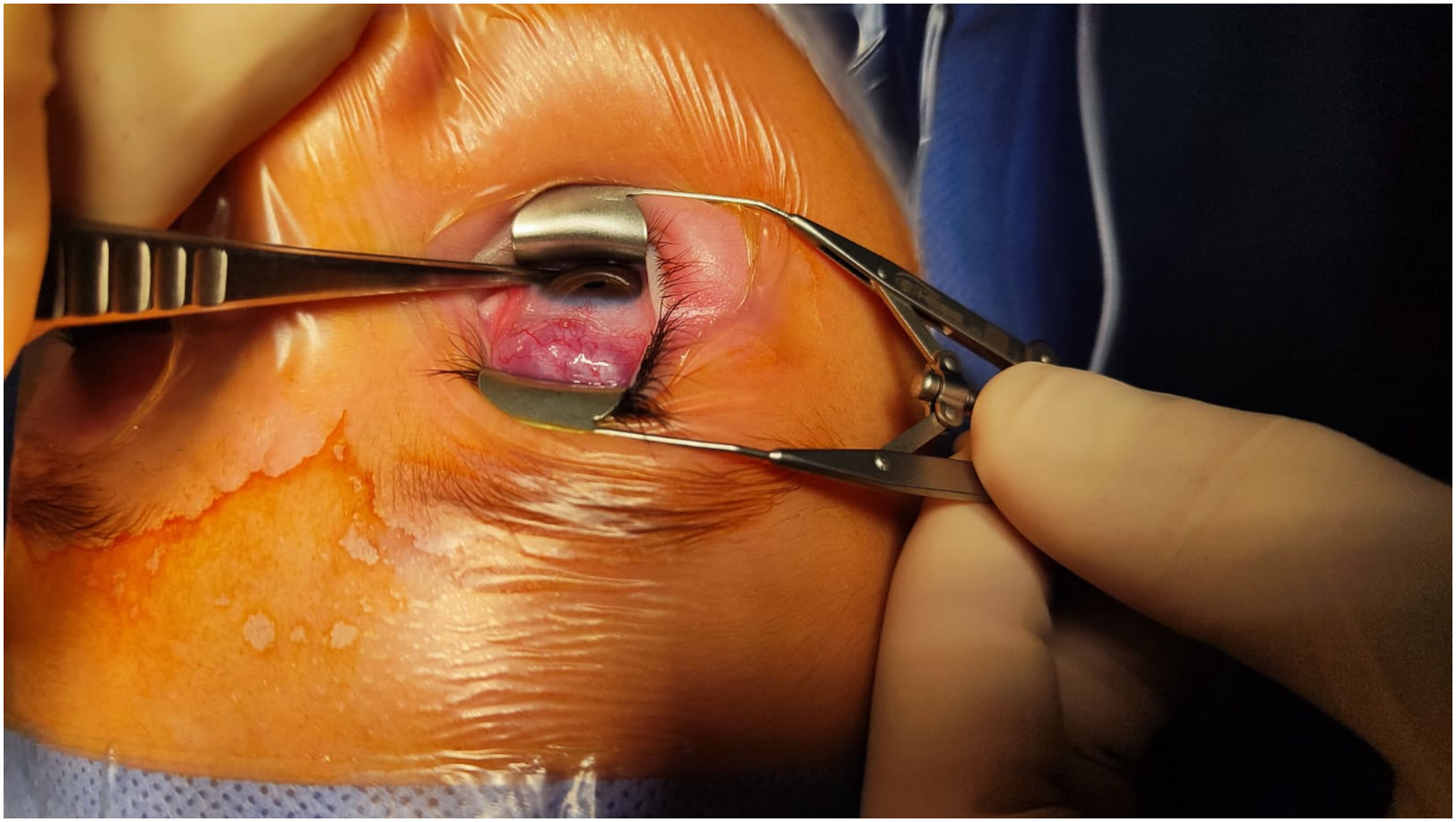
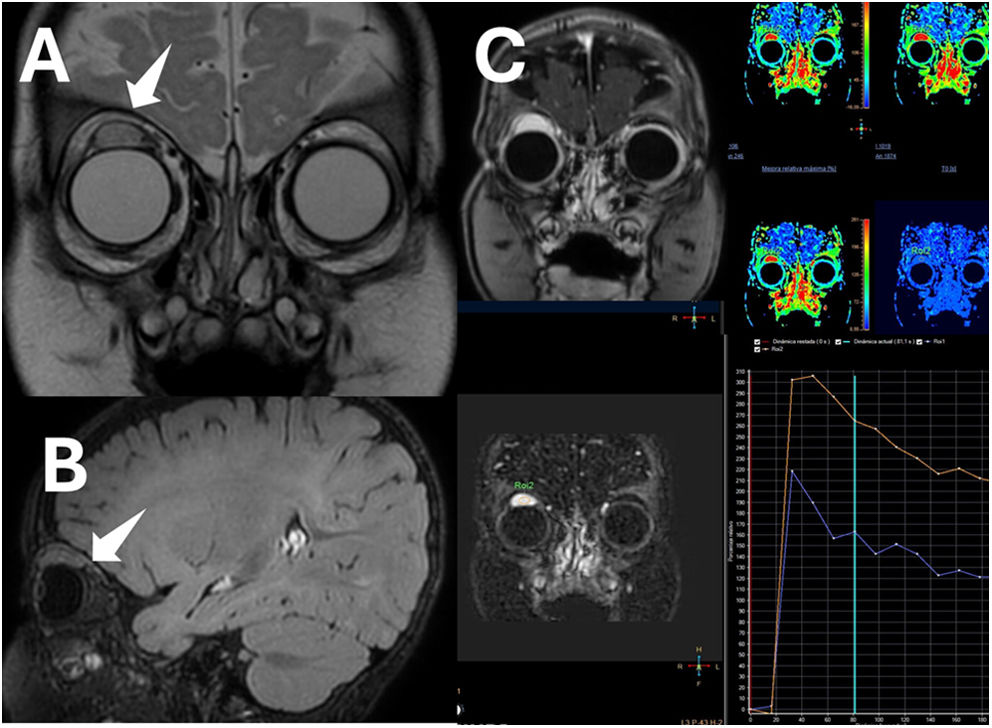
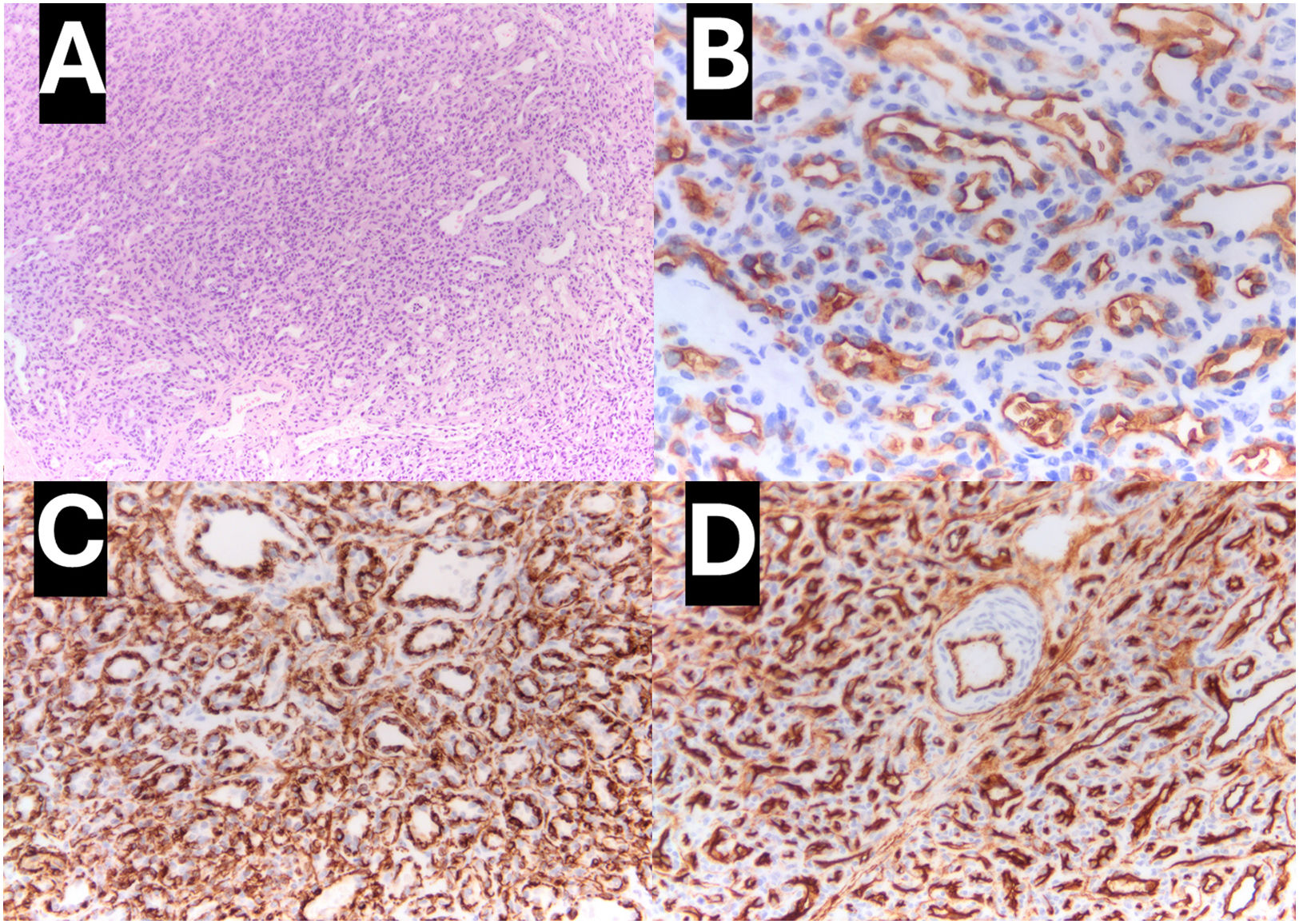
An infant aged 4 months was referred for assessment of a purplish mass in the posterior surface of the right upper eyelid (Fig. 1), with no other abnormalities in the ophthalmological examination. Magnetic resonance imaging revealed a well-defined intramuscular mass in the superior rectus muscle of the right eye with characteristics suggestive—but not pathognomonic—of hemangioma (Fig. 2). The patient underwent an incisional biopsy at age 9 months. The histological analysis revealed proliferation of small-caliber vessels without atypia. Immunohistochemical staining was positive for GLUT-1, CD34 and WT-1, confirming the diagnosis of infantile hemangioma (Fig. 3). The patient started treatment with oral propranolol (Hemangiol), which was well tolerated and achieved a favorable response.1 Follow-up MRI scans showed progressive involution and fibrotic changes.
Magnetic resonance imaging. (A) Coronal view and (B) sagittal view showing a homogeneous lesion, hyperintense on T2-weighted imaging, in the distal portion of the superior rectus muscle of the right eye, near the insertion on the globe, measuring 16 × 14 × 16 mm (anteroposterior × transverse × craniocaudal diameters), with a hypointense border corresponding to a pseudocapsule, showing facilitated diffusion, without calcification or bleeding within the lesion. (C) Dynamic contrast-enhanced MRI, fat-suppressed T1-weighted images showing a type 3 kinetic curve with a rapid uptake followed by a progressive reduction on the late phase (washout). Post-contrast imaging of the right superior rectus muscle showing homogeneous enhancement.
Infantile hemangioma is the most frequent benign vascular tumor of infancy; it is absent at birth to then present in the first weeks of life, with a natural history in three phases: proliferation, stabilization and involution.2 The differential diagnosis includes rapidly involuting congenital hemangioma, present from birth and with rapid spontaneous involution, and non-involuting congenital hemangioma, which persists over time and is negative for GLUT-1 expression.3
The salient features of this case were the atypical location combined with the typical clinical course of orbital infantile hemangioma.