Urinary tract infection (UTI) is the most common bacterial infection in infants with fever without source (FWS).1 Until 2024, the protocols for the management of febrile infants of the Asociación Española de Pediatría (Spanish Association of Pediatrics) and the Sociedad Española de Urgencias de Pediatría (Spanish Society of Pediatric Emergency Medicine) recommended systematic screening for UTI by assessing for the presence of leukocytes or nitrites in urine through a urine test strip (UTS) in all infants aged less than 3 months with FWS, as well as in infants aged 3–6 months, in the latter group only if they presented to the emergency department with a fever of 39 °C or higher or of more than 48 h’ duration.2 However, the UTI protocol of the Asociación Española de Pediatría highlights the importance of systematic screening by means of a UTS of all infants with FWS.3 In 2024, the febrile infant management protocol was modified, expanding the recommendation of screening for UTI to all infants aged less than 6 months with FWS, independently of the severity of the fever.4 That is, the recommendation of systematic screening for UTI was expanded to include infants aged 3–6 months with FWS of less than 39 °C.
To assess the impact of systematic UTI screening in infants aged 3–6 months with FWS, we conducted a multicenter, retrospective and observational cohort study including all infants younger than 6 months with FWS who visited the pediatric emergency departments (PEDs) of three hospitals between January 2023 and June 2024. One of these hospitals had already implemented the recommendation for systematic UTI screening in all infants aged less than 6 months of age, while the other two continued to implement the traditional strategy. We analyzed the management of the infants in the emergency department and the follow-up in primary care and compared the final prevalence of UTI in the patients based on the implemented approach. Urinary tract infection was defined as abnormal urine test results (leukocyturia and/or positive nitrite test) and growth of a bacterial pathogen with at least 10 000 CFU/mL in a urine culture performed with a specimen collected with sterile technique.
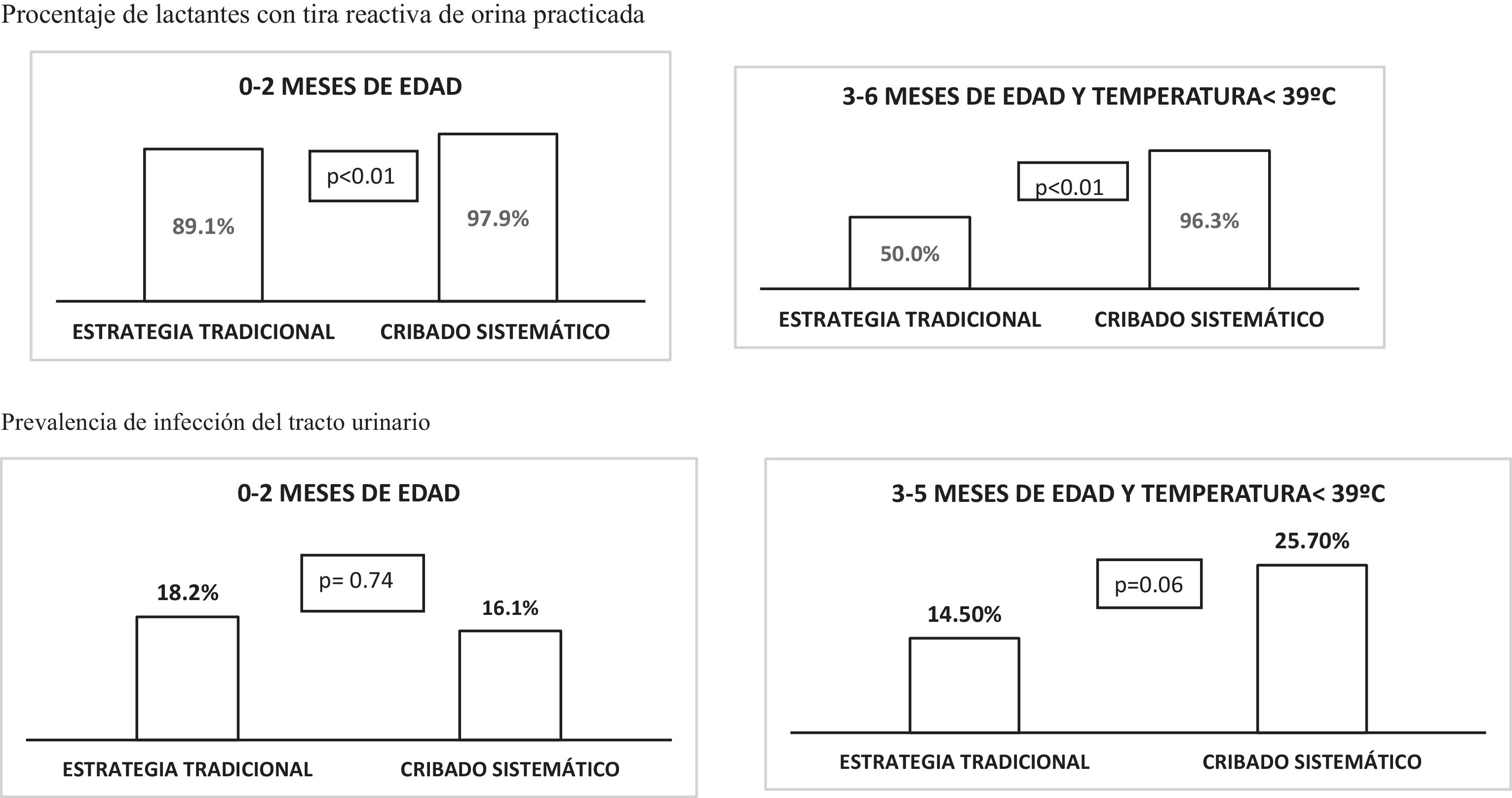
We identified 171 episodes corresponding to infants aged 3–6 months with FSF of less than 39 °C during the study period (109 in the center with systematic screening and 62 in the centers with traditional screening). Of all these patients, 37 (21.6%) received a final diagnosis of UTI (28/109 [25.7%] in the hospital with the new protocol vs 9/62 [14.5%] in the hospitals with the traditional protocol; P = .06). In the hospital with systematic screening, a UST was performed in 105 infants (96.3% compared to 31% and 50.0% in the hospitals with traditional screening; P < .01), with abnormal findings in 39 of them. In addition, there were 346 documented episodes in infants aged less than 3 months with FWS: 236 in the center with systematic screening of older infants and 110 in centers with traditional screening. In the former, screening with a UTS was performed in 231 infants (97.9%) compared to 98 (89.1%) in the other two hospitals (P < .01). The prevalence of UTI in infants aged less than 3 months was similar in all centers (16.1% in the hospital with systematic screening vs 18.2% in the centers with traditional screening, not significant) (Fig. 1).
Systematic screening for UTI in the emergency department in infants aged 3–6 months with a temperature of less than 39 °C doubled the frequency of a final diagnosis of UTI, a difference that would probably have been even greater if, in adherence to previous recommendations, a UTS had not been used for screening in the emergency department in any of the infants in this age range with a temperature of less than 39 °C.
The higher rate of UTI in infants aged 3–6 months can be explained by more selective visits to the emergency departments in this age group, in which a higher percentage is referred by the primary care pediatrician, compared to infants aged less than 3 months, who are frequently brought to the emergency department almost as soon as a fever is detected, in addition to visits due to fever following administration of the first vaccines.
On the other hand, screening for leukocytes or nitrites in urine is one of the essential quality indicators in the management of febrile infants aged less than 3 months.5 Like others before, our study evinces interhospital variation in clinical practice and issues with adherence to protocols.
The main limitation of this study was the small sample size, which may have contributed to the lack of statistical significance in the difference in UTI diagnoses based on the UTI screening strategy applied to infants aged 3–6 months with FSF of less than 39 °C.
The indications for the performance of a UTS in febrile infants aged more than 2 months remain controversial. Although testing could be performed by the primary care pediatrician during the follow-up, our findings suggests that the systematic implementation of UTI screening in the emergency department in infants aged 3–6 months with FSF of less than 39 °C enables the identification of a significant number of UTI cases, supporting a change in the guidelines for the management of these patients.
Meeting Presentation: this study was presented at the XXIX Annual Meeting of the Sociedad Española de Urgencias de Pediatría; May 22–24, 2025.