Acute appendicitis (AA) is the most frequent urgent surgical pathology in paediatrics. The COVID-19 pandemic has led to a decrease in emergency department (ED) visits, which can lead to a delay in health care and an increase in the severity of the pathologies. The objective is to analyze the rate of complicated AA during the pandemic, compared to the same period of the previous year.
Materials and methodsRetrospective unicenter observational cohort study that included patients under 14 years of age seen in the ED with a diagnosis of AA during the months of March to May 2019 (non-pandemic) and 2020 (pandemic).
Results90 patients were included (41 in non-pandemic and 49 in pandemic). No difference was found between the two periods in the time from the clinic onset until the visit to the ED (37h vs. 38h, P=.881), but there was a difference in the time from arrival at the ED until the surgery (7:00h vs. 10:30h, P=.004). The difference was accentuated when comparing the month of March with April–May 2020 (6h vs. 12h; P=.001). No significant differences were observed in the rate of complicated AA in intraoperative diagnosis (35% vs. 33%; P=.870) or anatomopathology (35% vs. 48%; P=.222), nor in the number of postoperative complications, length of hospitalization and readmissions. An increase in the anatomopathological diagnosis of AA with periapendicitis was observed (47% vs. 81%; P=.001).
ConclusionDuring the pandemic, a delay from arrival at the ED until the surgery was observed in children diagnosed with AA. This delay resulted in an increase in the diagnosis of histologically evolved AA, but without an increase in the clinical complications of the disease.
La apendicitis aguda (AA) es la patología quirúrgica urgente más frecuente en pediatría. La pandemia por la COVID-19 ha generado un descenso en las consultas a urgencias, pudiendo conllevar un retraso en la atención sanitaria y un aumento en la gravedad de las patologías. El objetivo es analizar la tasa de AA complicadas durante la pandemia, en comparación con el mismo periodo del año anterior.
Material y métodosEstudio retrospectivo observacional de cohortes unicéntrico que incluyó a pacientes menores de 14años atendidos en urgencias con diagnóstico de AA durante los meses de marzo a mayo de 2019 (no pandemia) y 2020 (pandemia).
ResultadosSe incluyeron 90 pacientes (41 en no pandemia y 49 en pandemia). No se encontraron diferencias en el tiempo desde el inicio de la clínica hasta la consulta en urgencias entre los dos periodos (37h vs. 38h, p=0,881), pero sí en el tiempo desde la llegada a urgencias hasta la intervención quirúrgica (7:00h vs. 10:30h; p=0,004). La diferencia se acentuó al comparar el mes de marzo con abril-mayo de 2020 (6h vs. 12h; p=0,001). No se observaron diferencias significativas en la tasa de AA complicadas en el diagnóstico intraoperatorio (35% vs. 33%; p=0,870) ni anatomopatológico (35% vs. 48%; p=0,222), ni tampoco en el número de complicaciones postoperatorias, duración de ingreso y reingresos. Se objetivó un aumento del diagnóstico anatomopatológico de AA con periapendicitis (47% vs. 81%; p=0,001).
ConclusiónDurante la pandemia se observó una demora desde la llegada a urgencias hasta la intervención quirúrgica en niños diagnosticados de AA. Esta demora se tradujo en un incremento del diagnóstico de AA evolucionadas histológicamente, pero sin objetivarse un aumento de las complicaciones de la enfermedad.
Acute appendicitis (AA) is the most frequent surgical emergency in the paediatric population and is the leading cause of surgical abdomen in children aged more than 2 years. It mainly affects school-aged children and adolescents, and it accounts for 8% of visits to the paediatric emergency department (PED) associated with abdominal pain.1
Acute appendicitis is a progressive disease. It starts with obstruction in the appendiceal lumen, followed by bacterial overgrowth and invasion, inflammation, ischaemia and gangrene of the wall of the appendix that can eventually progress to perforation and peritonitis.2,3 The clinical presentation is highly variable,4 although it usually has onset with epigastric abdominal pain, nausea and vomiting, followed by pain in the right iliac fossa (RIF) and fever.
Treatment consists of surgical removal of the appendix (appendectomy) by laparoscopy or laparotomy. In the early stages of disease, there is a higher probability of diagnostic tests being inconclusive and of negative appendectomy on surgical intervention. On the other hand, delayed surgery increases the risk of perforated appendicitis with peritonitis, which is associated with a significant increase in morbidity and mortality.5,6 There is ample evidence proving that perforation is directly correlated to the time elapsed between the onset of symptoms and surgical intervention.7
Coronavirus Disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a pandemic by the World Health Organization (WHO) on March 11, 2020, constituting a global public health emergency. On account of its rapid progression, in March 14, 2020 the Spanish government declared a state of alert, closing down schools and businesses and mandating the confinement of the population while restricting travel.
Children account for 1%–2% of all cases of COVID-19.8 Most experience mild manifestations such as fever, cough and cold symptoms.9,10 A smaller proportion present with gastrointestinal symptoms, such as diarrhoea or vomiting.
The pandemic has caused a 70%–80% decrease in the visits to PEDs and delays in seeking care.11,12 However, despite the confinement and social isolation, children continue to develop other diseases, some of them severe and requiring urgent medical care, such as bacterial infections, cancer, endocrine disorders or surgical diseases. Delays in care can increase the morbidity and mortality associated with these diseases, as is the case of AA, a factor that has not been taking into account in calculating the extent of the damage caused by the pandemic.13
This was the rationale to conduct a study analysing the impact of the pandemic in the clinical presentation, outcomes and complications of paediatric patients with a diagnosis of AA.
The main objective of the study was to analyze the incidence of complicated AA during the COVID-19 pandemic, comparing it to the incidence during the same period the year before.
Material and methodsWe conducted a retrospective single-centre observational cohort study that included all patients aged less than 14 years managed in the PED of a tertiary care hospital given a diagnosis of AA between March and May 2020 (pandemic), comparing these cases to data for the same period the year before (no pandemic).
Definitions- •
Complicated AA: the surgical diagnosis included perforated appendicitis, abscess, appendiceal phlegmon requiring surgery and peritonitis.14–16 The histopathological diagnosis included gangrenous AA, necrotizing AA and AA with abscess formation. In this study, we defined complicated AA based on the histopathological diagnosis.
- •
Periappendicitis: the presence of periappendicitis, or changes in periappendiceal fat and serositis in the histological examination reflect greater histological progression of AA.
- •
State of alert: exceptional state that is applicable when extraordinary and very dire circumstances (disasters, health care crises, war, etc.) make it impossible to maintain normal life with the ordinary powers of the competent authorities. The government and armed forces are given greater authority and can restrict free travel of individuals or vehicles (mandatory confinement/lockdown).
- •
Pandemic: emerging epidemic disease that spreads through a large geographical area, affecting nearly all individuals in the region.
The paediatric emergency physician made the initial diagnosis of AA based on the clinical presentation and sonographic features. Subsequently, the surgeon confirmed the suspected diagnosis and established the indication for surgery, and antibiotic prophylaxis was administered before the operation. In April and May 2020, with the aim of preventing SARS-CoV-2 transmission, the protocol called for performance of a PCR test before surgery, except in life-threatening emergencies.
All cases of AA were managed with appendectomy, restricting conservative treatment with antibiotics exclusively to cases of suspected appendiceal phlegmon based on clinical and sonographic features. Appendectomy was performed routinely according to standard protocol, in most cases through laparoscopy. During surgery, the appendicitis was classified as phlegmonous (inflamed, congested and erythematous appendix with decreased compressibility and presence of exudate), gangrenous (appendix with a greyish, purplish or greenish hue and a thin and friable wall) or perforated-complicated (macroscopic perforation, appendicolith or free fecalith, purulent peritonitis, para-appendiceal abscess or appendiceal mass).14,17,18 The Department of Pathology performed routine examinations of the surgical specimen, classifying cases of phlegmonous AA as uncomplicated, cases of phlegmonous AA with periappendicitis as progressing to complicated, and cases of gangrenous AA, necrotizing AA or AA with abscess formation as complicated.
Data collectionWe retrieved information from the electronic health records. We collected data for the following: demographic characteristics, paediatric assessment triangle (PAT), time elapsed from onset to PED visit, associated symptoms, findings of the physical examination, diagnostic tests and treatment received. We also analyzed patient outcomes in hospital and after discharge by reviewing hospital and primary care records and the histopathological report of the examination of the surgical specimen that included the definitive diagnosis.
The primary outcome was the proportion of complicated appendicitis in patients given a diagnosis of AA in the pandemic period, which we compared to the proportion in patients managed the year before.
Statistical analysisWe have expressed qualitative variables as absolute and relative frequencies. We analyzed the association between qualitative variables by means of the chi square test. We compared normally distributed quantitative variables with the Student t test. We compared nonparametric variables with the Kruskal–Wallis and Mann–Whitney U tests. The statistical analysis was performed with the software SPSS 23.0 for Windows (SPSS Inc.; Chicago, IL, USA). We defined statistical significance as a P-value of less than 0.05.
Ethical considerationsThe study was approved by the Ethics Committee of the hospital. Since we collected all the data from a database in which all patient information was anonymised and the inclusion of these data in our register did not involve any additional intervention, the study did not require obtention of informed consent.
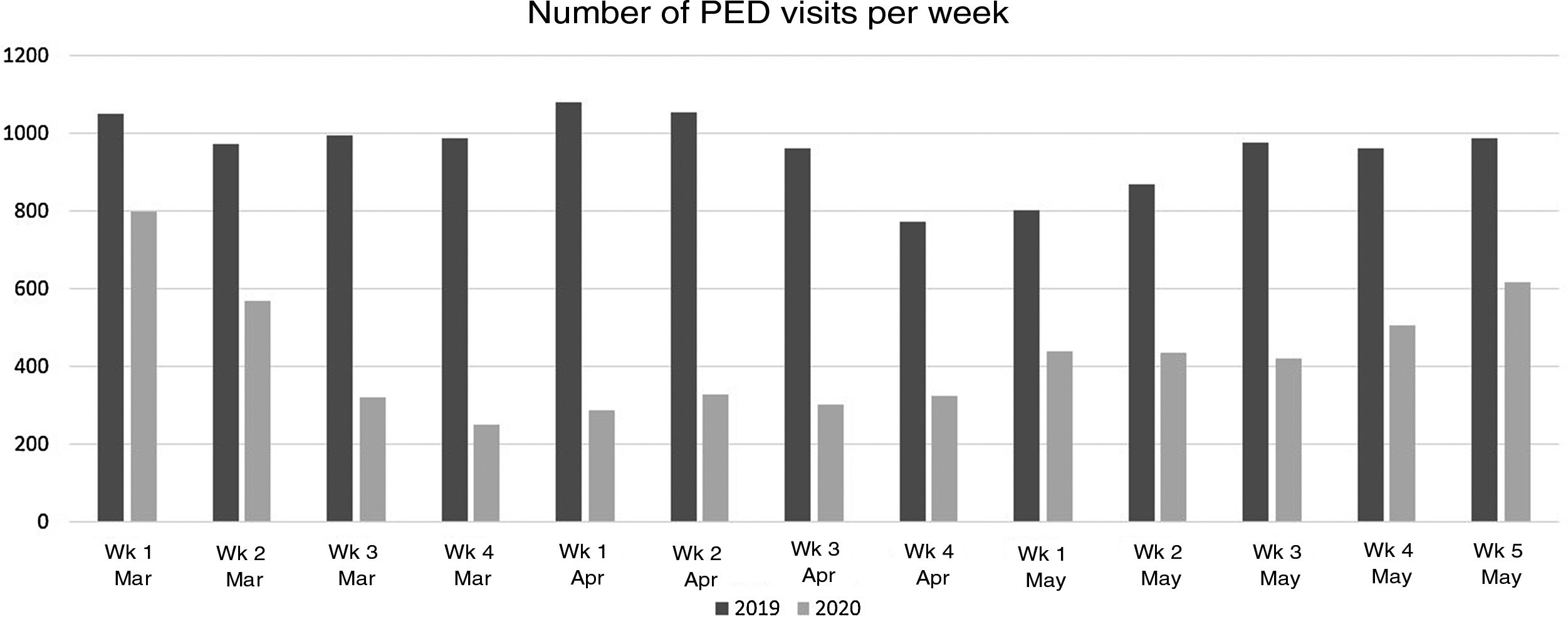
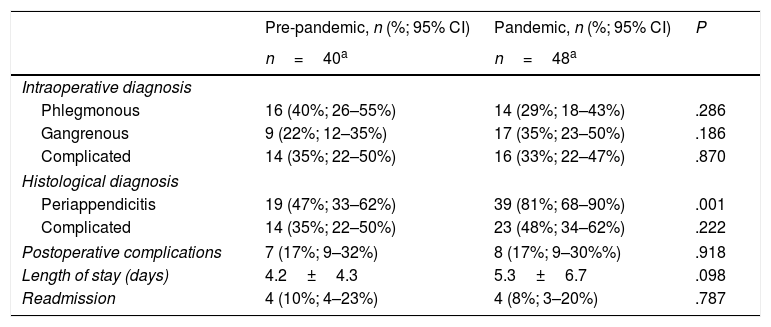
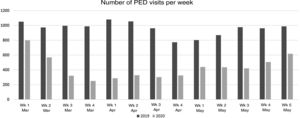
ResultsBetween March 1 and May 31, 2019, the PED managed 12 593 visits, compared to 5775 in the same period in 2020, which represented a 54% reduction in the volume of visits. Fig. 1 shows the number of visits to the PED broken down by week in both periods under study.
A total of 90 patients received a diagnosis of AA, 41 (46%) in the pre-pandemic period and 49 (54%) during the pandemic, which amounted to 0.3% and 0.8% of total visits to the PEDs in each of these periods, respectively. The mean age of the patients was 9.2 years (range, 2–13 years); 73% were male and 27% female, without differences in the distribution between study periods.
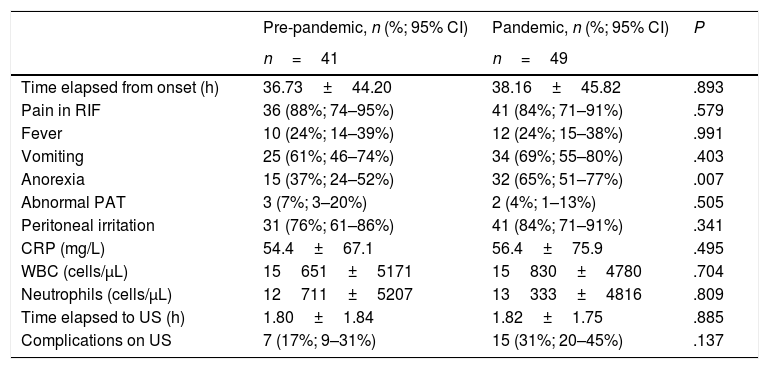
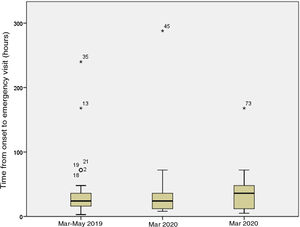
The mean time elapsed from onset of symptoms to surgical intervention was 42.75h (median, 30.50h; range, 9.00–248.00h) in the pre-pandemic period versus 48.42h (median, 40.00h, range, 11.00–301.00h) in the pandemic period (P=.936). Table 1 presents the differences in the time elapsed form onset to the PED visit, the clinical manifestations, findings of the physical examination, laboratory test results, time elapsed from arrival to the PED to performance of ultrasound and the frequency of complications detected by ultrasound in both groups. We only found a statistically significant difference in the presence of anorexia (37% vs. 65%, P=.007).
Comparison of clinical manifestations, findings of physical examination, time elapsed to ultrasound and complications in the pre-pandemic and pandemic periods.
| Pre-pandemic, n (%; 95% CI) | Pandemic, n (%; 95% CI) | P | |
|---|---|---|---|
| n=41 | n=49 | ||
| Time elapsed from onset (h) | 36.73±44.20 | 38.16±45.82 | .893 |
| Pain in RIF | 36 (88%; 74–95%) | 41 (84%; 71–91%) | .579 |
| Fever | 10 (24%; 14–39%) | 12 (24%; 15–38%) | .991 |
| Vomiting | 25 (61%; 46–74%) | 34 (69%; 55–80%) | .403 |
| Anorexia | 15 (37%; 24–52%) | 32 (65%; 51–77%) | .007 |
| Abnormal PAT | 3 (7%; 3–20%) | 2 (4%; 1–13%) | .505 |
| Peritoneal irritation | 31 (76%; 61–86%) | 41 (84%; 71–91%) | .341 |
| CRP (mg/L) | 54.4±67.1 | 56.4±75.9 | .495 |
| WBC (cells/μL) | 15651±5171 | 15830±4780 | .704 |
| Neutrophils (cells/μL) | 12711±5207 | 13333±4816 | .809 |
| Time elapsed to US (h) | 1.80±1.84 | 1.82±1.75 | .885 |
| Complications on US | 7 (17%; 9–31%) | 15 (31%; 20–45%) | .137 |
Quantitative variables expressed as mean and standard deviation.
CI, confidence interval; CRP, C-reactive protein; PAT, paediatric assessment triangle; RIF, right iliac fossa; US, ultrasound; WBC, white blood cell count.
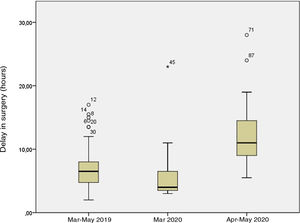
The mean time elapsed from arrival of the patient to the PED to surgical intervention was 7.00h (median, 6.30h; range, 2.00–17.00h) in the pre-pandemic period, compared to 10.30h (median, 9.30h; range, 3.00–28.00h) in the pandemic period (P=.004). Every patient received antibiotic prophylaxis before surgery, administered either at the PED or the surgical anteroom. Administration of antibiotherapy at the PED before surgery was significantly more frequent in the pandemic period (83%) compared to the pre-pandemic period (58%) (P=.008). Two patients with a sonographic diagnosis of appendiceal phlegmon, one in each period, received conservative treatment with antibiotherapy and did not undergo surgery, in adherence to the protocol for management of phlegmon.
Table 2 presents the differences in the frequency of complicated AA, postoperative complications, length of stay and readmission rate in patients that underwent surgical intervention in each period. The proportion of patients with periappendicitis, changes in periappendiceal fat or serositis was greater in the pandemic period (19% vs. 39%; P=.001).
Comparison of proportion of complicated AA, incidence of postoperative complications, length of stay and readmission rate.
| Pre-pandemic, n (%; 95% CI) | Pandemic, n (%; 95% CI) | P | |
|---|---|---|---|
| n=40a | n=48a | ||
| Intraoperative diagnosis | |||
| Phlegmonous | 16 (40%; 26–55%) | 14 (29%; 18–43%) | .286 |
| Gangrenous | 9 (22%; 12–35%) | 17 (35%; 23–50%) | .186 |
| Complicated | 14 (35%; 22–50%) | 16 (33%; 22–47%) | .870 |
| Histological diagnosis | |||
| Periappendicitis | 19 (47%; 33–62%) | 39 (81%; 68–90%) | .001 |
| Complicated | 14 (35%; 22–50%) | 23 (48%; 34–62%) | .222 |
| Postoperative complications | 7 (17%; 9–32%) | 8 (17%; 9–30%%) | .918 |
| Length of stay (days) | 4.2±4.3 | 5.3±6.7 | .098 |
| Readmission | 4 (10%; 4–23%) | 4 (8%; 3–20%) | .787 |
Quantitative variables expressed as mean and standard deviation.
AA, acute appendicitis; CI, confidence interval.
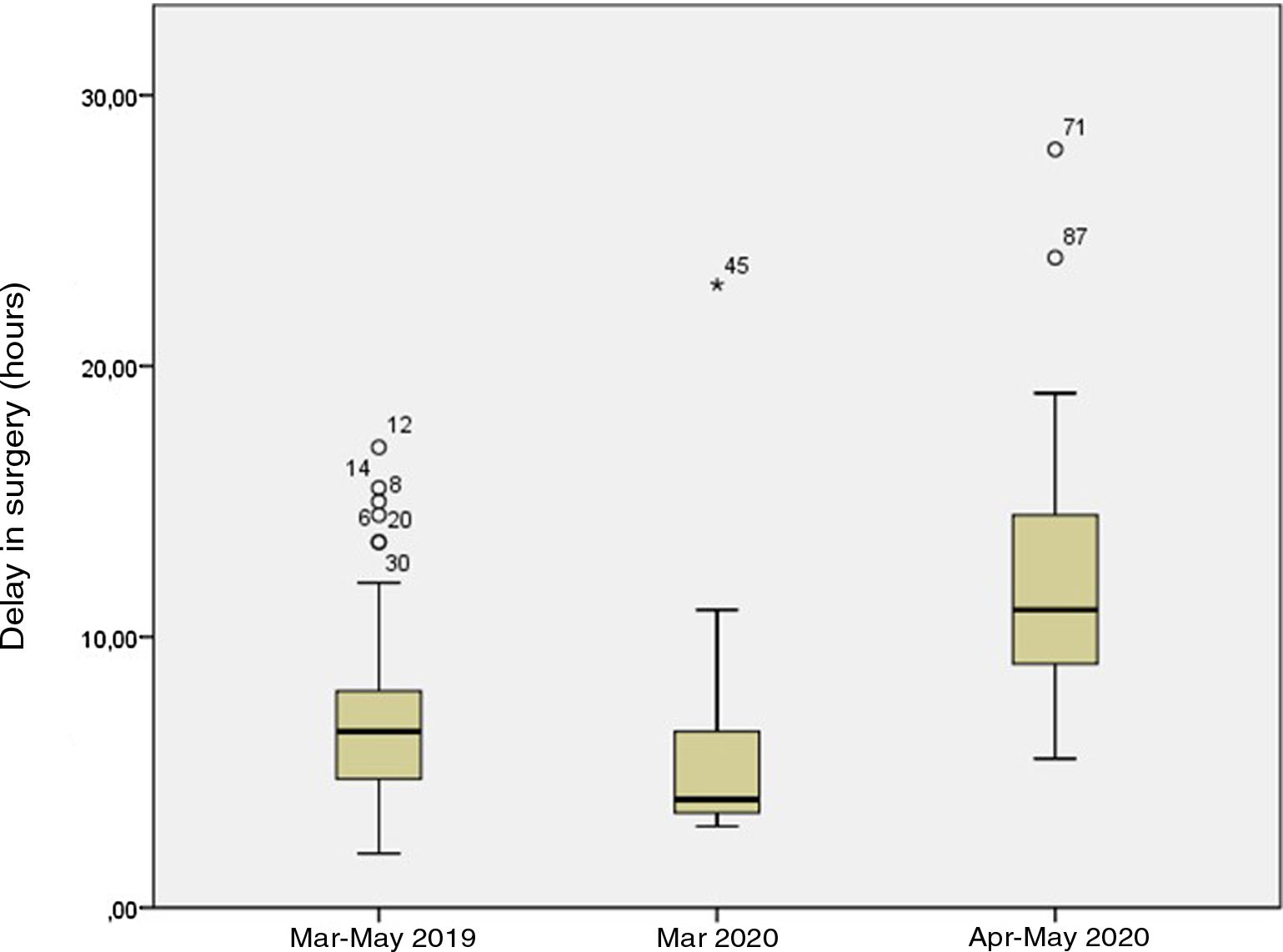
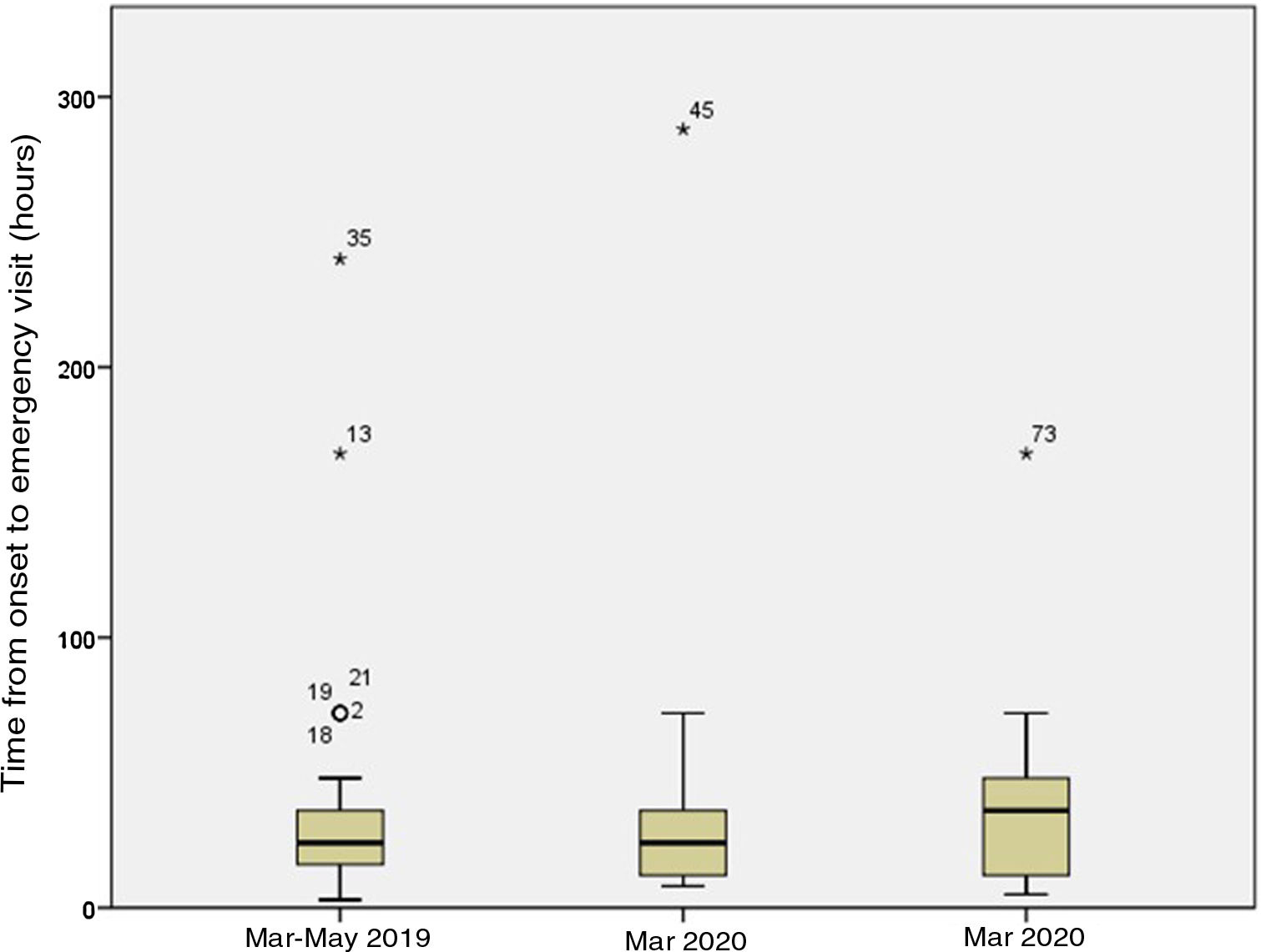
Of the 49 patients in the pandemic period, 13 (27%) were managed in March and the remaining 36 (73%) in April and May. In the latter subset, patients underwent a SARS-CoV-2 PCR test before surgery, which turned out negative in all. The mean time elapsed between onset and seeking care in the PED was 45.69h in March (median, 24.00h; range, 8.00–288.00h) versus 35.44h in April–May (median, 36.00h; range, 5.00–168.00h) (P=.072). Fig. 2 shows the time elapsed from the onset of symptoms to the PED visit, and Fig. 3 the time elapsed from arrival to the PED to surgical intervention in the 3 periods under study. The difference in the time elapsed to surgical intervention between March 2020 and April–May 2020 was statistically significant (6 vs. 12h; P=.001). We did not find statistically significant differences in the proportion of complicated AA diagnosed intraoperatively (31% vs. 34%; P=.818) or histologically (46% vs. 49%; P=.882) or in the frequency of postoperative complications (23% vs. 14%; P=.468).
Our study shows that during the first 3 months of the COVID-19 pandemic, there was an increase in the time elapsed between arrival to the PED and surgical intervention in patients with a diagnosis of AA. This delay was associated with the presence of more advanced stages of AA at the time of histological diagnosis, which did not result in a higher frequency of preoperative or postoperative complications.
Many studies have evinced a decrease in the total number of visits to PEDs, a trend that started becoming evident in February 2020 and that became more marked with the mandatory lockdowns established in different countries and the first peak of cases in the first wave of the pandemic in late March. Consistent with studies performed in Italy,11,12,19,20 the United Kingdom21 or Ireland,22 whose authors reported a 70%–80% decrease in PED visits compared to 2018 and 2019, our study found a much lower-than-normal frequency of PED visits between March and May 2020. During the pandemic, the number of visits to our PED decreased by 54%, and the decrease was most marked in the weeks that followed the declaration of the state of alert, when the number dropped to 25% of the expected volume.
This decrease in medical visits can be explained in part by the reduction in the transmission of infections and in traumatic injuries resulting from confinement.19,20 However, fear of the hospital setting, advertising campaigns that encourage staying at home and guidance by health care staff obtained through the telephone may also have contributed to delays in seeing care.12,23 These delays have led to delayed diagnosis of diseases such as diabetes mellitus, sepsis, different forms of cancer or AA.24
Despite the decrease in the total number of visits, we found a similar frequency in the diagnosis of AA, which suggests that patients with severe disease have not stopped seeking medical advice. In our hospital, cases of AA amounted to 0.3% of all visits to the PED in the pre-pandemic period and 0.8% of the total in the pandemic period. This supports previous findings in the literature describing a decrease in visits for mild complaints and an increase in the proportion of diagnostic codes considered urgent in triage.11,20
A similar study published recently25 found an increase in the time elapsed between the onset of symptoms and the diagnosis of AA during the pandemic compared to the pre-pandemic period. Our study did not identify statistically significant differences in the duration of symptoms at the time of care seeking between the 2 periods (37 vs. 38h). However, when we focused specifically on the month of March, which corresponded to the beginning of the pandemic, the exponential increase in the number of COVID-19 cases and the declaration of the state of alert, we found a delay in seeking care at the PED that was greater compared to the months that followed (46 vs. 35h), which may be explained by a greater fear of contagion in the hospital setting at the beginning of the pandemic.
Our study found an increase in the time elapsed from arrival to the PED to surgical intervention in the pandemic period compared to the pre-pandemic period (10.30 vs. 7.00h), a delay that increased in the last 2 months of the pandemic period (12 vs. 6h). This increase was due to the turnaround time of the SARS-CoV-2 PCR test, as in the first month of the pandemic period, when this test was not performed before surgery, the time elapsed to surgery was similar to the time elapsed in the pre-pandemic period (6.00 vs. 7.00h).
There is controversy regarding the clinical impact of delayed consultation at the PED. Some articles have reported an increase in mortality associated with the delayed diagnosis of diseases such as sepsis and malignancies.24 However, other authors have reported that the proportion of patients that delay seeking care that require admission to the hospital or the PICU is not significantly higher compared to patients that do not delay,23 so it does not seem as if these delays increase the frequency of complications.
When it comes to AA, a recent study by Velayos et al. found that during the pandemic, there was an increase in the proportion of complicated AA with peritonitis (32% vs. 7.3%) and of complications in general (20% vs. 9.8%) compared to before the pandemic, without significant differences in the time elapsed from onset to diagnosis (46 vs. 30h). This differs from our findings, as in our study, despite an increase in the time elapsed form onset to surgical intervention in the pandemic period, the incidence of complications was similar to the incidence the year prior. Differences in the criteria used to define complicated AA or in the delays in surgery may explain this discrepancy. In fact, the proportion of complicated AA cases in our series was higher compared to the proportion reported in the study by Velayos et al. in both periods under study. We ought to highlight that while we did not find an increase in the proportion of complicated AA, the increased delay in surgery observed in our study was associated with a significant increase in the detection of AA with periappendicitis on histological examination, which suggests a greater progression of AA at the histological level.
Whether gangrenous AA should be classified as complicated or uncomplicated based on the intraoperative findings continues to be the subject of debate.14–16 This is a macroscopic, visual diagnosis that can be subject to interrater variability. In our study, although the frequency of phlegmonous and complicated cases of AA remained stable, we found an increase in the proportion of gangrenous AA cases during the pandemic (22% vs. 35%). This highlights the usefulness of histological criteria, which not only are more objective but were able to demonstrate a greater progression of the inflammatory process at the periappendiceal level that was statistically significant. Thus, our findings suggest that delays in surgical intervention favour progression of the inflammatory process of AA at the histological level, although the observed delays were not large enough to result in clinically significant complications.
In patients with AA receive early antibiotherapy and undergo surgery within 24h of onset, the incidence of complications is lower.26–28 In our series, while we found more cases of gangrenous AA and more advanced histological progression, we did not find a higher incidence of complicated AA or intraoperative or postoperative complications, although it must be taken into account that the delay in surgical intervention never exceeded 28h.
There are several limitations to this study. First, it was conducted in a single centre and a relatively small sample, which increases the probability of biases associated with the characteristics of care delivery in our PED. However, we believe that the results can be extrapolated to other PEDs serving populations of similar sociodemographic characteristics. On the other hand, there are the limitations intrinsic to its retrospective design and obtaining data from past health records. In this regard, the fact that the documentation was produced by qualified staff and the use of prewritten notes guaranteed the quality of the health records for the purposes of our study. In addition, the comparison of the surgical diagnosis, with a known interrater variability, and the histopathological diagnosis, improved the objectivity of the findings.
In conclusion, we observed an increase in the number of cases of AA with histological progression, although we found no evidence that this was associated with an increase in the incidence of postoperative complications or in the length of stay. The increase in cases of AA presenting at more advanced stages seems to be associated with the delay in surgical intervention from the time of onset, resulting from both the initial delay in seeking emergency care and, later on, the delay in awaiting the results of the SARS-CoV-2 PCR test. Considering that the situation caused by the pandemic will continue in upcoming months, we need to ensure a high quality and safety of care in PEDs to inspire trust in the community and allow the prompt diagnosis and treatment of AA, avoiding unnecessary delays.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bonilla L, Gálvez C, Medrano L, Benito J. Impacto de la COVID-19 en la forma de presentación y evolución de la apendicitis aguda en pediatría. An Pediatr (Barc). 2021;94:245–251.