We present the case of a female adolescent aged 12 years admitted to hospital with fever and frontal headache of 5 days’ duration associated with somnolence and vomiting. The salient findings of the physical examination were ptosis and drooping of the left corner of the mouth.
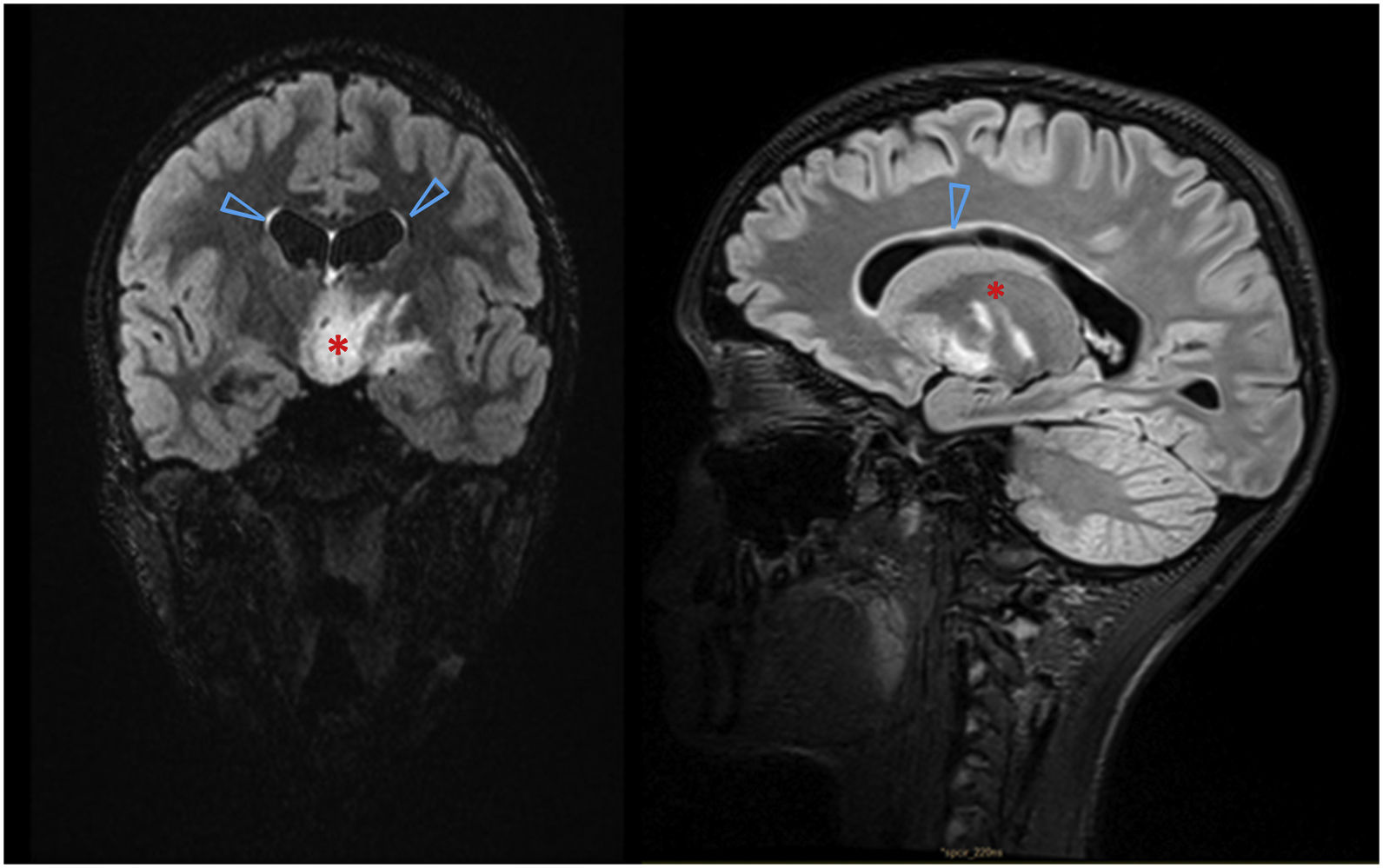
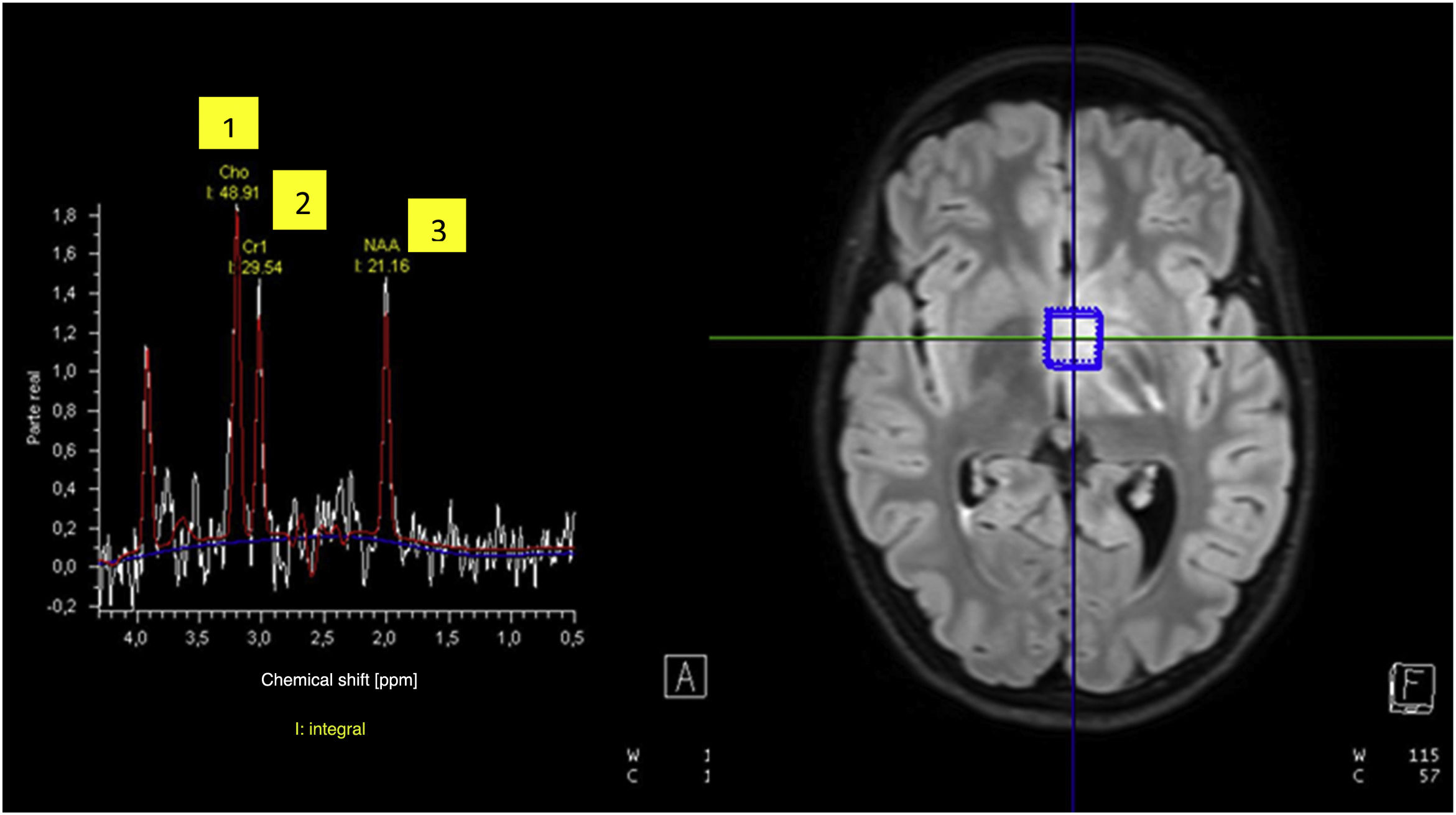
Papilledema was ruled out and the evaluation completed with head CT and MRI scans (Fig. 1). Based on the imaging findings, the principal diagnostic impression was diffuse midline glioma, although an inflammatory process could not be ruled out. This prompted extension of the evaluation with magnetic resonance spectroscopy (MRS), the findings of which were inconclusive for diagnosis of a tumor (Fig. 2). The surgical biopsy was deferred to perform a 11C-methionine PET scan, the findings of which were not suggestive of high grade glioma. Suspicion of autoimmune encephalitis prompted testing for anti-MOG/AQP4 antibodies (which turned out negative) and initiation of intravenous steroid therapy.1
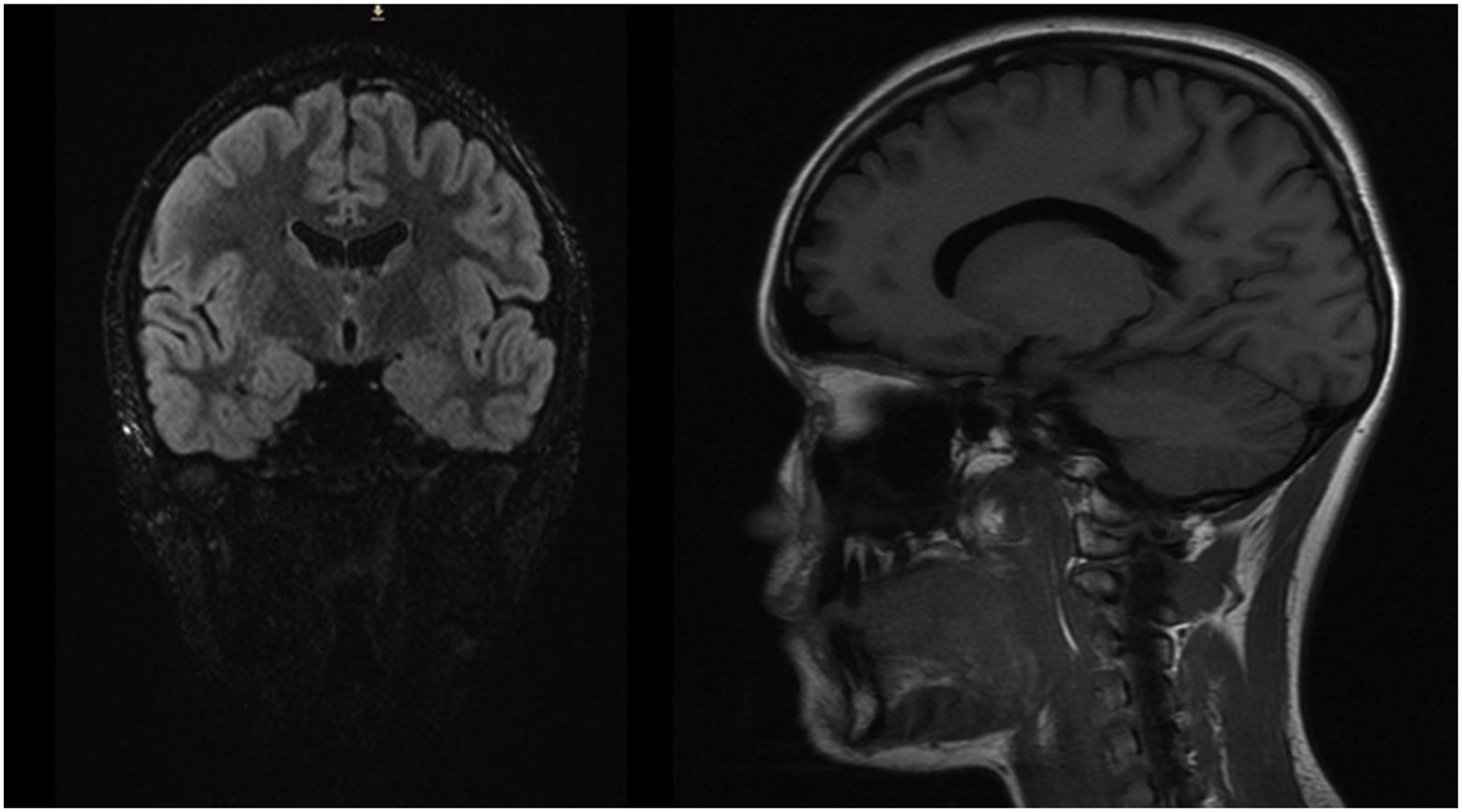
At 2 months of treatment, the neurologic symptoms had resolved and there was significant radiological improvement, with full resolution of the lesion at 5 months (Fig. 3), which confirmed the inflammatory etiology.
Thus, we can conclude that not every intracranial midline lesion is a tumor. Tools such as MRS are useful for the differential diagnosis of these lesions.2,3