On March 14, 2020, the Spanish government declared a state of alarm in response to the health crisis caused by SARS-CoV-2 (Royal Decree 463/2020), which ended on July 5, 2023 (Order SND/726/2023). The protective measures adopted during this period (hygiene and social distancing) brought on important epidemiological changes in different infectious diseases.1,2
To our knowledge, no studies analyzing the impact on the epidemiology of invasive bacterial infections (IBIs) in infants aged less than 3 months with fever without a source (FWS) have been published in Spain.
We conducted a secondary descriptive analysis of a retrospective multicenter register that included all infants aged up to 90 days with FWS managed between May 1, 2022 and April 30, 2023 in 24 pediatric emergency departments in Spain. The aim was to analyze the incidence of IBI in infants under 3 months with FWS in the late phase of the public health crisis due to SARS-CoV-2 and the causative bacteria involved in these cases. We defined IBI as detection of a bacterial pathogen in blood (bacteremia) or cerebrospinal fluid (bacterial meningitis) through culture or polymerase chain reaction (PCR). We defined urinary tract infection (UTI) as a positive urine culture (growth with ≥1000 CFU/mL of a single pathogen in culture of a urine specimen obtained through suprapubic aspiration, or growth with >10 000 CFU/mL of a single pathogen in culture of a urinary catheter specimen) in addition to abnormal results in the urine dip test (positive result for leucocyte esterase or nitrites in urine specimen collected with sterile technique). The study was approved by the Research and Ethics Committee of the Basque Country (code PI2021044).
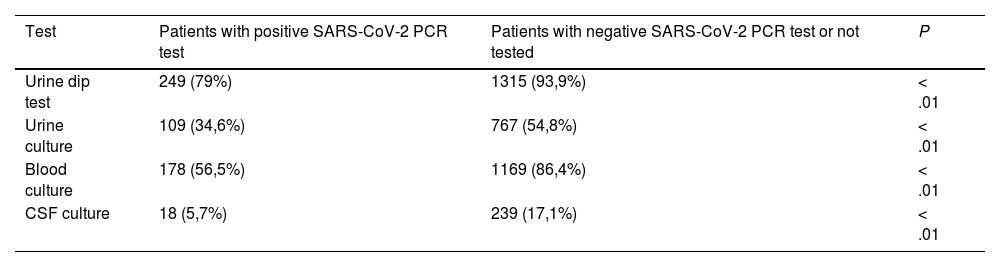
The sample included 1716 patients (1013 [59.0%] male; median age, 50 days [IQR, 31–67]), of who 96.4% were in good general health on arrival. A urine dip test was performed in 1564 patients (91.6%), urine culture in 876 (51%), blood culture in 1347 (78.5%) and cerebrospinal fluid (CSF) culture in 257 (15%), with significant differences in relation to having a positive PCR test result for SARS-CoV-2 (Table 1).
Diagnostic tests performed in relation to SARS-CoV-2 PCR test results.
| Test | Patients with positive SARS-CoV-2 PCR test | Patients with negative SARS-CoV-2 PCR test or not tested | P |
|---|---|---|---|
| Urine dip test | 249 (79%) | 1315 (93,9%) | < .01 |
| Urine culture | 109 (34,6%) | 767 (54,8%) | < .01 |
| Blood culture | 178 (56,5%) | 1169 (86,4%) | < .01 |
| CSF culture | 18 (5,7%) | 239 (17,1%) | < .01 |
CSF, cerebrospinal fluid; PCR, polymerase chain reaction.
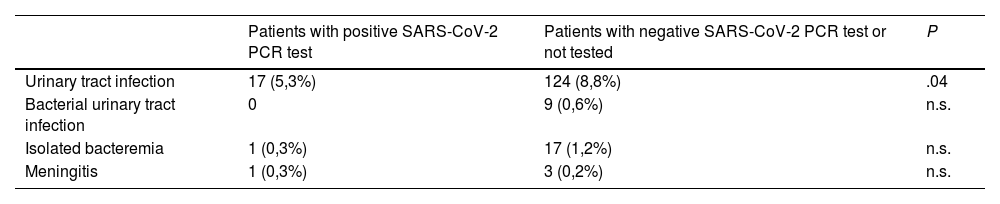
There were a total of 141 diagnoses of UTI (8.2%) and 31 of IBI (1.8%): 18 of bacteremia, 9 of UTI associated with bacteremia and 4 of meningitis (one of them of urological origin and all of them with associated bacteremia). The most frequent causative agents in IBI cases were Escherichia coli (10 [32.3%]), Streptococcus agalactiae (5 [16.1%]) and Staphylococcus aureus (4 [12.9%]). In the case of meningitis, the causative agents were E coli (1), S agalactiae (1), Streptococcus gallolyticus (1) and Streptococcus pneumoniae (1). The frequency of IBI was 3.7% in infants aged up to 30 days, 1.5% in the group aged 31–60 days and 0.7% in the group aged 61 and 90 days (P < .01); and, in relation to the PCR test for detection of SARS-CoV-2, 0.6% in patients with a positive result vs 2.1% in the rest of patients (P < .05). Table 2 shows the distribution of bacterial infections in relation to the SARS-CoV-2 PCR test results.
Type of bacterial infection in relation to positive SARS-CoV-2 PCR results.
| Patients with positive SARS-CoV-2 PCR test | Patients with negative SARS-CoV-2 PCR test or not tested | P | |
|---|---|---|---|
| Urinary tract infection | 17 (5,3%) | 124 (8,8%) | .04 |
| Bacterial urinary tract infection | 0 | 9 (0,6%) | n.s. |
| Isolated bacteremia | 1 (0,3%) | 17 (1,2%) | n.s. |
| Meningitis | 1 (0,3%) | 3 (0,2%) | n.s. |
n.s., not significant; PCR, polymerase chain reaction.
Overall, 436 patients (25.4%) received antibiotherapy (7.6% of patients with a positive SARS-CoV-2 PCR test vs 29.4% of the rest of patients; P < .01) and 651 (38%) were admitted to hospital (20.3% of patients with a positive SARS-CoV-2 PCR test vs 41.9% of the rest of patients; P < .01).
The frequency of IBI in infants aged up to 90 days with FSF and the distribution of bacterial causative agents were similar to those observed in the prepandemic period, with E coli remaining the leading cause of IBI.3,4 The prevalence of bacterial meningitis was 0.23%, and all cases occurred in infants aged less than 60 days.
Based on our findings, among infants aged up to 90 days with FWS, the proportion of IBI was lower in the subset who had a positive test result for SARS-CoV-2, although the difference was not statistically significant. Burstein et al.5 also found a lower prevalence of IBI in febrile infants aged up to 90 days who had a positive SARS-CoV-2 result (1%). A meta-analysis that included nearly 4000 febrile infants found an even lower prevalence: 0.56% in the group aged up to 21 days, 0.53% in the group aged 22–28 days and 0.11% in the group aged 29–60 days.6 The authors concluded that infants aged more than 28 days with a positive SARS-CoV-2 test result could be managed conservatively without blood tests, although given the heterogeneity of the inclusion criteria in the reviewed studies, the authors recommended caution in the management of infants in whom the presenting complaint was FWS, as was the case in our study. This is an important aspect, as, according to our findings, the management of these patients changes if there is a positive SARS-CoV-2 result, which highlights the need to conduct additional studies to determine the appropriateness of diagnostic tests in infants aged less than 3 months with FWS and a positive result for SARS-CoV-2.
FundingThis research did not receive any external funding.
Amaia Cámara (HU Donostia, San Sebastián), Ana Muñoz (HU Infanta Leonor, Madrid), Andres González (HU Basurto, Bilbao), Anna Orejuela (Hospital Joan XXIII, Tarragona), Anna Pizà (HU Mútua de Terrasa, Terrasa), Antón Castaño (HU de Cabueñes, Gijón), Clara Ferrero (HU Gregorio Marañón, Madrid), Clàudia Coderch (H. de Terrassa CST, Terrassa), Daniel de la Rosa (CHUIMI Las Palmas de Gran Canaria, Las Palmas de Gran Canaria), Roberto Velasco, Elena Granda (Hospital Universitario Río Hortega, Valladolid), Irene Baena (Corporació Sanitària Parc Taulí, Sabadell), Jone Amasorrain (H. de Mendaro, Mendaro), Laura Díaz (HU Santa Creu i Sant Pau, Barcelona), Leticia González (H. de Segovia, Segovia), Maria Amalia Pérez (Hospital de Zumárraga), Maria José Carbonero (HU Virgen del Rocío, Seville), Mariano Plana (H. Barbastro, Barbastro), Nuria Clerigué (CHU de Navarra, Pamplona), Núria Gilabert (HU Son Espases, Palma de Mallorca), Sofía Piera (HU Sant Joan, Reus, Tarragona), Virginia Gómez (HU Miguel Servet, Zaragoza), Yudith Mesa (HU de Canarias, La Laguna, Santa Cruz de Tenerife).
Previous presentation: XXVIII Annual Meeting of the Sociedad Española de Urgencias de Pediatría; May 9–11, 2024; online.
Appendix A lists the members of the Working Group on Care Quality in the Management of Febrile Infants of the Research Network of the Sociedad Española de Urgencias de Pediatría (RISEUP-SPERG) who participated in the study.