Sleep quality has positive effects on children’s sleep and eating habits. In turn, improvement in sleep quality is associated with sleep hygiene training. The aim of our study was to determine the impact of sleep hygiene education on sleep and nutrition management in children aged 10–18 years. In addition, we explored the association between sleep problems and eating behaviours in participants before and after the training programme.
MethodsWe conducted a quasi-experimental study between August 25 and December 27, 2023, in children aged 10–18 years who participated in the study on a voluntary basis with the consent of their parents. We collected data from a total of 80 children aged 12–18 years. The study investigated the relationship between sleep problems and eating behaviours. We randomly allocated participants to one of two groups, the training group or the waitlist group. We assessed the association between changes in sleep problems and changes in eating behaviours in the training group. The data were collected using a sociodemographic data form, the Children’s Sleep Habits Questionnaire, and the Three-Factor Eating Questionnaire.
ResultsIn the study sample, the proportions of male and female participants (training group) were 60.0% and 40.0%, respectively. There was a statistically significant difference between the pretest and post-test scores in the Children’s Sleep Habits Questionnaire and the Three-Factor Eating Questionnaire (P < .01) and significant differences in the changes in sleep and eating habit scores between groups between the pre- and post-sleep hygiene training timepoints (P < .01). Thus, we concluded that sleep hygiene training is associated with and has an impact on sleep and nutrition.
ConclusionWe observed that in children aged 10–18 years, sleep problems were associated with their eating behaviours. Sleep hygiene education had a significant and favourable impact on sleep and nutrition outcomes. Thus, sleep hygiene training has an important effect on children’s sleep and diet.
La calidad del sueño tiene efectos positivos en los hábitos de sueño y alimentación de los niños. La mejora de la calidad del sueño también está relacionada con la formación en higiene del sueño. Este estudio se realizó para determinar el impacto de la educación en higiene del sueño en el control del sueño y la nutrición en niños de 10 a 18 años. Además, intentamos explorar la asociación entre los problemas de sueño y las conductas alimentarias entre ellos antes y después del programa de formación.
MétodosSe realizó un estudio cuasiexperimental del 25 de agosto al 27 de diciembre de 2023, con niños de 10 a 18 años que participaron voluntariamente en el estudio con el consentimiento de sus padres. Se recogieron datos de un total de 80 niños de 12 a 18 años. El estudio investigó la relación entre los problemas de sueño y las conductas alimentarias. Los categorizamos en dos grupos aleatoriamente y un grupo se clasificó en el grupo de entrenamiento y los otros en el grupo de lista de espera. Exploramos la asociación entre los cambios en los problemas de sueño y los cambios en las conductas alimentarias entre el grupo de entrenamiento. Los datos se recopilaron utilizando las siguientes herramientas: formulario de datos sociodemográficos, cuestionario de hábitos de sueño del niño (CSHQ) y escala de alimentación de tres factores (TFEQ).
ResultadosEntre los participantes, la proporción (grupo de entrenamiento) de niños y niñas participantes fue de 60,0% y 40,0%, respectivamente. Existe una diferencia estadísticamente significativa entre los cambios en las puntuaciones de la encuesta de hábitos de sueño de los niños antes y después de la prueba y las puntuaciones de la escala de alimentación de tres factores (p < 0,01) y una diferencia significativa entre las puntuaciones de los grupos en términos de entrenamiento de higiene del sueño y la gestión de la nutrición antes y después del sueño (p < 0,01). Se concluyó que el entrenamiento en higiene del sueño tiene una relación y un efecto entre el sueño y la gestión de la nutrición.
ConclusiónObservamos que los problemas de sueño de los niños de 10 a 18 años estaban asociados con sus conductas alimentarias. La educación en higiene del sueño impactó significativamente y de manera positiva el sueño y la gestión de la nutrición. Por lo tanto, el entrenamiento en higiene del sueño tiene un efecto importante en la calidad del sueño de los niños y la gestión nutricional.
Sleep is a fundamental physiological process and a biological need, just like air, water and food. It is crucial for the health and wellbeing of all living things, and, especially for adolescents, it is significant for growth and development.1 Sleep problems are common among children during physical development; however, especially among adolescents, they can give rise to important physiological and psychological issues that have a significant impact on their families and caregivers.2 Furthermore, it is crucial to protect children from issues related to sleep and/or poor sleep habits.3 Therefore, it is necessary to evaluate sleep quality and habits in children in the assessment of related issues that can impact their development and quality of life. This could facilitate timely intervention to preclude future risks.
Nutrition refers to the process of consuming and utilizing the nutrients required for growth, development, and a long, healthy and productive life. Inadequate and poor-quality sleep, inadequate and unbalanced nutrition and unhealthy eating habits may have a deleterious effect on children’s quality of life. A recent study found that sleep restriction had a negative impact on certain endocrine system functions and induced changes in appetite, with stimulation of the hormone ghrelin and the anorexigenic hormone leptin, concluding that school-aged children should get 8–10 h of sleep. Another study concluded that school-aged children should sleep 8.5–10 h a night, as insufficient sleep could lead to irritability and lack of attention, resulting in poor academic performance and also sleep problems, especially in families and caregivers; insufficient sleep, in addition, frequently causes emotional problems, such as stress and irritability, and physiological problems, such as fatigue or waist or back pain.4,5
There is robust evidence that dietary and sleeping habits are related.6 It is believed that insufficient or poor-quality sleep and inadequate and unbalanced nutrition and dietary habits contribute to the increasing prevalence of obesity among children and adolescents. A study found that sleep restriction negatively affects selected endocrine system functions and causes changes in the levels of the appetite-stimulating hormone ghrelin and the anorexigenic hormone leptin.7 Another study concluded that school-aged children should sleep 8.5–10 h. Emphasis has been placed that insufficient sleep can lead to irritability and attention deficit in children, resulting in poor academic performance and unbalanced eating habits.8 Sleep deprivation has a direct impact on weight gain, unbalanced and inadequate nutrition and dietary habits and may significantly increase the risk of overweight and obesity, especially in children aged 10–18 years.
Sleep hygiene encompasses practices to improve sleep quality and plays a significant role in preventing sleep-related problems.9 Sleep hygiene training and education have positive effects on children’s sleep quality, eating habits and management. In a study conducted by Geiger-Brown et al.,10 a 15-week sleep training intervention mitigated children’s sleep and eating issues. Another study in parents of children with autism spectrum disorder (ASD) aged 2–10 years found that sleep training had a positive effect on sleep duration.10 Reed et al.11 evaluated the effectiveness of a sleep education workshop with a small group format. Each group included 3–5 families, with a total of 20 families of children with ASD participating in the programme. The ages of the children ranged between 3 and 10 years. The results showed that the sleep education programme had positive effects on children’s sleep habits, nutrition and daytime behaviour as well as on family stress levels. A study by Gavela-Pérez et al.,12 concluded that sleep habits directly affect eating habits and that eating habits are healthier and more balanced as sleep quality increases. A study by Bhurosy and Thiagarajah13 found a negative impact on daily activities in students with poor sleep quality and eating habits. Zhao et al.14 reported that adolescents who could not keep a healthy and balanced diet had poor sleep quality and could not maintain healthy sleep.
In a study conducted in high school students by de Castro Corrêa et al.,15 the authors concluded that delivery of sleep hygiene education to high school students had a positive impact on both sleep and healthy and balanced dietary habits. A study by LeBourgeois et al.16 found that sleep problems decreased after sleep hygiene education, as did unbalanced eating problems in dietary patterns. In the study of Malik et al.,17 the authors concluded that sleep hygiene practices had positive effects on daily quality of life as well as physiological needs in eating habits.
The main reason for considering both sleep and diet within the scope of the intervention was that sleep problems and nutritional deficiencies are frequently observed in children aged 10–18 years and have an adverse impact on their social and academic lives. Since sleep and diet affect every aspect of social life, an association between them is inevitable.
The aim of the study was to determine the effect of sleep hygiene education on sleep and diet in children aged 10–18 years. We hypothesised that (1) sleep problems in children aged 10–18 years are associated with their eating behaviours, (2) there would be differences in sleep problems between children aged 10–18 years who received sleep hygiene education versus those who did not (H1), (3) there would be differences in eating behaviours between children aged 10–18 years who received sleep hygiene education versus those who did not (H1), and (4) changes in sleep problems after the training programme would be associated with changes in eating behaviours.
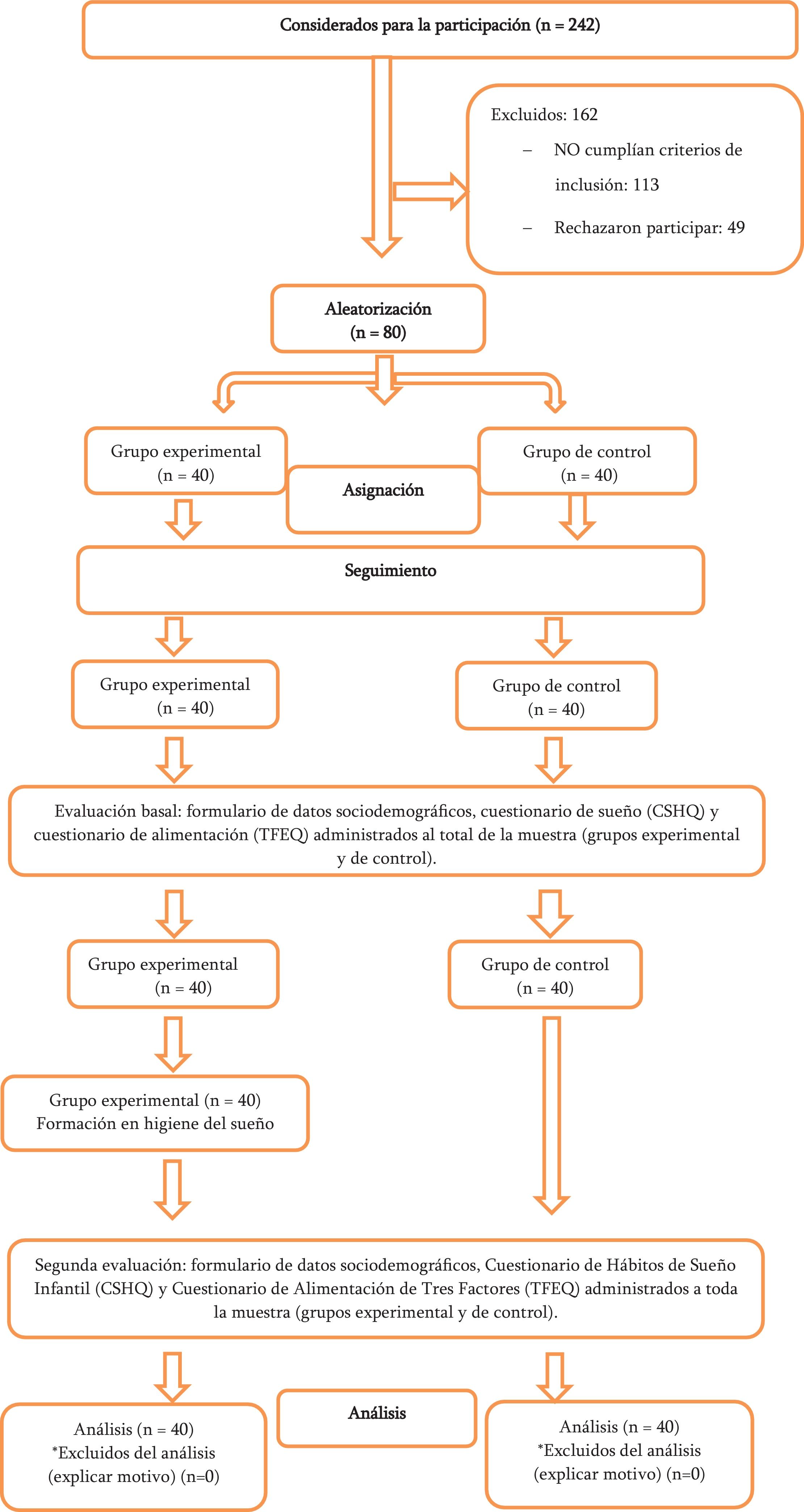
Material and methodsParticipantsWe conducted a quasi-experimental study between August 25 and December 27, 2023 in children aged 10–18 years from Eskişehir, whose participation was voluntary. We estimated the sample size using the software G*Power, version 3.1.9.2. Based on the findings of the 2019 study by Rafihi-Ferreira et al.,18 we assumed that the effect size for the sleep parameter was high (f = 1.5). We expected the effect size in our study to be large. Accordingly, we estimated that the sample size required to achieve a 95% power (1 − β = 0.95, effect size f = 0.5) for an α level of 0.05 would be of 80 participants.
Of the 242 children considered for participation, a total of 80 were included in the sample. The inclusion criteria were age 10–18 years, parental consent, and signing of the assent form by the child. Patients who did not meet all of these criteria were excluded from the study. We randomly allocated participants to the training group (n = 40) or the waitlist group (n = 40) (Fig. 1).
Trainings were conducted face-to-face in the conference room arranged by the research team. The data were collected online due to the lower cost, easy access, accuracy and reliability of this approach. Despite the in-person training format, data on the demographic characteristics such as the age, sex, and educational status of the children were collected through an online questionnaire (Google Forms platform) disseminated and accessed through social networks and media.
Rating scalesSocio-Demographic Data Collection Form: This form consists of 3 questions about the age, sex and educational status of the children. Children’s Sleep Habits Questionnaire (CSHQ): The CSHQ-Short Form, developed by Owens et al. in 2000 to investigate children’s sleep habits and sleep-related problems, comprises 33 items.19 The validity and reliability study of the Turkish version was conducted by Perdahli Fiş et al.,20 from whom we obtained permission for its use. The domains include bedtime resistance (items 1, 3, 4, 5, 6, and 8), sleep onset delay (item 2), sleep duration (items 9, 10, and 11), sleep anxiety (items 5, 7, 8, and 21), night wakings (items 16, 24, and 25), parasomnias (items 12, 13, 14, 15, 17, 22, and 23), sleep-disordered breathing (items 18, 19, and 20), and daytime sleepiness (items 26, 27, 28, 29, 30, 31, 32, and 33). The questionnaire is completed retrospectively by the parents. Parents are asked to recall their child’s sleep behaviours over the previous week. The items are rated on the following 3-point scale: “usually” (3 points: the specified behaviour occurred 5–7 times/week), “sometimes” (2 points: behaviour occurred 2–4 times/week) and “rarely” (1 point: 0–1 times/week). Items 1, 2, 3, 10, 11, and 26 are reverse-coded (“usually” 1 point; “sometimes” 2 points; “rarely” 3 points). The answer choices for the 32nd and 33rd items are “not sleepy” (0 points), “very sleepy” (1 point) and “falls asleep” (2 points). Children who score a total of 42 points or more on the questionnaire are considered to have clinically significant sleep problems. The questionnaire also includes three open-ended questions regarding the child’s sleep habits (bedtime, time spent sleeping during the whole day, and time spent awake at night). In the validity and reliability study of the Turkish version of the questionnaire; the assessment of the internal consistency yielded a Cronbach α coefficient of 0.78 and a test-retest correlation coefficient of 0.81.
Three-Factor Eating Questionnaire (TFEQ): Bryant et al.21 developed the TEFQ to assess eating habits in children. The validity and reliability study of the Turkish version was conducted by Demir et al.,22 from whom we obtained permission for its use. The questionnaire comprises 17 items regarding the behaviours of primary and secondary school students, which are scored on a Likert scale ranging from 4 (“definitely true”) to 1 (“definitely false”). The scale has a three-factor structure—uncontrolled eating (UE), emotional eating (EE), cognitive restraint (CR)—and the internal consistency analysis yielded a Cronbach α of 0.85. In the validity and reliability study of the Turkish version, the Cronbach α values for the dimensions were 0.85 (UE), 0.83 (EE) and 0.67 (CR). Moreover, the factor loadings of the dimensions ranged from 0.61 and 0.81. Thus, the researchers concluded that the developed scale was valid and reliable.
Intervention and data collectionData collection: the data were collected through the Google Forms platform and the trainings were delivered in person in a conference room arranged by the research team. Before collecting the data, the team obtained the authorization of the family and the assent of the child through the consent form. Children for whom we obtained both parental consent and their own assent were included in the training sessions. First, we shared the Sociodemographic Data Collection Form, CSHQ and TFEQ online with participants in training group l and in the waitlist group, requesting their completion. In the next stage, one month later, the training group received the sleep hygiene training, developed under the supervision of expert faculty members. It was delivered in person in sessions held in a conference room arranged by the research team. The training was delivered by a researcher to groups of 10 people in weekly sessions lasting 40 min for a total of four weeks, and started with a 10-minute introduction and explanation of the interview rules. Then, the researcher gave a 30-minute PowerPoint and video presentation on sleep hygiene. After the training, children received feedback in a question and answer (Q&A) format.
The training was provided to determine the effect of sleep hygiene training on sleep and diet. Sleep hygiene training topics include individual characteristics and experiences regarding sleep, previous sleep-related behaviours, sleep-related health promotion behaviour, sleep-related habits, personal factors affecting sleep, cognitive factors and influences specific to sleep behaviour; definition of sleep, importance of sleep, symptoms of sleep, causes of insomnia, sleep problems, factors that prevent sleep quality, factors that facilitate sleep quality and sleep-related behaviour outcomes; it encompasses sleep hygiene, sleep hygiene training, and health behaviour practices to improve sleep quality. The presentation was followed by a 10-minute Q&A and explanation session. Three months after completion of the training in the first phase, the families of the children who participated in the training were contacted again via social media and invited to participate in the survey, and the same data collection tools were used to re-evaluate participants in the two groups.
Ethical considerationsThe study was approved by the Hakkari University Scientific Research and Publication Ethics Board (IRB, 2023/9 0-1; date, 24/08/2023). We did not obtain or shared any personally identifiable information. We obtained the assent of the children, who participated on a voluntary basis, and the consent of the parents to the participation of the children in the study.
Statistical analysisThe statistical analysis of the data was carried out with the software SPSS, version 26.0, contingency tables to assess the distribution of the sociodemographic characteristics of the participants and the χ2 test to make comparisons. We used ANCOVA and correlation tests to compare the scores of the Three-Factor Eating Scale for Children and the Children’s Sleep Habits Questionnaire in the pretest and post-test assessments of the training group and waitlist group.
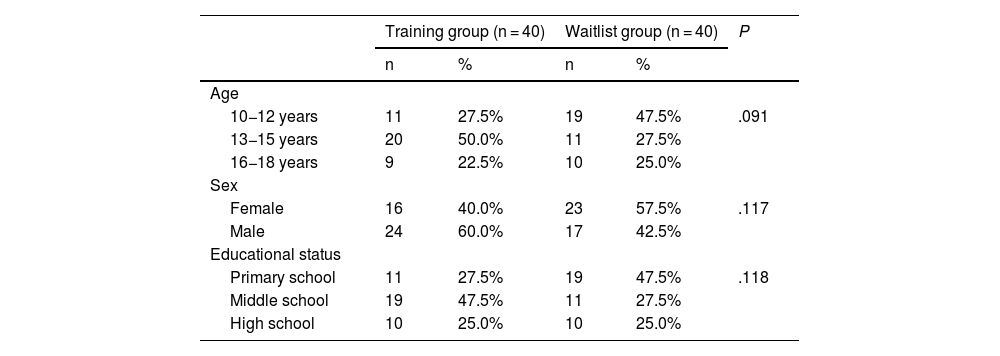
ResultsTable 1 shows the sociodemographic characteristics of participants. In the training group, the 27.5% of the children were aged 10–12 years, 50.0% 13–15 years and 22.5% 16–18 years. The sex distribution in the training group was 60.0% male and 40.0% female. Of all participants, 27.5% attended primary school, 47.5% middle school and 25.0% high school. We did not find any statistically significant differences in the age, sex or educational status distribution between the training and waitlist groups.
Sociodemographic characteristics of participants.
| Training group (n = 40) | Waitlist group (n = 40) | P | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age | |||||
| 10−12 years | 11 | 27.5% | 19 | 47.5% | .091 |
| 13−15 years | 20 | 50.0% | 11 | 27.5% | |
| 16−18 years | 9 | 22.5% | 10 | 25.0% | |
| Sex | |||||
| Female | 16 | 40.0% | 23 | 57.5% | .117 |
| Male | 24 | 60.0% | 17 | 42.5% | |
| Educational status | |||||
| Primary school | 11 | 27.5% | 19 | 47.5% | .118 |
| Middle school | 19 | 47.5% | 11 | 27.5% | |
| High school | 10 | 25.0% | 10 | 25.0% | |
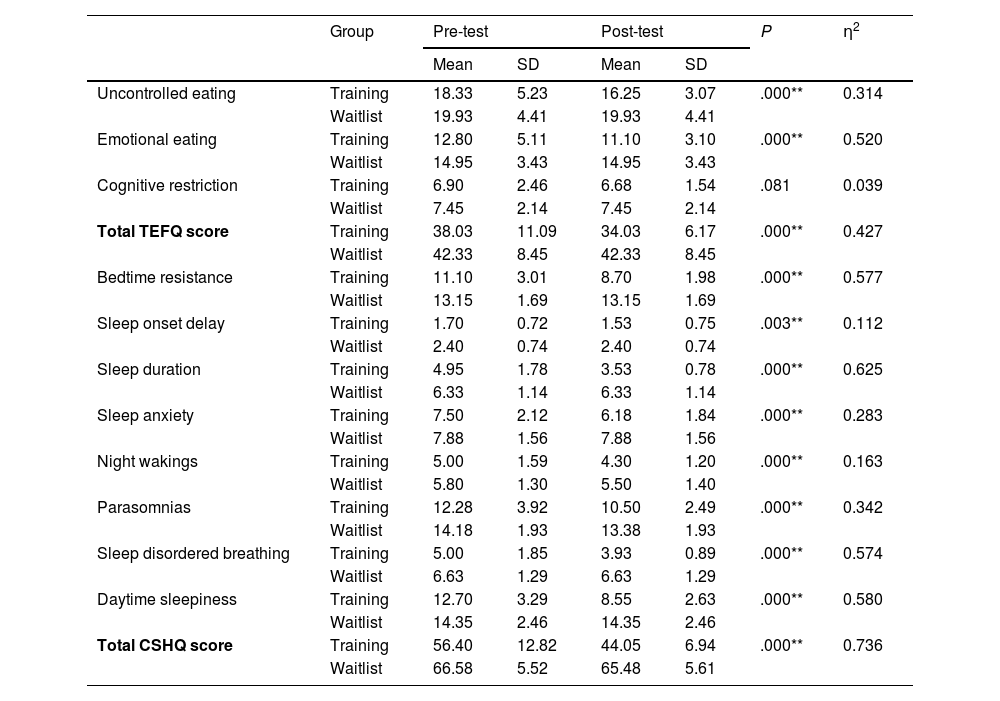
As can be seen in Table 2, we found statistically significant differences between groups in the changes in the total CSHQ, bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night wakings, parasomnias, sleep-disordered breathing, and daytime sleepiness scores (P < .001 in every comparison). We also found statistically significant differences between the training and waitlist groups in the changes in the uncontrolled eating and emotional eating dimensions of the TFEQ between the pre- and post-test assessments (P < .001 in these comparisons). However, we did not find significant differences between groups in the changes in the cognitive restraint dimension scores of the TFEQ between the pre- and post-test assessments (P = .081). There was a statistically significant difference between the training and waitlist groups in the changes in the total TFEQ score between pre- and post-test assessments (P < .005).
Comparison of Three-Factor Eating Questionnaire and Children’s Sleep Habits Questionnaire scores in the sample.
| Group | Pre-test | Post-test | P | η2 | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Uncontrolled eating | Training | 18.33 | 5.23 | 16.25 | 3.07 | .000** | 0.314 |
| Waitlist | 19.93 | 4.41 | 19.93 | 4.41 | |||
| Emotional eating | Training | 12.80 | 5.11 | 11.10 | 3.10 | .000** | 0.520 |
| Waitlist | 14.95 | 3.43 | 14.95 | 3.43 | |||
| Cognitive restriction | Training | 6.90 | 2.46 | 6.68 | 1.54 | .081 | 0.039 |
| Waitlist | 7.45 | 2.14 | 7.45 | 2.14 | |||
| Total TEFQ score | Training | 38.03 | 11.09 | 34.03 | 6.17 | .000** | 0.427 |
| Waitlist | 42.33 | 8.45 | 42.33 | 8.45 | |||
| Bedtime resistance | Training | 11.10 | 3.01 | 8.70 | 1.98 | .000** | 0.577 |
| Waitlist | 13.15 | 1.69 | 13.15 | 1.69 | |||
| Sleep onset delay | Training | 1.70 | 0.72 | 1.53 | 0.75 | .003** | 0.112 |
| Waitlist | 2.40 | 0.74 | 2.40 | 0.74 | |||
| Sleep duration | Training | 4.95 | 1.78 | 3.53 | 0.78 | .000** | 0.625 |
| Waitlist | 6.33 | 1.14 | 6.33 | 1.14 | |||
| Sleep anxiety | Training | 7.50 | 2.12 | 6.18 | 1.84 | .000** | 0.283 |
| Waitlist | 7.88 | 1.56 | 7.88 | 1.56 | |||
| Night wakings | Training | 5.00 | 1.59 | 4.30 | 1.20 | .000** | 0.163 |
| Waitlist | 5.80 | 1.30 | 5.50 | 1.40 | |||
| Parasomnias | Training | 12.28 | 3.92 | 10.50 | 2.49 | .000** | 0.342 |
| Waitlist | 14.18 | 1.93 | 13.38 | 1.93 | |||
| Sleep disordered breathing | Training | 5.00 | 1.85 | 3.93 | 0.89 | .000** | 0.574 |
| Waitlist | 6.63 | 1.29 | 6.63 | 1.29 | |||
| Daytime sleepiness | Training | 12.70 | 3.29 | 8.55 | 2.63 | .000** | 0.580 |
| Waitlist | 14.35 | 2.46 | 14.35 | 2.46 | |||
| Total CSHQ score | Training | 56.40 | 12.82 | 44.05 | 6.94 | .000** | 0.736 |
| Waitlist | 66.58 | 5.52 | 65.48 | 5.61 | |||
CSHQ, Children’s Sleep Habits Questionnaire; TFEQ, Three-Factor Eating Questionnaire.
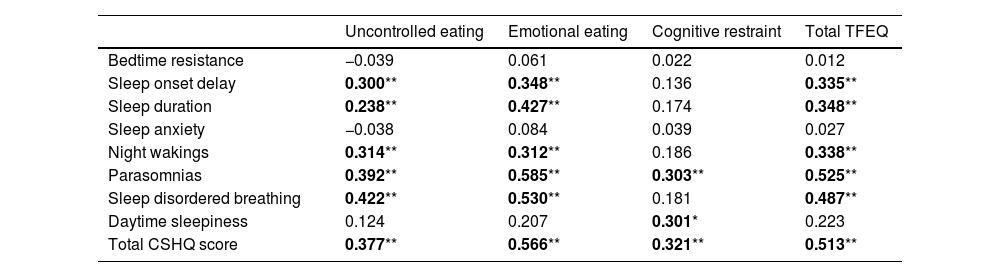
When we considered the entire sample (80 children), we found statistically significant and positive correlations between the uncontrolled eating, emotional eating, cognitive restraint and total scale scores in the TFEQ and the sleep onset delay, sleep duration, night wakings, parasomnias, daytime sleepiness, sleep-disordered breathing and total scale scores in the CSHQ (Table 3). There were statistically significant and positive correlations between the total TFEQ score and the total CSHQ score and the scores for sleep onset delay, sleep duration, night awakenings, parasomnias and sleep-disordered breathing (P < .05).
Correlation between changes in CSHQ scores and TFEQ scores in the overall sample (training and waitlist groups, N = 80).
| Uncontrolled eating | Emotional eating | Cognitive restraint | Total TFEQ | |
|---|---|---|---|---|
| Bedtime resistance | −0.039 | 0.061 | 0.022 | 0.012 |
| Sleep onset delay | 0.300** | 0.348** | 0.136 | 0.335** |
| Sleep duration | 0.238** | 0.427** | 0.174 | 0.348** |
| Sleep anxiety | −0.038 | 0.084 | 0.039 | 0.027 |
| Night wakings | 0.314** | 0.312** | 0.186 | 0.338** |
| Parasomnias | 0.392** | 0.585** | 0.303** | 0.525** |
| Sleep disordered breathing | 0.422** | 0.530** | 0.181 | 0.487** |
| Daytime sleepiness | 0.124 | 0.207 | 0.301* | 0.223 |
| Total CSHQ score | 0.377** | 0.566** | 0.321** | 0.513** |
CSHQ, Children’s Sleep Habits Questionnaire; TFEQ, Three-Factor Eating Questionnaire.
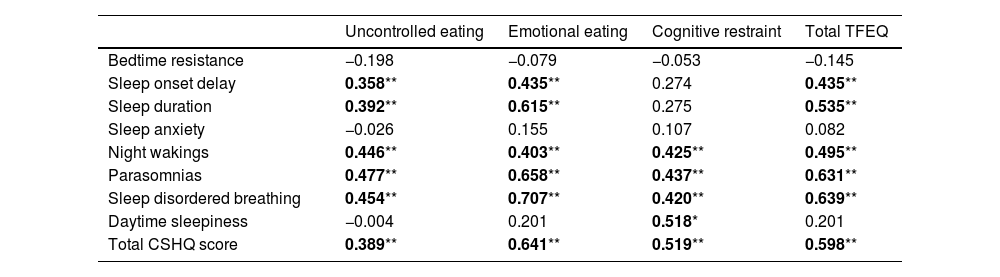
When it came to the training group (40 children), there were statistically significant and positive correlations between the uncontrolled eating, cognitive restraint and total scale scores in the TFEQ and the total scale, sleep onset delay, sleep duration, night awakenings, parasomnias, daytime sleepiness and sleep-disordered breathing scores in the CSHQ (P < .05) (Table 4). We found statistically significant and positive correlations between the total TFEQ score and the total scale, sleep onset delay, sleep duration, night awakenings, parasomnias and sleep-disordered breathing scores in the CSHQ (P < .05).
Correlation between changes in sleep problems and eating behaviours in the training group (n = 40).
| Uncontrolled eating | Emotional eating | Cognitive restraint | Total TFEQ | |
|---|---|---|---|---|
| Bedtime resistance | −0.198 | −0.079 | −0.053 | −0.145 |
| Sleep onset delay | 0.358** | 0.435** | 0.274 | 0.435** |
| Sleep duration | 0.392** | 0.615** | 0.275 | 0.535** |
| Sleep anxiety | −0.026 | 0.155 | 0.107 | 0.082 |
| Night wakings | 0.446** | 0.403** | 0.425** | 0.495** |
| Parasomnias | 0.477** | 0.658** | 0.437** | 0.631** |
| Sleep disordered breathing | 0.454** | 0.707** | 0.420** | 0.639** |
| Daytime sleepiness | −0.004 | 0.201 | 0.518* | 0.201 |
| Total CSHQ score | 0.389** | 0.641** | 0.519** | 0.598** |
CSHQ, Children’s Sleep Habits Questionnaire; TFEQ, Three-Factor Eating Questionnaire.
Based on the results, the sleep hygiene training delivered to children aged 10–18 years had positive effects on sleep and diet, and there was an association between the scores in the Three-Factor Eating Questionnaire and the Children’s Sleep Habits Questionnaire.
DiscussionBased on the results of the analysis, 27.5% of children in the training group were aged 10–12 years, 50.0% 13–15 years and 22.5% 16–18 years. Overall, there was a predominance of girls in the sample. We did not find statistically significant differences in the age, sex and educational status distributions between groups. There were statistically significant differences between the training and waiting groups in the changes in the CSHQ and TFEQ scores in the pre- and post-test assessments. In the analysis of the association between the changes in CSHQ scores and in TFEQ scores in children in the entire sample (training and waitlist groups), we found statistically significant and positive correlations between the total scale scores in the TFEQ and the CSHQ. In the analysis of the association of the changes in sleep problems and in eating behaviours in children in the training group, we found statistically significant and positive correlations between the total score in the TFEQ and the total score in the CSHQ.
Based on these findings, the sleep problems of children aged 10–18 years were associated with their eating behaviours. A study conducted by Faris et al.'s (“Eating habits are related to subjective sleep quality results in university students: findings of a cross-sectional study”, 2021)23 found an association between sleep problems and eating habits. Based on their findings in a study on sleep and eating in childhood, Burt et al.24 concluded that insufficient sleep in children is associated to their nutrition, with a negative impact. The results of a study by Gavela-Pérez et al.25 indicate that there is a relationship between sleep habits and nutrition problems.
Sleep hygiene education has positive effects on sleep quality and nutrition in children. Research shows that sleep hygiene education improves sleep quality and promotes adequate and healthy eating habits.26 Our study identified a significant difference between the scores of the two groups after training (P < .01). The working hypothesis (H1—There will be a difference between the sleep scores of children aged 10–18 years in the training group who received sleep hygiene education and the scores of children in the waitlist group who did not) was confirmed because there was a difference between the sleep scores of the training group children who received sleep hygiene training and those of children in the waitlist group. This was consistent with the findings of Corkum et al.,27 who assessed healthy sleep practices (sleep hygiene) in children with attention deficit hyperactivity disorder. Hayli and Aydin28 assessed the effect of sleep hygiene training delivered to children with intellectual disability and their mothers according to the health promotion model on sleep quality. They found improvement in sleep quality in the training group, no change in the waitlist group, and a significant difference between the average sleep scores in the two groups. Almondes and Leonardo29 investigated the study protocol of the sleep training tool for children “the perfect bedroom: learn to sleep well” and determined that children who received training in the framework of the sleep hygiene protocol slept more comfortably than children who did not receive training. Tan et al.30 studied a sleep hygiene intervention for young people aged 10–18 years with sleep problems and reported that those who received sleep hygiene education had fewer sleep problems and slept better than before. Stuttard et al.31 conducted a study in children with intellectual disability aged 5–15 years and their mothers, and determined that the children had sleep problems such as bedtime resistance or night wakings. To determine the sleep quality of children and parents, the authors used the CSHQ and a parental self-competence scale. Sleep-preventing factors were identified, and a three-month sleep hygiene training was delivered to the training group in the framework of the behavioural sleep programme to address these factors. After the intervention, the assessment of children’s sleep was repeated and found better sleep quality in children in the training group compared to children in the waitlist group. This is consistent with the findings of our study.
We found a significant difference between TFEQ scores of the children in the training and waitlist groups before and after the training (P < .01). This supported the working hypothesis (H1—there will be differences in eating behaviours between children aged 10–18 years who received sleep hygiene education versus those who did not). A similar finding was reported by Ramírez-Contreras et al.32 in their study of sleep dimensions in relation to obesity, poor diet quality and eating behaviours in school-aged children. The findings suggested that children who had adequate sleep hygiene had a balanced and regular diet, and their weight values were in the normal range for age. Albakri et al.33 conducted an umbrella review on sleep health promotion interventions and their effectiveness and found that sleep hygiene education achieved significant and effective results in terms of diet, nutrition and exercise. Zhao et al.14 reported that children who had sleep problems had a poorer diet and tended to consume more fast food. Safitra and Muharyani34 studied the relationship between sleep hygiene and sleep quality in adolescents aged 12–15 years and concluded that sleep hygiene had an impact on sleep quality as well as eating habits. Kulkarni35 investigated the impact of an intervention on parents on their sleep hygiene promoting behaviours and suggested that it had a positive impact on children in terms of both sleep hygiene and dietary habits.
The results of a sleep intervention study by Sutton et al.36 in children with developmental disabilities showed a decrease in sleep problems, an increase in sleep quality and positive changes in diet as a result of sleep assessment and education. Tapia-Serrano et al.37 reported that changes in sleep quality after an educational intervention were effective in improving diet. A study conducted by Malow et al.38 found that parent-based sleep education improved the sleep problems of children with autism spectrum disorder and had a positive impact on their eating habits.
Our study has several limitations. Although it had a prospective quasi-experimental design, One of the limitations is that the small number of children that participated due to the limited consent of families. Secondly, the inclusion of only one city on account of accessibility narrowed down the sample, which therefore is not representative of the general population. Thirdly, due to the time constraints of participants, both the data collection and training periods were short, which may have resulted in an underestimation of the association between sleep and nutrition problems.
ConclusionIn conclusion, sleep hygiene education was identified as an effective tool in sleep and nutrition management. Thus, sleep hygiene education could be included in health care and nursing interventions. We recommend training children with sleep and nutrition issues on the use of nonpharmacological methods and practices, such as sleep hygiene, in schools. We recommend performance of comprehensive studies in larger samples to assess the effects of sleep hygiene education on paediatric age groups in Turkey and other countries.
What this study adds- •
We concluded that sleep hygiene education had a significant impact on the sleep quality of children aged 10–18 years.
- •
We concluded that sleep hygiene education had a significant impact on the nutrition of children aged 10–18 years.
- •
The study provides guidance for future research.
This project did not receive any financial support. It was carried out with the resources of the researchers.