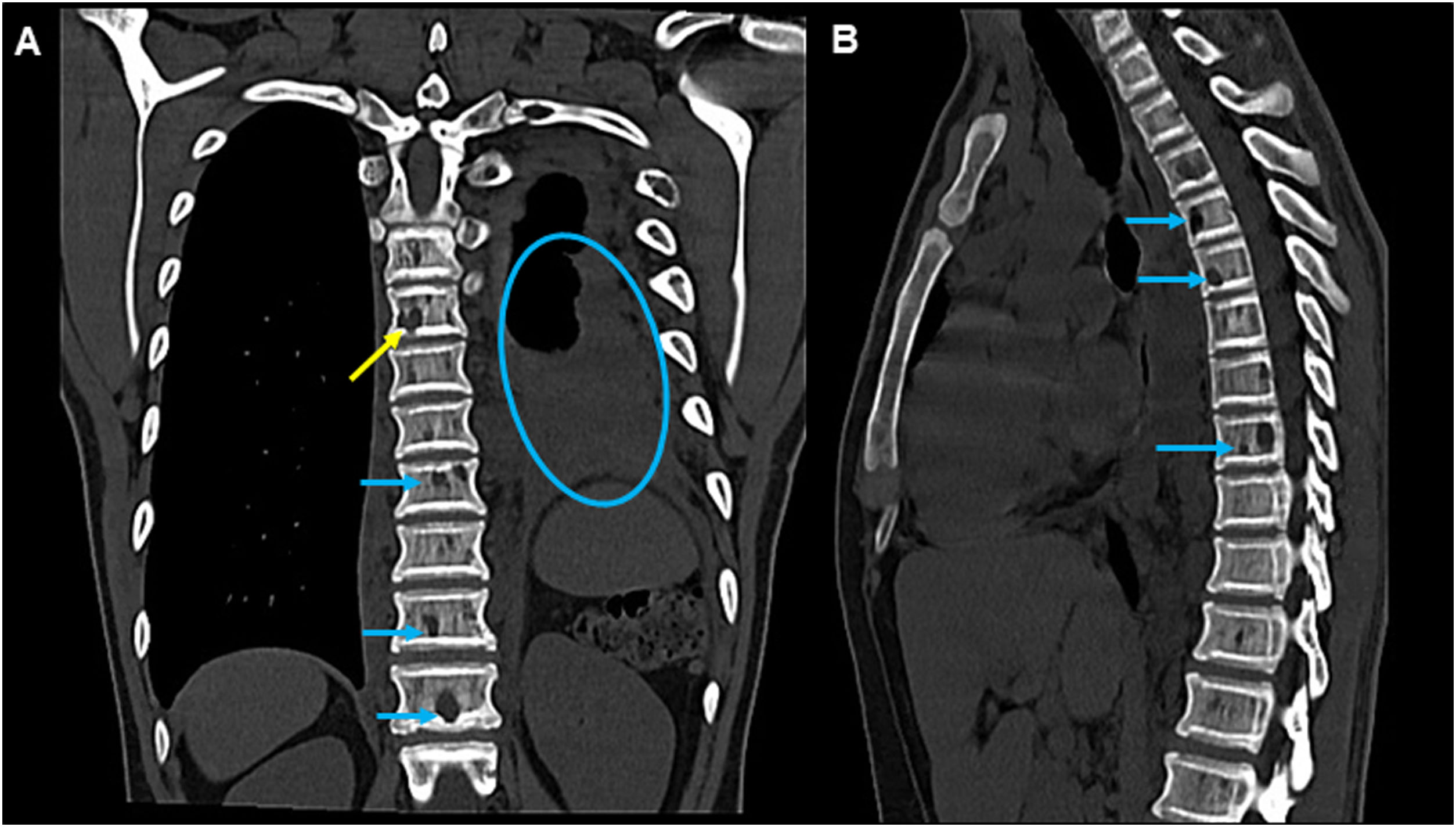
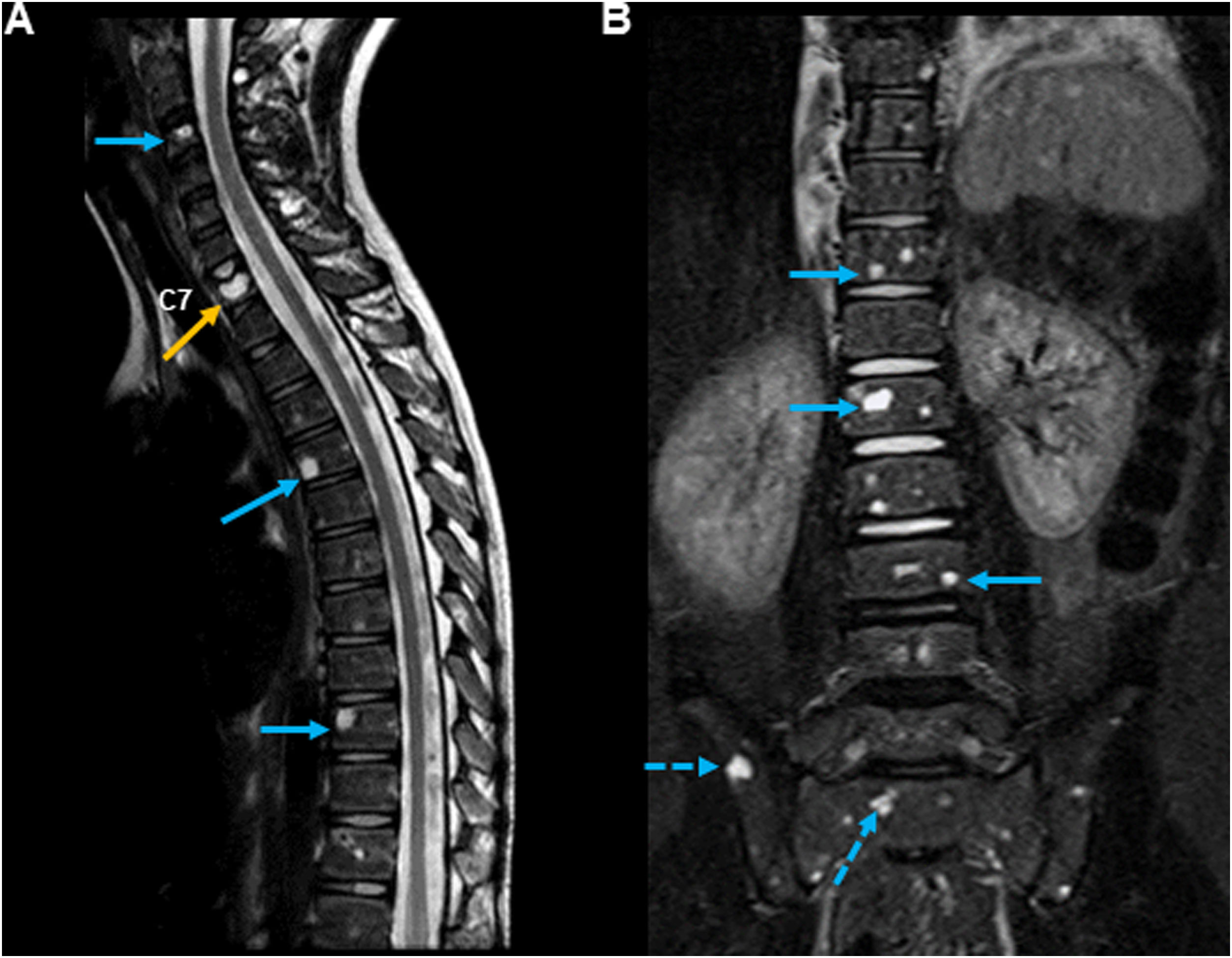
A boy aged 6 years that had experienced some episodes of dyspnoea that resolved with bronchodilators presented to the emergency department with a progressive dyspnoea, with onset 1 week prior, refractory to bronchodilators. The physical examination revealed decreased lung sounds in the left hemithorax and absence of fever. The laboratory findings were unremarkable, including no leukocytosis. A chest computed tomography scan evinced moderate pleural effusion on the left side and multiple osteolytic lesions in the spine (Fig. 1). The thoracentesis revealed chylothorax. A magnetic resonance imaging (MRI) scan confirmed diffused vertebral lesions, with fracture of C7, with involvement of the skull (Fig. 2). A positron-emission tomography scan was performed that also detected multiple osteolytic lesions involving the ribs and intercostal spaces, shoulder blades, pelvis, femurs and the foot bones. The parietal bone biopsy revealed lymphangiomatosis without increased osteoclastic activity, which was suggestive of Gorham-Stout syndrome, also known as vanishing bone disease. Other possible causes of osteolysis, such as infection, cancer, inflammatory and endocrine disorders, were excluded. The constant recurrence of the chylothorax required several surgical interventions. The patient started treatment with interferon-α-2b (1.5 million IU/m2, 3 times a week, subcutaneously) for 27 months, and chylothorax has not since recurred. At 27 weeks, a follow-up MRI scan showed a slight reduction and volume increase in different osteolytic lesions. The dose of interferon-α-2b was increased to 3 million IU/m2, with administration 3 times a week, for approximately 32 months, with no relevant side effects. From this point, the interferon-α-2b dose has been tapered, and the patient is currently in treatment with 1.5 million IU/m2/week. The follow-up MRI at 10 years evinced that the bone lesions had stabilised and absence of any other significant complications, with no impact on the patient’s daily activity. Gorham-Stout disease is a rare skeletal condition characterized by proliferation of endothelial-lined vessels (lymphangiomatosis) replacing normal bone, thereby causing osteolysis. The cause of excessive bone resorption in GSD is unclear, but it is related to local vascular/lymphatic proliferation.1,2 Chylothorax may develop due to the extension of lymphangiomatosis into the pleural cavity, affecting the thoracic skeleton, which we consider the most likely cause in this case, or by invasion of the thoracic duct. In most cases, the disease progression is slow, but clinical suspicion is important to start treatment in order to avoid complications.3
Computed tomography (CT) scan of the thoracic spine in bone window. (A) Coronal view showing moderate pleural effusion on the left side (circle) and multiple sharply demarcated lytic lesions, predominantly in vertebral bodies (blue arrows), one of them with cortical erosion (yellow arrow). (B) Sagittal view showing the same multiple sharply demarcated lytic lesions involving the vertebral bodies (arrows).
(A) Sagittal T2-weighted MRI scan of the cervical spine confirming the presence of multiple lesions involving the vertebral bodies, with hyperintense signals (blue arrows) suggestive of compression fracture at the level of C7 (orange arrow). (B) Coronal T2-STIR sequence image of the upper thoracic and lumbosacral spine revealing lesions with the same characteristics (arrows) and sacroiliac involvement (dashed arrows).