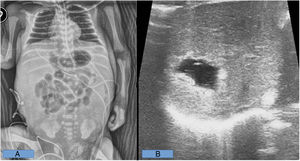
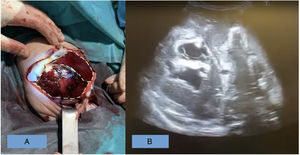
We write in relation to the article published by Torres del Pino et al, titled “Steps to improve umbilical vein catheterization in neonatal care”,1 which we have read with great interest. As the authors state, malposition of the catheter into the portal system causes complications that are relatively frequent and potentially severe, which warrants efforts to improve umbilical vein catheterization techniques in these patients. In this regard, we present two cases of exceptional complications resulting from umbilical vein catheter malposition.Case 1 Preterm male neonate born at 29+6 weeks of gestation admitted to the neonatal intensive care unit (NICU) due to prematurity and respiratory distress. He carried an umbilical vein catheter from admission, which was used from day 2 to day 5 for parenteral nutrition. On day 5, the catheter was removed because the patient could tolerate enteral feedings. On day 6, the NICU consulted with the paediatric surgery department for assessment of abdominal distension and rapidly progressive swelling of the abdominal wall. The patient required invasive ventilation and vasoactive drugs. During the followup, there was no evidence of pneumoperitoneum or enterocolitis in the serial abdominal radiograph. The patient developed progressive ascites with central crowding and collapse of the bowel loops. The findings of laboratory tests were also not suggestive of enterocolitis. These findings persisted on day 7. An ultrasound examination revealed left portal vein thrombosis, a focal cystic in segment iva of the left liver lobe compatible with extravasation and moderate to severe ascites with septations and floating echogenic foci within (enterocolitis was not ruled out). Due to the considerable clinical severity and the diagnostic uncertainty, an abdominal tap was placed, with immediate discharge of a large amount of cloudy fluid, compatible with the extravasation of parenteral nutrition. The patient had a favourable outcome, with extubation and removal of the abdominal tap 2 days later and no further abdominal manifestations. Female neonate born at 31+4 weeks of gestation admitted to the NICU for prematurity and respiratory distress, with a favourable course. On day 9 post birth she developed hypotension, anaemia and rapidly progressing abdominal distension. An urgent laparotomy was performed after medical resuscitation measures failed. The procedure evinced massive intraperitoneal haemorrhage, with remnants of parenteral nutrition, secondary to right liver rupture. There was an 8 cm laceration in segments vii-viii, with a smaller lateral laceration in segment vi, both actively bleeding. The portal vein system was intact and there was generalised hypoperfusion in the bowel. Intraparenchymal extravasation of parenteral nutrition administered through the umbilical vein catheter was identified as the cause of liver rupture. Different haemostatic techniques were attempted without success, and the intervention was brought to an end with abdominal packing as a temporary measure to consider the next step. In the hours that followed, the patient’s condition worsened, leading to multiple organ failure and eventually death (Figs. 1 and 2). Association of clinical and imaging features. A: shows the difference between the right liver (presence of cyst resulting from parenteral nutrition and superficial bursting of the liver with hypoperfused areas) and left liver (normal appearance). B: shows the intraparenchymal cysts and free fluid.
In conclusion, the complications of umbilical vein catheter malposition can be severe and pose a significant diagnostic and therapeutic challenge.2,3 In consequence, we congratulate our colleagues on the implementation and improvement of neonatal umbilical vein catheterization techniques, thereby improving the safety of the technique and reducing the incidence of adverse events in neonatal patients.