Physical activity (PA) and exercise improve the overall quality of life, as well as prevent the onset of diseases in healthy children and adolescents, and is an aid to treat prevalent chronic diseases in childhood. PA and exercise are like medicine, while sedentary lifestyle and inactivity cause disease. In this article, the existing scientific evidence in this field is reviewed and recommendations for professionals involved in child health are updated. A good knowledge of how to prescribe exercise and PA in paediatrics in different diseases is necessary. Interventions to avoid inactivity of children and adolescents must be supported by the appropriate increase in the level of PA, through integration and training programs, which achieve both an overall improvement of the neuromuscular physical condition and also physical, cognitive, and psychosocial performance. The Health Promotion Committee of Spanish Paediatric Association proposes strategies that help to obtain this objective, aiming to improve the health of our patients through the practice of exercise and the increase in PA.
La actividad física (AF) y el ejercicio físico (EF) mejoran la calidad de vida global, previenen la aparición de enfermedades en niños y adolescentes sanos, y sirve para el tratamiento de enfermedades crónicas prevalentes en la infancia. Si la AF y el EF son medicina, el sedentarismo y la inactividad provocan enfermedad. Se revisa en este artículo la evidencia científica existente al respecto y se ponen al día las recomendaciones para los profesionales involucrados en la salud del niño, ya que es necesario un buen conocimiento de cómo prescribir EF y AF en pediatría en diferentes patologías. Las intervenciones para evitar la inactividad del niño y del adolescente deben estar sustentadas en el apropiado aumento del nivel de AF, mediante programas de integración y capacitación, que consigan una mejora conjunta de la condición física neuromuscular y del rendimiento físico, cognitivo y psicosocial. La AEP, a través del Comité de Promoción de la Salud, propone estrategias que faciliten este objetivo para mejorar la salud de nuestros pacientes a través de la práctica de EF y el aumento de la AF.
Physical activity (PA) improves overall quality of life and prevents the development of diseases in healthy children and adolescents, and it is an unquestionable tool in the management of prevalent chronic diseases of childhood (Table 1). In this article, we review the scientific evidence that is currently available on the subject and update recommendations for paediatric health care providers for its integration in the multidisciplinary management of diseases, including some diseases in which rest was traditionally recommended. In this regard, the World Health Organization (WHO) and the American College of Sports Medicine (ACSM) have established guidelines on how to improve health through PA with initiatives such as Exercise is medicine,1 in which the Asociación Española de Pediatría (Spanish Association of Pediatrics, AEP) has collaborated. The integration of PA in everyday life improves the physical condition of the child as well as bone and cardiovascular health, the risk of obesity, academic performance and mood. For all the above reasons, PA is an essential tool for the prevention of disease in childhood and adolescence and later in life.2,3
Health benefits of physical activity.
| Body composition, fat mass and bone health |
|---|
| - Increased daily energy expenditure- Improved fitness: improved agility, sharper reflexes, increased speed and greater endurance |
| - Modulates the production of hormones and the regulation of hunger.- Increases muscle mass. Hypertrophy, increased oxygen consumption.- Decrease in fat mass and the risk of obesity, useful in both the prevention and treatment of obesity. |
| - Lowered risk of comorbidities associated with obesity.- Increase in bone mass and bone mineral density, decreasing the risk of osteoporosis |
| Cardiovascular risk- Improvements in cardiorespiratory fitness and metabolism.- Improvements in atherogenic lipid profile (increase in HDL cholesterol levels and decrease in triglyceride levels).- Decreased insulin resistance (prevents diabetes and decreases insulin requirements in diabetic individuals). |
| Mental health and attitude towards life- Protects from the adverse effects of sedentary behaviours.- Boosts self-esteem and mood (reduces anxiety and depression).- Improves social integration. (Promotes compliance with rules, valuing and engaging in teamwork, integrating and taking on responsibilities, and reduces the tendency to develop aggressive traits).- Improves the management of the underlying disease.- Boosts academic performance.- Can contribute to the prevention of smoking initiation in children and adolescents. |
| Improves aspects of health and contributes to clinical improvement in patients with the following:- Motor impairment.- Disorders with hypotonia.- Diseases with cardiorespiratory involvement.- Asthma.- Cancer.- Depression.- Other |
The WHO has identified sedentary lifestyles as a serious health problem in children and adolescents aged 5–17 years, with an impact comparable to the impact of other risk factors such as high blood pressure, smoking or obesity.4 In adults, physical inactivity is one of the most important preventable causes of death.5 According to the ANIBES study on sedentary habits in Spanish children and adolescents, published in 2016, 48.4% of all participants aged 9–17 years spent more than 2 h a day in front of a screen, and 84.0% had more than 2 h of screen time a day during weekends. Childhood and adolescence are stages that offer the opportunity to establish health-promoting habits, so it is of the essence that we develop strategies for the promotion of PA from an early age.
General recommendations for physical activity in children and adolescentsRecommendations for PA should be adapted based on the level of fitness, age and sex while taking into account sociocultural determinants and individual preferences. In this regard, the Committee on Physical Activity of the AEP has developed useful and specific recommendations6 (Table 2). In addition to institutional initiatives, parents and educators should contribute by delivering specific and realistic messages to achieve a clear improvement in community-based health through the promotion of exercise and PA.
Summary of the recommendations of the Committee on Physical Activity of the Asociación Española de Pediatría for the population aged 5–17 years.
| 1. Performance of moderatea to vigorousb PA for a minimum of 60 minutes per day, which can be distributed in 2 or more sessions, mostly aerobic activity, alternating with vigorous activity to promote muscle strength and bone health 3 times a week. Physical activity for more than 60 minutes may offer additional health benefits. |
|---|
| 2. Avoid sedentary behaviours. Any activity of daily living is preferable to being sedentary: walking when going to places, riding a bicycle, climbing stairs, etc. Limit to a minimum the time the child or adolescent spends watching television or with any other electronic devices. |
| 3. Group activities that are fun, conducted outdoors and offer positive reinforcement are preferable in order to integrate PA as a ‘fun and healthy daily habit’. Extracurricular activities can be very good options to this end. |
| 4. The physical setting where PA takes place should be appropriate and hazard-free, adhering to the basic safety regulations that apply to the practice of any sport. |
| 5. Physical activity is recommended for everyone regardless of health condition. Regular PA has proven to offer countless benefits when adapted to individual situations or diseases, improving the general health status. |
| 6. The practice of sports and PA as a family reinforces good habits in the child or adolescent. Parents must be role models, planning family activities in which they participate. |
| 7. Adequate nutrition and hydration improve and complement the benefits of exercise. |
These recommendations are based on those published by the WHO in 20107 and endorsed by the physical activity guidelines of the Department of Health and Human Services of the United States, which were published recently.8 The latter are even more emphatic in the need to perform PA at a moderate to vigorous level of intensity to obtain health benefits. However, despite ongoing efforts to promote PA, the PASOS study conducted in Spain in 2019 found that 63.6% of children and adolescents did not engage in the 60 min of moderate to vigorous PA every day of the week. A higher percentage of girls did not adhere to the recommendations of the WHO (70.4%) compared to boys (56.3%).9
The importance of promoting PA from an early age with the aim of educating children “from day 1” is clear in the latest guidelines on PA in children aged 0–5 years of the WHO, published in 2019. According to these guidelines, infants should be physically active several times a day by engaging in interactive floor play and should not be restrained in prams/strollers, high chairs or baby carriers for more than 1 h at a time. Those not yet mobile should spend at least half hour a day in the prone position while awake. From age 1 year, they recommend that children engage in at least 180 min of PA a day, and from age 3 years in at least 1 h of moderate to vigorous PA, for instance, by playing games involving running or jumping.10
Obesity and cardiovascular riskThe prevalence of childhood overweight and obesity in Spain seems to be reaching a plateau, but the prevalence of obesity in children is still as high as 18.1% (20.4% in boys and 15.8% in girls).11 Excess body fat in children and adolescents increases the risk of comorbidities such as high blood pressure, dyslipidaemia, insulin resistance and disorders of glucose metabolism, non-alcoholic fatty liver disease, hyperuricemia, reduced fitness and sleep apnoea.12 All of these are cardiovascular risk factors associated with cardiovascular disease in adulthood.13 One of the main contributors to this situation is the substantial decrease in the level of PA in children and adolescents.
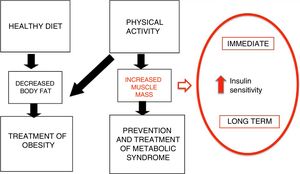
Where inactivity is the cause of disease, PA is the cure for two reasons.14 On one hand, it increases energy expenditure, which allows reducing body fat stores. On the other, PA can improve metabolic status, increasing the sensitivity to insulin in the short and the long term, and increasing muscle mass, which has a beneficial effect on cardiovascular health and fitness (Fig. 1). These benefits have been demonstrated by multiple cross-sectional studies, cohort studies and clinical trials, which we summarise in Table 3.2,15
Mechanisms of PA in the prevention and treatment of obesity (adapted from Brambillia et al14).
Association between the practice of PA and cardiovascular risk factors (adapted from I. Janssen2).
| Health outcome | Sample | Effect | Amount of PA required for health benefit |
|---|---|---|---|
| Adiposity | Overweight, obese | + | F: 3–5 d/wk I: moderate to vigorousD: 30−40 min/d T: variety of aerobic activities |
| Cardiovascular | |||
| Metabolic syndrome | Overweight, obese | + | Unclear |
| Lipids | |||
| Total cholesterol | 0 | Unclear | |
| LDL-cholesterol | 0 | Unclear | |
| HDL-cholesterol | + | Unclear (probably similar to adiposity) | |
| Triglycerides | + | Unclear (probably similar to adiposity) | |
| Blood pressure | Normotensive | 0 | Unclear |
| Hypertensive | + | F: 12–32 wk, 3 d/wk I: intensity to improve aerobic fitnessD: 30 min/session T: aerobic exercise |
+, positive effect; 0, undetermined effect; D, duration; F, frequency, I, intensity; PA, physical activity; T, type.
In the case of children and adolescents with obesity, the general recommendations apply, always taking into account the potential limitations of these patients due to their decreased fitness. Metabolic risk can be reduced considerably with a progressive increase in the level of PA, especially in inactive children.7,8 At the beginning, activities with a high impact on the joints, such as running, are not recommended, and brisk walking is considered one of the most suitable physical activities for obese children and adolescents.15,16
Bone healthOsteoporosis is one of the most frequent disorders in the elderly, and its origins can be traced to childhood. Bone mass is developed progressively during growth and depends on adequate nutrition and mechanical stimuli. With the onset of puberty, in addition to the increase in height, there is a rapid accrual of bone mineral content (BMC) that peaks following the maximum peak of height gain.17 In the 4 years surrounding this peak of maximum bone mineral accrual, individuals acquire 39% of the total BMC, and by the end of the following 4 years (until approximately age 20), individuals have accrued 95% of the total bone mass they will have as adults.18 From this moment, the bone mass percentile tends to remain constant throughout life.19 Therefore, a low BMC and bone mineral density (BMD) in adolescence would increase the risk of developing osteopenia early on and osteoporosis in adulthood, leading to an increased risk of fracture.20
The decreased intake of milk and dairy products combined with the increased intake of sugary drinks, which have a low content of calcium and a high content of phosphates, cause hypovitaminosis D. Other factors, such as the high prevalence of overweight and obesity and the use/abuse of sunscreen and the decrease in PA make the paediatric population a high-risk group. It is important to identify children and adolescents with low BMC and BMD to implement interventions for improving bone mass, making dietary/metabolic changes and proposing osteogenic exercises and sports in which bone benefits from the impact of the body weight and the action of gravity, such as running and jumping.15
Aspects related to brain health and academic performanceThe practice of sports can yield significant physical, psychological and social benefits to human individuals, and is an essential part of the well-rounded education of a person.21 There is an age-old belief that sports develop character. The practice of sports fosters the emergence of positive traits such as loyalty, cooperation, bravery, resolve, endurance, perseverance or determination, and therefore it is extremely important in education and training. Sports should not be considered a mere spectacle in pursuit of excellence and winning, but a framework for education, contact with nature, health promotion, stress relief, the discovery of new sensations and adventures, enjoyment and social interaction. The practice of sports increases self-esteem and improves academic performance and quality of life.22,23
In addition, intense PA increases the concentration of neurotransmitters that modulate cognitive processes such as memory consolidation.24 The level of fitness is positively correlated with academic achievement and intelligence, and some studies have even demonstrated a correlation between the level of fitness and performance in specific areas such as mathematics or reading. Thus, there is ample evidence supporting the recommendation of PA, and more specifically of aerobic-cardiovascular endurance PA, to optimise academic performance in children.25,26
Bronchial asthmaBy improving fitness, PA is associated with cardiorespiratory health in children and adolescents.
Asthma is the most common chronic respiratory disorder, with a current prevalence in Spain of 10% that has exhibited an increasing trend in recent years. There is solid scientific evidence that the practice of PA reduces the frequency and severity of asthma exacerbations. Thus, given that the aim of asthma treatment is for the child or adolescent to be able to live a normal life, the performance of PA or even competitive sports can positively contribute to the management of asthma.27 In these individuals, sports involving continuous activity, such as athletics, soccer, basketball etc, trigger exacerbations more often, whereas sports involving sequential activity, such as badminton, tennis, judo or swimming, are less likely to trigger exacerbations. Nevertheless, children and adolescents ought to pick the PA or sport of their preference, and physicians should adjust treatment to make their practice possible. In any case, recommendations on PA in this group should be individualised.
To prevent attacks, preventive measures should be taken for the practice of PA, such as not engaging in sports or exercise during an ongoing asthma exacerbation, practicing sports in warm and humid environments, warming up before exercise and gradually increasing the intensity of exercise. Children and adolescents need to know/learn how to breathe, using the nose and mouth appropriately, and keep their nostrils clear. If a child or adolescent experiences symptoms relatively frequently, pharmacological treatment should be prescribed and given daily or before PA.
If an exacerbation occurs during PA, the patient should stop the activity. In many cases, this is the only action that will resolve the attack, and the activity can be resumed later. If this is not the case, the patient must follow the indications of the paediatrician for the management of exacerbations. The child or adolescent should be watched an accompanied throughout the activity.28
The benefits of PA and adherence to these recommendations, even in individuals with exercise-induced asthma, amply exceed any potential risks. In addition, these risks are considerably reduced if the duration and the intensity of PA are increased gradually. Children and adolescents should be properly identified, and parents ought to inform teachers and coaches about the medication that they may need, which they should carry at all times in case it is ever needed.29
CancerDue to the relatively high survival in paediatric cancers, the care of these patients has been increasingly focusing on minimising the adverse effects of chemotherapy and radiation in survivors, and also in the prevention secondary malignancies. The long-term survival of children and adolescents that receive a cancer diagnosis exceeds 75%. However, approximately 60% of these patients will suffer chronic health problems for decades after completing treatment. Cancer treatments are associated with a broad spectrum of side effects and relapses. The course of disease and the high survival require that efforts be made to improve the quality of life of these patients.
One of the consequences of treatment is, on one hand, the low level of PA characteristic of paediatric patients30 and, on the other, their reduced cardiorespiratory fitness and muscle strength compared to healthy controls, factors that explain why children with cancer get fatigued easily, which impairs their ability to carry out daily activities and therefore their quality of life. The overprotective attitude frequently exhibited by the parents or guardians of these children further complicates this situation.30
Exercise can reduce the side effects of treatment due to its beneficial effects on the central nervous system, cardiorespiratory fitness, skeletal muscle, immune system and inflammatory and oxidative processes. Thus, regular exercise improves the capacity to carry out everyday activities more easily and effectively. In the past, physicians advised cancer patients to avoid an excess of activity before and after treatment, which was particularly deleterious to children, as PA in this population is essential for a healthy and balanced development in addition to its physical, psychological and social benefits.
In recent years, research has proven that therapeutic exercise programmes are safe for paediatric cancer patients during and after treatment, and there is solid evidence confirming the improvements achieved in cardiorespiratory fitness and muscle strength. However, these programmes have mainly targeted children with blood cancers and there is a lack of evidence on exercise interventions in patients with solid tumours, who receive more aggressive treatments that therefore have a greater impact on the child’s body. Regular moderate exercise may improve immune function (increase in the number and functionality of NK cells, the dendritic cell count or the levels of anti-inflammatory cytokines).
On the other hand, this type of nonpharmacological intervention significantly improves 2 key indicators of general health status in children with cancer (cardiorespiratory fitness and muscle strength) while having no adverse effects. Exercise can attenuate the devastating effects of treatment (especially chemotherapy) and improve the well-being of children with cancer. Regular PA (such as walking at a brisk pace for at least 30 min most days of the week) counteracts the effects of anticancer therapy.31 Of the diverse studies that have analysed exercise interventions in children with cancer, those that found the greatest benefits were those with individualised and supervised exercise programmes, conducted in the hospital setting, and that combined endurance and strength training. In addition, the beneficial effects remained at least partially for a few months after the intervention ended.32,33 In contrast, exercise programmes that involved PA that was unsupervised or conducted outside the hospital (usually in the home) have proven less effective.34,35
Physical and/or psychological disabilityExercise and PA are essential for the integral development of individuals with physical or psychological impairment. The health benefits of PA are even more important in populations with special characteristics, such as individuals with disabilities. Most individuals with disabilities can benefit from exercise, adapting the intervention to the personal circumstances of each patient.36
Disability is often associated with reduced movement. Overprotection, fear or ignorance can turn disabled individuals into inactive individiuals.37 This lack of muscular activity results in a reduction in function that is not justified by the disability. Ultimately, the functional impairment caused by the lack of activity worsens the clinical condition of the individual by adding excess weight, high blood pressure or diabetes to the underlying disability. This vicious cycle must be broken by offering exercise interventions that are inclusive of and adapted to this subset of the population.
The level of fitness and body composition of individuals with disability is poorer compared to healthy peers on account of a lower cardiorespiratory endurance and muscle strength, a higher body fat percentage, a smaller muscle mass and a reduced bone mass and density. These findings are relevant due to association between these physical fitness variables and the ability to carry out everyday tasks and activities autonomously, in addition to an increased risk of more serious problems such as stroke, sarcopenia or osteoporosis.
Children with disabilities should be given recommendations for performing the sport or type of PA best suited to their individual characteristics. This intervention is essential to promote independent living, a satisfactory life and fulfilling social interactions. Water-based activities, not limited to swimming, are the most interesting options in individuals with disability, as they offer multiple benefits (weightlessness, temperature, etc) and are easy to adapt to the individual characteristics of each person based on their disability.38
Exercise and PA in general have proven to have beneficial effects on a broad range of health-related variables in individuals with disabilities,38 including balance, muscle strength, aerobic endurance and body weight, improving muscle mass and bone health. Adapting exercise plans to the individual characteristics and goals of patients with disabilities are the key to the success of these interventions, which must be of an inclusive nature and conducted in settings close to the social and family environment.
Paediatric inactivity triadThe paediatric inactivity triad (PIT) is a novel concept proposed to assess inactivity in its 3 components: exercise deficit disorder, paediatric dynapenia and physical illiteracy.39 These 3 components are different and important in and of themselves, but they are interrelated and ought to be assessed as a whole, especially for the purpose of addressing inactivity in the context of any of the disorders mentioned in this article.
The first component of the PIT refers to levels of moderate-to-vigorous PA that do not meet current public health recommendations, thus posing a risk to health, and should be treated with the same determination as other risk factors like high blood pressure or smoking. The second and third components of the PIT help identify the other 2 conditions that influence and are in turn influenced by exercise deficit. Paediatric dynapenia refers to low levels of muscle strength and power that are not caused by neuromuscular disease, in addition to the associated functional limitations. Children and adolescents with dynapenia are more likely to be inactive, have functional impairment and become injured during PA. It is important to identify these individuals at risk and develop specific interventions to improve muscular fitness and establish PA habits that will improve strength, thus making it possible for them to achieve the levels of PA of fitter peers.39 The third component of PIT, physical illiteracy, refers to the lack of confidence, competence, motivation and knowledge required to move proficiently. This encompasses a constellation of negative factors that lead to exercise deficiency and paediatric dynapenia involving psychomotor, cognitive and affective domains of learning. Thus, interventions to improve the third component of the PIT need to be reinforced with effective pedagogical, motivational, and social strategies so inactive youth can learn the value of physical activity.
Treatment strategies that address isolated components of the PIT are less likely to achieve the desired results. The goal of intervention should be to increase the level of PA through integrative exercise programmes with physical and cognitive training, which are more likely to improve the neuromuscular fitness and physical, cognitive and psychosocial outcomes of the child.40
Final commentsBased on the body of evidence, we may conclude that PA is medicine, and that sedentary behaviours and inactivity cause disease. Therefore, paediatric health care providers must have the necessary knowledge to prescribe physical activity and promote its practice inside and outside the clinic. Through its Committee on Health Promotion, the AEP offers its members tools to facilitate the pursuit of the ambitious objective that is improving the health of our patients through this “treatment” that is so human and characteristic of childhood and adolescence: the practice of PA and the increase of PA in our population.
Please cite this article as: Alvarez-Pitti J. et al. Ejercicio físico como ‘medicina’ en patologías crónicas durante la infancia y la adolescencia. An Pediatr (Barc). 2020;92:173–173.e7.