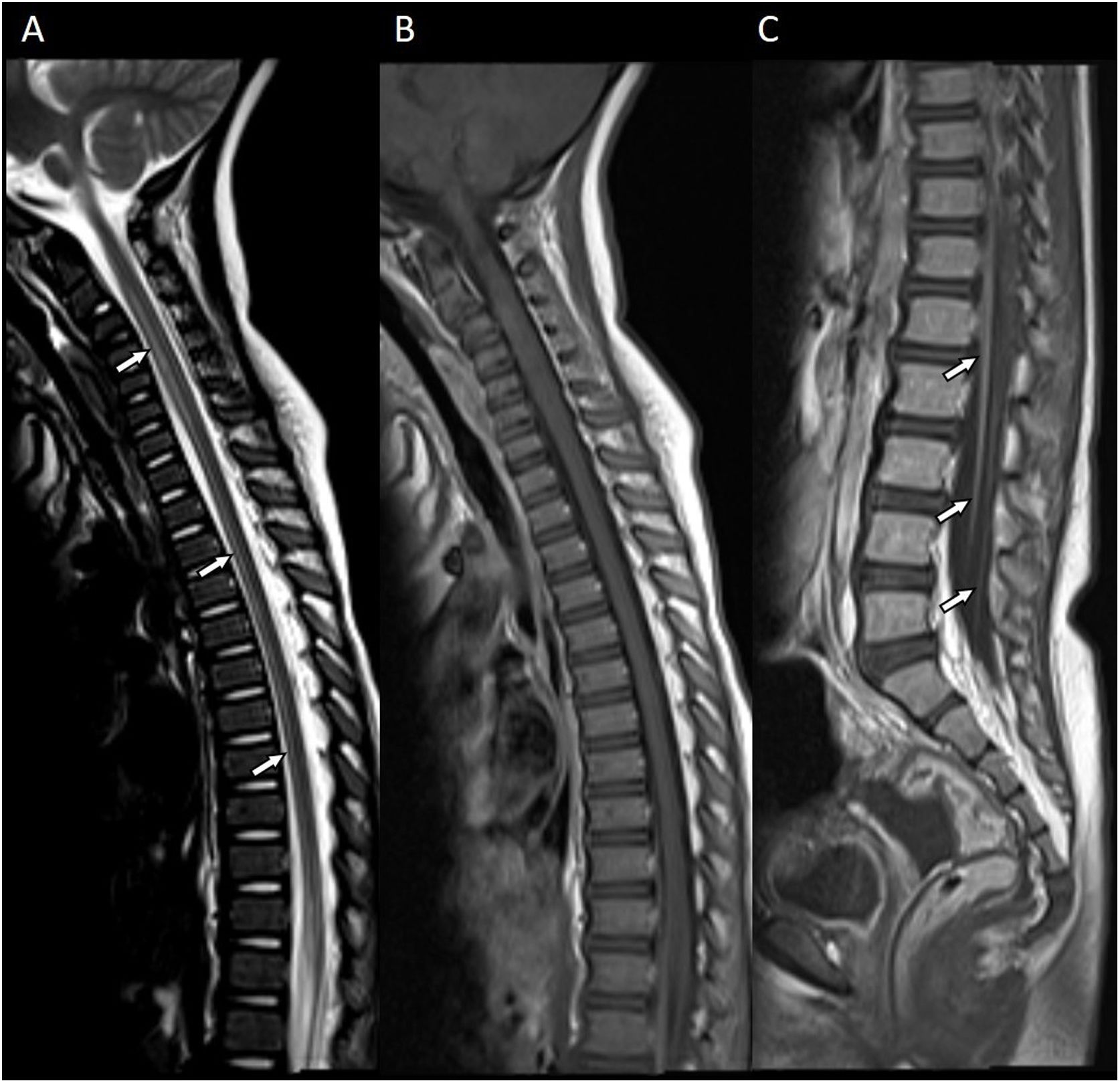
Spinal cord and cauda equina root involvement, sagittal view. Extensive anterior spinal cord hyperintensity from the cervical segment to the conus medullaris (arrows in A) in the T2-weighted image. The post-contrast sagittal T1-weighted image showed enhancement of the ventral roots of the cauda equina (arrows in C) and absence of enhancement in most of the spinal cord (B).
To the best of our knowledge, this is the first reported case exhibiting a combination of medullary, spinal cord, and radicular involvement associated with EBV; the infection presented with a polio-like pattern that has only been previously described in 2 cases.1–3 Involvement of the nervous system in EBV infection should be considered despite the presence of an atypical imaging pattern, even in immunocompetent patients.