In recent years, parents have been playing an important role in the Pediatric Emergency Department (PED), and wish to be present when invasive procedures (IP) are performed.
Objectives(1) To compare the presence of parents during IP in PED in Spain between 2008 and 2012; (2) to compare the arguments to restrict the presence and problems arising from this; and (3) to determine whether the views of health personnel have changed on this subject.
MethodologyA descriptive multicenter comparative study was conducted in 2008 and 2012. A total of 42 questionnaires were sent by email to PED managers, with the responding hospitals being included in the 2 periods of the study.
ResultsA total of 22 hospitals participated in the study. The presence of parents in the PED increased between 2008 and 2012 for all IP, significantly in the blood test and urine catheterization. In 2012, managers stated that children are not so nervous, anxiety of the parents, and fear of a poorer staff performance, as an argument to restrict family presence. There were few problems during the 2 periods, with the poor behaviour of the children decreasing. According to managers, the opinion of health personnel has not changed in the last four years.
ConclusionsThe presence of parents during the IP in the PED has increased in the last four years, although the presence is low for more invasive procedures. Managers argue the presence of fewer behaviour problems to restrict family presence. The opinion of the staff has not changed in the last four years, although more studies are required on this issue.
En los últimos años los padres están adquiriendo un protagonismo cada vez mayor en los servicios de urgencias pediátricos (SUP), manifestando su deseo de presenciar los procedimientos invasivos (PI) realizados a sus hijos.
Objetivos1) Comparar la presencia de los padres durante los PI en SUP españoles entre 2008 y 2012; 2) comparar los argumentos para restringir la presencia y los problemas derivados; y. 3) conocer si ha cambiado la opinión del personal sanitario.
MetodologíaEstudio descriptivo multicéntrico comparativo. En 2008 y 2012 se envían 42 encuestas vía correo electrónico a los responsables de SUP españoles, incluyéndose en el estudio los que responden en ambos periodos.
ResultadosVeintidós hospitales participan en el estudio. La presencia de los padres en los SUP españoles aumenta entre 2008 y 2012 para todos los PI, significativamente en la analítica sanguínea y en el sondaje vesical. En 2012 los responsables argumentan menos frecuentemente el nerviosismo de los niños, la ansiedad de los padres y el temor del personal a un peor rendimiento para restringir la presencia. En ambos periodos los problemas son ocasionales, disminuyendo el peor comportamiento de los niños. Según los responsables el acuerdo del personal sanitario no ha cambiado en estos años.
ConclusionesLa presencia de los padres durante los PI en los SUP ha aumentado en los últimos 4 años, aunque es aún escasa durante los procedimientos más invasivos. Los responsables argumentan menos problemas conductuales, aunque el grado de acuerdo del personal no ha cambiado, siendo necesario continuar trabajando en el tema.
Over recent decades health care has been moving away from a paternalistic model of medicine towards one of family-centred care.1–4 This change is particularly important in the paediatric field, since children's parents and/or carers are responsible for their health and well-being. Studies carried out in the last few years on the presence of parents during invasive procedures (IPs) in paediatric emergency departments (PEDs), such as taking samples for blood tests, lumbar punctures, suturing and even cardiopulmonary resuscitation procedures (CPR), have shown that parents want to be present, and moreover many of them believe it is a right both for the child and for the parents.5–9
Health care staff, for their part, are increasingly convinced that the presence of parents can be beneficial, and some authors have drawn attention to an increase in family presence in PEDs.3,4,10
Indeed, a multicentre descriptive study2 was carried out in our department in 2008, based on questionnaires sent to the managers of various PEDs in Spain, with the main object of ascertaining whether parents were given the option of being present at various IPs. The conclusions of this study showed that family presence was still rare in Spanish PEDs and that health care staff were largely opposed to it, especially during the most invasive procedures. In 2012 it was proposed that the study be repeated, comparing the results with those obtained in 2008, with the following objectives: (1) to compare the presence of parents during IPs in Spanish PEDs in 2008 and 2012; (2) to examine the arguments for restricting family presence and the problems arising from it; and (3) to find out whether the opinion of health care staff on this subject had changed in the previous four years.
MethodsA multicentre comparative descriptive study was carried out based on questionnaires sent to the managers of Spanish PEDs affiliated to the Spanish Society of Paediatric Emergency Medicine (SEUP).
We used the same questionnaire that was sent in the study carried out in 2008. It was formulated for the first study, based on the published literature on the subject,2 and consisted of 13 multiple-response questions. In 2012 a further question was added on the managers’ perception of whether the presence of parents had increased in the previous four years. A copy of the questionnaire is included in Appendix 1.
In November 2012 the questionnaire was sent by email to the managers of the various Spanish PEDs that had taken part in the 2008 study, and two reminder emails were sent during the following three months. No remuneration was offered for completing the questionnaire; the managers who responded in both periods were included in the study.
The procedures were classified, according to their invasiveness, as low (blood sampling, intravenous (IV) line placement, bladder and gastric intubation), moderate (lumbar puncture, suturing, skeletal reduction or traction) and high (thoracentesis, endotracheal intubation and CPR).
The responses to the questionnaires received in the two periods were stored and processed in a specific Microsoft Access relational database. Quantitative and categorical variables were tabulated and analysed using the SPSS 17.0 statistical programme, applying tests to study the distribution (Kolmogorov–Smirnov test) and comparison of data, both in quantitative (Student's t test, Mann–Whitney U test) and in qualitative terms (chi-squared test, contingency table test, Fisher's exact test). P-values of less than 0.05 were considered significant.
ResultsOf the 42 managers who were sent the questionnaire, 31 replied in 2008 and 32 in 2012. A total of 22 hospitals responded in both periods. The median number of visits per year to the services surveyed was 35,000 (range 4000–115,000) in 2008 and 30,000 (range 10,000–102,000) in 2012; 3 hospitals in the sample treated fewer than 20,000 emergencies per year, 12 treated 20,001–50,000 and 6 treated more than 50,000. The median number of staff paediatricians who treated patients in the PED was 2 (range 1–4) in both periods.
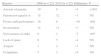
As regards the presence of parents during IPs (Table 1), in 2008 there were 8 hospitals in which they were never given the option of being present at procedures, and in 2012 all the participating hospitals gave family members the option of being present during at least one type of procedure; the difference between the two periods was statistically significant (P=.004). Comparing the presence of parents at the various IPs during the two periods, we find an increase in their presence at all procedures, and this increase was significant for blood sampling (P=.004) and bladder intubation (P=.007). No significant differences were found when the presence of parents was analysed in relation to the number of emergencies treated per year.
Presence of parents at the various invasive procedures in participating paediatric emergency services.
| Procedure | 2008 (n=22) | 2012 (n=22) | Difference | P |
| None | 8 | 0 | −8 | .004 |
| Blood sampling | 10 | 19 | +9 | .004 |
| IV line placement | 10 | 16 | +6 | NS |
| Bladder intubation | 6 | 15 | +9 | .007 |
| Oro-/nasogastric intubation | 7 | 12 | +5 | NS |
| Gastric lavage | 5 | 10 | +5 | NS |
| Lumbar puncture | 5 | 11 | +6 | NS |
| Suturing | 9 | 15 | +6 | NS |
| Fracture reduction | 3 | 7 | +4 | NS |
| Thoracentesis | 0 | 2 | +2 | NS |
| Endotracheal intubation | 0 | 2 | +2 | NS |
| PR procedures | 0 | 2 | +2 | NS |
Comparing the motives for restricting the presence of parents in the 2 periods (Table 2), behavioural reasons, such as the anxiety of the parents (P=.001) and the nervousness of the child in the second period (P=.007) were less often put forward as arguments. In 2012 the health care staff's fear of performing worse in the presence of the parents was also cited less as an argument (P=.002). No statistically significant differences were obtained for the remaining arguments for restricting parental presence, although a reduction was observed in the frequency of all of them.
Reasons for restricting parental presence during invasive procedures.
| Reason | 2008 (n=22) | 2012 (n=22) | Difference | P |
| Anxiety of parents | 19 | 8 | −8 | <.001 |
| Parents not equal to it | 15 | 12 | −3 | NS |
| Poorer staff performance | 16 | 6 | −10 | .002 |
| Invasiveness | 14 | 11 | −3 | NS |
| Nervousness of child | 8 | 1 | −7 | .007 |
| Lack of space | 9 | 5 | −4 | NS |
| Asepsis | 3 | 2 | −1 | NS |
| Complaints | 5 | 1 | −4 | NS |
As for incidents arising from the presence of parents in PEDs, the managers replied that these had occasionally occurred in both periods, but fewer problems were observed in 2012 (Table 3): there was a decrease in problems arising from bad behaviour by the child (13/22 hospitals in 2008 and 6/22 hospitals in 2012), and the difference was statistically significant (P=.022).
Fig. 1 shows the differences in the degree to which health care staff accepted family presence during IPs (according to the managers of the PEDs): their acceptance of the presence of parents at procedures whose invasiveness was considered low and moderate increased, but not to a statistically significant degree.
In 2008 one hospital in the sample had a working group on the presence of parents and another had a specific protocol. In 2012 four hospitals had a working group and five had a protocol on the subject. Finally, most of the managers in the sample (20/22) thought that a change had taken place in this area in the previous few years.
DiscussionAccording to this study, the presence of parents during IPs performed in the PEDs of the hospitals examined had increased significantly in the previous four years, and the most notable finding was that all the hospitals in the study offered parents the option of being present at some invasive procedure. No other studies analysing the frequency of parental presence during IPs in PEDs have been published up till now, and therefore we have nothing with which to compare these results. In any case, this result probably reflects a change in the model of health care, whereby parents are being given an increasingly important role.
When the results are analysed according to the IP performed, blood extraction, IV line placement, bladder intubation and suturing are currently the procedures most often witnessed by the children's parents, probably because they are the least invasive. In both periods, however, parents were not permitted to be present for the most invasive procedures (thoracentesis, orotracheal intubation and other CPR procedures), probably because they are less frequent and because of the opposition of health care staff in the case of the most invasive procedures.6,10–15
Comparing the two periods, it is now less common for managers to argue that behavioural problems arise on the part of the child and his or her family. We think this point is very important, as it reflects a change of mentality among health care staff: traditionally they have been opposed to the presence of parents, arguing that the latter are not equal to witnessing certain procedures and that children are more anxious and cry more when their parents are with them.6,10,13–16 In our view, the fact that such arguments, whose validity it has not so far been possible to demonstrate,6,10,14,16 are used less and less often is a positive development, as it implies a change of mentality among health care staff, moving away from the traditional paternalistic model of medicine.
In the same vein, the argument that health care staff perform worse when parents are present is put forward less and less frequently, according to our study. Again, it has not so far been demonstrated that this is in fact the case1,6,10,16,17; on the contrary, some authors have suggested that the more accustomed staff are to working with parents, the more comfortable they feel.17 A preliminary learning period is therefore needed in order to persuade staff.
When we compare the degree of acceptance among health care staff, as reported by the managers of PEDs, over these four years, we observe a trend towards staff being more in favour of family presence at minimally or moderately invasive procedures, and there are therefore no differences between these findings and those of other studies carried out to assess the opinion of health care staff on the subject.1,10–12
Finally, in line with the foregoing comments, most managers consider that a change had taken place in this area in the previous few years, and indeed in the PEDs in our sample the number of working groups had increased and protocols had started to be drawn up. Although the results are not statistically significant, probably due to the small sample size, the creation of multidisciplinary working groups is the first step towards increasing the presence of parents: these groups must review the published literature, analyse the views of health care staff in each hospital, create spaces for debate so that staff can express their reservations and fears, and finally formulate action protocols.3,4,18
Apart from the limitations inherent in any study based on questionnaires, the sample size in our study is small, and therefore some differences may not be significant and the results may not be representative of the population. In addition, those who responded to the questionnaires were the heads of the PEDs, and bias might have arisen from the fact that health care staff did not reply directly. Moreover, the questionnaire did not ask whether the health care staff in the hospitals were dedicated exclusively to treating paediatric patients, a point which could have influenced the results. Finally, it is likely that the heads of department who took part in our study are more interested in this subject than those who did not do so, and that the real level of family presence in PEDs is lower.
In conclusion, this study shows that the model of health care is changing in our country and that parents are playing a more prominent role: they increasingly accompany their children throughout the whole care process, although they are still rarely present during the most invasive procedures. More work therefore needs to be done to continue this process, establishing working groups in every hospital to encourage the presence of parents even at the most invasive procedures.
Conflicts of interestThe authors have no conflicts of interest to declare.
Hospitals that took part in the study: Hospital de Basurto, Hospital de Donostia, Hospital Clínico de Santiago de Compostela, Hospital Universitario de Salamanca, Hospital del Niño Jesús, Hospital Gregorio Marañón, Hospital La Paz, Hospital Príncipe de Asturias, Hospital Virgen de la Salud, Hospital Miguel Servet, Hospital Virgen del Rocío, hospital Carlos Haya, Hospital Los Arcos, Hospital Virgen de la Arrixaca, Hospital General de Castellón, Hospital de Cruces, Hospital del Mar, Hospital Arnau de Vilanova, Hospital Mútua de Terrassa, Hospital de Terrassa and Hospital Son Espases.
Please cite this article as: Angel Solà J, Sagué Bravo S, Parra Cotanda C, Trenchs Sainz de la Maza V, Luaces Cubells C. ¿Ha aumentado la presencia de los padres durante los procedimientos invasivos en urgencias en los últimos años? An Pediatr (Barc). 2015;82:6–11.
Paper given as an oral presentation at the 18th annual meeting of the Spanish Society of Paediatric Emergency Medicine, Granada, 25–27 April 2013.