The number of late preterm births (between 34 and 36 weeks’ gestation) has been increasing in recent years and amounts to more than 70% of all preterm births. In addition to abnormal neurodevelopment, infants born late preterm are at higher risk of infection, faltering growth, respiratory problems and hospital admission and are less likely to be breastfed.1–4
The Sociedad Española de Neonatología (Spanish Society of Neonatology), in collaboration with the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics), published guidelines for the followup of late preterm infants in 2017 with the aim of minimising the impact of prematurity.2 The objective of our study was to analyse the comorbidities detected in a population of children born late preterm followed up in a primary care centre.
We conducted a retrospective descriptive study in which we included all children born late preterm between January 2007 and October 2019 followed in an urban primary care centre with a catchment population of 2844 children under 15 years as of September 2019.
Between January 2007 and October 2019 there were 1782 births registered at the primary care centre, of who 95.7% (n = 1707) were term births, 8.9% (n = 159) late preterm births and 2.5% (n = 44) preterm births before 34 weeks of gestation. In the subset of preterm births (n = 203), late preterm births amounted to 78% of the total.
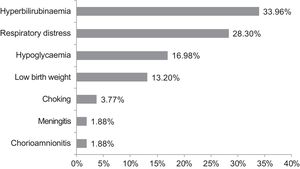
The study included 136 children (4.7% of the paediatric population served in the primary care centre during the study period). Of this total, 60.3% were male. The gestational age at birth was 34 weeks in 19.1% (n = 26), 35 weeks in 23.5% (n = 32) and 36 weeks in 57.4% (n = 78). Out of all children, 25.7% (n = 35) were not breastfed, of who 26% (n = 4) had been born at 34 weeks, 11% (n = 4) at 35 weeks and 63% (n = 22) at 36 weeks (P = .119). The mean duration of exclusive or mixed breastfeeding in the sample was 4.2 months overall (95% confidence interval [CI], 3.7–4.7; standard deviation [SD], 5.58) and 6 months after excluding participants that were not breastfed (95% CI, 5.6–6.6; SD, 5.85). Hospital admission during the neonatal period was required in 33.8% (n = 46) of participants. Of the subset of infants that required neonatal admission, 47.8% (n = 22) were born at 36 weeks’ gestation, 23.9% (n = 11) at 35 weeks and 28.2% (n = 13) at 34 weeks. Fifty percent of infants born at 34 weeks’ gestation required admission compared to 34.3% of those born at 35 weeks and 28.2% of those born at 36 weeks (P = .126). Fig. 1 presents the reasons for neonatal admission.
Nine (6.6%) children were in followup in early intervention programmes and 5 in rehabilitation (3.67%). Fifty percent (n = 7) of the children followed up through early intervention or rehabilitation services had required admission in the neonatal period.
When it came to sensory impairment, 9.55% (n = 13) had visual impairment in the form of astigmatism (n = 8), hypermetropia (n = 3), myopia (n = 2), strabismus (n = 2) and retinopathy or prematurity (n = 1). There was no evidence of impaired hearing in any of the participants.
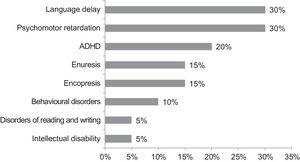
Neurodevelopmental problems were present in 15.4% (n = 21). Nineteen percent (n = 4) of these children had been born at 34 weeks of gestational age, 19% (n = 4) at 35 weeks and 62% (n = 13) at 36 weeks (P = .860). Of all patients with developmental impairment, 57% (n = 12) had required admission in the neonatal period, while 43% (n = 9) did not require it (P = .014). Of the patients that were not breastfed (n = 35), 28.5% (n = 10) had neurodevelopmental impairment compared to 10.9% (n = 11) of patients that were breastfed (n = 101) (P = .013). Fig. 2 summarises the diagnoses of children born late preterm with neurodevelopmental disorders.
In our case series, late preterm infants amounted to 78% of all infants born preterm, a proportion similar to the proportion described in the literature. Traditionally, children born late preterm were not included in the protocols for follow up of preterm infants. However, late preterm birth also entails greater vulnerability and increased morbidity, especially in the area of neurodevelopment. Several studies have highlighted that compared to children born to term, children born late preterm have a nearly 2-fold risk of experiencing neurodevelopmental impairment, with less favourable outcomes in the areas of communication, cognitive development, learning and behaviour, extending even to psychiatric disorders in adulthood or lower educational attainment.1,5 in our sample, approximately 15% of children born late preterm had some form of neurodevelopmental impairment. We ought to underscore that in this case series, only 6.6% of patients were followed up in early intervention programmes and 3.6 in rehabilitation programmes despite this being a population at higher risk of neurodevelopmental disorders. The variability in actual clinical practice, the lack of standardised criteria for referral and the long waiting lists for care such as early intervention programmes may explain the low frequency of followup in these patients, especially in those with mild neurodevelopmental impairment that may be considered as being within the normal range. In any case, the low rate of followup in early intervention and rehabilitation programmes suggests that it is necessary to ensure that health care professionals are aware of the importance of close neurologic followup in these patients.
Several studies have analysed the association between breastfeeding and cognitive development in the child.6 In our case series, nearly 30% of patients that were not breastfed had neurodevelopmental disorders compared to 10% of patients that were breastfeed, and this difference was statistically significant. We ought to highlight that in the subset of late preterm infants, 25% were not breastfed, compared to a proportion of 4.5% reported in other studies.
Knowledge of the most frequent problems in this population, promotion of breastfeeding and implementation of late preterm infant follow-up programmes are crucial to ensure early diagnosis and intervention and therefore to minimise the potential sequelae.
Please cite this article as: Andrés MM, Fernández LS, Hernández MIM, Velillas JJL. Estudio de seguimiento del prematuro tardío en un centro de atención primaria. ¿Cuál es la realidad de esta población? An Pediatr (Barc). 2021;95:49–51.