In the context of epidemiological trends in maternal obesity and type 2 diabetes, the incidence of gestational diabetes has increased significantly in recent decades, increasing the risk of foetal, neonatal and long-term complications in the offspring.1
Maternal diabetes can be classified as gestational diabetes (GD) or pregestational diabetes (PGD), with a prevalence of 7.5% (90% of pregnant women with diabetes) and 1.8% (10% of pregnant women with diabetes), respectively. Gestational diabetes is defined as diabetes first detected during pregnancy, although it could be pre-existing or persist after delivery. Pregestational diabetes includes diabetes type 1 and type 2 diagnosed before pregnancy.2
In Spain, routine screening for diabetes is recommended for all pregnant women between weeks 24 and 28 of gestation with the O’Sullivan test, with performance of a glucose tolerance test if the results are positive or in the presence of risk factors. The end of pregnancy does not differ from all other pregnancies unless diabetes is severe or poorly controlled.3
Children of mothers with GD are at increased risk of macrosomia, hypoglycaemia, jaundice, respiratory distress and hypertrophic cardiomyopathy. On the other hand, PGD is associated with an increased risk of miscarriage, intrauterine growth restriction and congenital malformations, especially if the mother has poor glycaemic control in the preconceptional period and early in the first trimester of gestation.4
Congenital anomalies amount to 50% of all perinatal morbidity, and chiefly involve the cardiovascular system, followed by the central nervous system and genitourinary system.5
We conducted a retrospective and descriptive study of neonatal morbidity in the offspring of mothers with diabetes. To this end, we reviewed health records for the period ranging from January 2017 to January 2021 to establish the incidence of neonatal illness in 2 different groups (GD and PGD). We analysed whether poor metabolic control in women with GD, defined as absence of control through dietary measures or exercise and requiring insulin. In the PGD group, we assessed whether the duration of diabetes, the presence of comorbidities and glycated haemoglobin (HbA1c) values before delivery were associated with neonatal morbidity.
Data handling started with collection of data for the variables of interest in an Excel spreadsheet that were later anonymised and transferred to an electronic database and analysed with the software SPSS version 21. We have expressed categorical data as absolute frequency and percentage distributions and compared them with the chi square test. For continuous data, we assessed the distribution with the Kolmogorov-Smirnov normality test. We expressed normally distributed data as mean and standard deviation (SD), and non-normally distributed data as median and interquartile range (IQR). We compared quantitative data in the 2 groups by means of the Student t test or Mann–Whitney U tests as applicable. For all tests, statistical significance was defined as a P-value of less than .05.
We included 161 patients managed in the period under study, 80% born to mothers with GD and 20% to mothers with PGD. The prevalence of GD in our region is 7.5%. In the GD group, 42% of women required treatment with insulin, an outcome that was not associated with the maternal body mass index (BMI).
The mean maternal age was 33.4 years, and mothers had had a median of 1 child before (IQR, 0–3). The median length of stay was 5 days (IQR, 2–11), and 41 infants required admission to the neonatal intensive care unit (NICU) for a median of 7 days (IQR, 3–12.5). Prematurity was the most frequent reason for NICU admission, followed by respiratory distress.
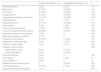
Table 1 presents the baseline characteristics and Table 2 a summary of neonatal morbidity for each group.
Baseline/prenatal characteristics by group.
| Gestational diabetes n (%) | Pregestational diabetes n (%) | P | |
|---|---|---|---|
| BMI: | |||
| <25 | 5 (25%) | 19 (61%) | .236 |
| 25–29 | 2 (10%) | 2 (25%) | |
| 30–39 | 6 (30%) | 6 (50%) | |
| ≥40 | 7 (35%) | 1 (8%) | |
| Polyhydramnios | 4 (3%) | 4 (13%) | .024 |
| Hypertension | 18 (14%) | 12 (39%) | .001 |
| Previous miscarriage | 43 (33%) | 17 (55%) | .024 |
| Delivery: | |||
| Uncomplicated | 51 (40%) | 7 (22%) | .110 |
| Instrumental | 22 (17%) | 4 (13%) | |
| Caesarean | 57 (43%) | 20 (65%) | |
| IUGR | 17 (13%) | 2 (7%) | .304 |
Analysis of neonatal morbidity by group.
| Gestational diabetes n (%) | Pregestational diabetes n (%) | P | |
|---|---|---|---|
| Shoulder dystocia | 2 (2%) | 2 (7%) | .114 |
| Macrosomia | 20 (15%) | 12 (40%) | .013 |
| Prematurity | 47 (36%) | 20 (65%) | .004 |
| Hypoglycaemia | 32 (25%) | 21 (68%) | <.001 |
| Hypoglycaemia requiring IV infusion | 14 (11%) | 15 (48%) | <.001 |
| Hypocalcaemia | 6 (5%) | 2 (7%) | .67 |
| Hyperbilirubinemia | 27 (21%) | 13 (42%) | .014 |
| Erythrocytosis | 3 (2%) | 1 (3%) | .768 |
| Hyaline membrane disease | 10 (8%) | 7 (23%) | .015 |
| Transient tachypnoea of the newborn | 34 (26%) | 8 (26%) | .968 |
| Respiratory distress due to asphyxia | 3 (2%) | 0 | .393 |
| Meconium aspiration syndrome | 1 (1%) | 0 | .624 |
| Congenital heart disease | 21 (16%) | 11 (36%) | .007 |
| Hypertrophic cardiomyopathy | 4 (3%) | 5 (16%) | .001 |
| Ventricular septal defect | 4 (3%) | 1 (3%) | .966 |
| Interatrial communication: | .029 | ||
| Patent foramen ovale | 3 (2%) | 4 (13%) | |
| Atrial septal defect | 6 (5%) | 2 (6,5%) | |
| Perinatal asphyxia | 4 (3%) | 0 | .323 |
| 5-min Apgar <7 | 5 (4%) | 1 (3%) | .87 |
| Cord blood pH <7 | 3 (2%) | 0 | .39 |
| Obstetrical brachial plexus palsy | 0 | 2 (6,5%) | .004 |
| Feeding intolerance | 20 (15%) | 6 (19%) | .589 |
| Dysraphism (neural tube defects) | 1 (1%) | 0 | .624 |
The analysis of the results showed that neonatal morbidity was more frequent in children of mothers with PGD, with a higher incidence of preterm birth, hypoglycaemia, jaundice, newborn respiratory distress syndrome, hypertrophic cardiomyopathy, macrosomia and obstetrical brachial plexus palsy.
The incidence of polyhydramnios and high blood pressure was greater in mothers with PGD, specifically in those with type 1 diabetes. We found an increased risk of macrosomia in the offspring of mothers with PGD and mothers with GD who required insulin. Neonatal morbidity in the offspring of mothers with PGD was not associated with maternal comorbidities (obesity, retinopathy, renal disease, acanthosis nigricans, high blood pressure, sudden cardiac arrest) or the treatment received during pregnancy. In mothers with PGD, the mean HbA1c concentration was 7.7 (SD, 1.19), and we found no association between this parameter and neonatal comorbidity. The mean duration of diabetes was 14 years (SD, 9.9), and the duration was significantly associated with maternal high blood pressure and neonatal hypoglycaemia, obstetrical brachial plexus palsy and congenital heart disease in the offspring.
Preterm birth, neonatal hypoglycaemia, hyperbilirubinaemia requiring phototherapy and hyaline membrane disease were more frequent in infants born to mothers with type 1 diabetes or with GD and poor glycaemic control.
The proportion of offspring with hypertrophic cardiomyopathy and congenital heart disease was greater in the subsets of mothers with type 1 diabetes and GD requiring treatment with insulin, although it is worth noting that most of congenital heart defects were uncomplicated ones, such as interatrial communication in the form of patent foramen ovale or patent ductus arteriosus. We only found one case of neural tube defect in an infant born to a mother with GD requiring insulin, and no cases of genitourinary anomalies.
In agreement with previous studies, our results lead us to conclude that neonatal morbidity is more frequent in the offspring of mothers with PGD and that poor metabolic control in GD increases the risk of neonatal adverse events.6
Thus, inadequate maternal glycaemic control before conception and during pregnancy increases the likelihood of neonatal morbidity. For this reason, we need to promote strategies for prevention of GD and also promote health in pregnant women with this condition to reduce the risk of perinatal morbidity and mortality in the offspring.
Please cite this article as: Santos Martín MT, Gómez Santos E, Torres del Pino M, Muñoz-Cobo GT, Pérez Hernández A. Diabetes gestacional y pregestacional: características perinatales y morbilidad neonatal. An Pediatr (Barc). 2022;96:158–160.