Spain is the European country where more assisted reproduction techniques (ART) are performed, reaching 9% of newborns. The objective of this article is to introduce the legal framework and to analyze some ethical questions, not without controversy, in relation to the anonymity of gamete donors and the concealment of origin by ART from their children. Spanish legislation establishes the relative anonymity of donors: both gamete recipients and born children have the right to obtain general information about them as long as their identity is not included, but in situations of risk to the life and health of the children allows your bankruptcy. Likewise, an unequivocal right to privacy and confidentiality of submission to the TRA is established. The movement aimed at introducing in our country a legislative amendment that ends the anonymity of gamete donors is based on the right of those children to know their biological origin. Along with legal changes, the attitude of parents and professionals must gradually change towards more transparent and responsible communication, based on the experiences of adults conceived by these techniques, and those adopted. Building values such as trust and truth in the family relationships from responsibility requires placing the children, largely forgotten and the most vulnerable part, at the center of the debate.
España es el país europeo donde se realizan más técnicas de reproducción asistida (TRA), alcanzando el 9% de los nacidos. El objetivo de este artículo es introducir el marco legal y analizar algunos aspectos éticos, no exentos de controversia, en relación con el anonimato de los donantes de gametos y la ocultación del origen mediante TRA a los hijos. La legislación española establece el anonimato relativo de los donantes: tanto las receptoras de gametos como los hijos nacidos tienen derecho a obtener información general de los mismos siempre que no incluya su identidad, pero ante situaciones de riesgo para la vida y la salud de los hijos permite su quiebra. Asimismo, se determina un inequívoco derecho a la intimidad y confidencialidad del sometimiento a las TRA. El movimiento tendente a introducir en nuestro país una modificación legislativa que acabe con el anonimato de los donantes de gametos, se basa en el derecho de los nacidos a conocer su filiación biológica. Junto a los cambios jurídicos, la actitud de padres y profesionales debe ir modificándose hacia una comunicación más transparente y responsable, en función de las experiencias de los adultos concebidos por estas técnicas, y de los adoptados. Construir valores como la confianza y la verdad en el ámbito de las relaciones familiares desde la responsabilidad, requiere colocar a los hijos, grandes olvidados y parte más vulnerable, en el centro del debate.
“It’s a girl!” With great anticipation, on July 25, 1978 the world learned of the birth of Louise Brown, the first “test-tube baby”, possibly the most awaited birth in 2000 years according to Time magazine. In Spain, the first baby fruit of in vitro fertilization (IVF), Victoria Anna, was born on July 12, 1984, an event that also received considerable media coverage.
“It’s a girl!” With great anticipation, on July 25, 1978 the world learned of the birth of Louise Brown, the first “test-tube baby”, possibly the most awaited birth in 2000 years according to Time magazine. In Spain, the first baby fruit of in vitro fertilization (IVF), Victoria Anna, was born on July 12, 1984, an event that also received considerable media coverage.
Since then, it is estimated that more than 9 million children1 have been born worldwide with the help of assisted reproductive technology (ART). It has been a veritable revolution in human reproduction that was initially aimed to treat infertile couples and has since been applied to other situations (single women, same-sex couples). Political, economic, ethical and legal aspects have resulted in substantial differences in the application and development of ART,2 the most important of which include factors like the accessibility and cost of treatment, but also cultural aspects and beliefs and personal and career choices that result in the postponement of childbearing. The large constellation of potential situations in Europe3 is complex in terms of the law, regulations, approved techniques, indications, the age windows for donors and recipients, the maximum number of offspring per donor, public funding or the registries of ART users and donors. These differences have given rise to the phenomenon known as reproductive tourism in search of countries with less stringent laws.
Spain is the leading country in Europe and third in the world in the number of performed ART treatments. In 2018, the 149 337 cycles of IVF and 34 100 artificial insemination procedures resulted in 37 094 births. This fact, which corresponds to a proportion of births after ART of more than 9% of the total births,4 involves a paradox (the birth rate is decreasing but the number of children born after ART increasing) as well as a certain incongruence (the popularity of ART contrasts with the secrecy that usually surrounds these births). This is reflected by the fact that while hospital discharge summaries may document the birth after ART, if it is mentioned at all, it is not infrequent for parents to request that this fact be excluded from the health record of the minor.5
All of this raises novel ethical dilemmas and countless questions: Who decides which data should be included in the health record (HR) and based on which criteria? Can patients decide which information to share or not share with their doctors? Is it possible to request the removal or modification of previously recorded information? If a potentially severe genetic disorder is diagnosed, should the donor or other potentially affected individuals born from the donor gametes be notified? Does the child have a right to know their biological origin?
The aim of this article is to introduce the legal framework of the anonymity of gamete donors and the concealment from the offspring of their history of birth after ART and analyse some associated ethical aspects that may be controversial in order to guide prudent clinical decision-making.
Contents on the right to anonymity in assisted reproductive technologyIn Spain, the right to anonymity established in Law 14/2006 regulating ART only refers to the right of the donor to not be identified, but this law also guarantees the confidentiality of health care, and therefore 2 different issues need to be addressed: the right to privacy and confidentiality in undergoing ART procedures, and the anonymity of donors in the strict sense (Table 1).
Contents of the right to anonymity and confidentiality in assisted reproductive technology.
| Law 14/2006 on assisted reproductive technology establishes that gamete donation will be anonymous and that gamete banks will guarantee the confidentiality of the personally identifiable data of the donor, as will any established donor registries and registries of the activity in associated facilities. At the same time, the same law dictates that all the information must be documented in individual health records guaranteeing confidentiality as concerns the identity of the donor, the data and health information of the users and the circumstances surrounding the origin of donor-conceived individuals. Therefore, it is necessary to distinguish two aspects of the right to privacy: on one hand, privacy in relation to the process itself, that is, to the fact that an individual is the recipient of gamete donation and ART, and on the other, the anonymity provided to gamete donors |
Reproduction belongs to the sexual life of individuals, to their private life, and individuals have the right to disclose what they see fit and keep whatever they wish private.6 The right to privacy of individuals that undergo ART procedures, as is the case of any other medical intervention, is clearly supported by the law. However, this right is in conflict with the right to know of the offspring, a conflict that is not limited to the legal sphere but that also has significant ethical and clinical repercussions.7 The main barrier to concealing the use of ART from the offspring is that Law 41/2002 on patient autonomy (PA) establishes the right to know all the available information on one’s own health, based on which the concealment of the genetic origin does not seem appropriate.
Leaving aside the will of the parents, the use of ART is documented in 3 types of HRs whose contents and the access to which are regulated by the law, which guarantees that it will be possible for the offspring to obtain information about their biological origin.
Health records in assisted reproductive technology facilitiesThe law on ART establishes that all the information pertaining to it has to be documented in individual HRs and that these data, “with the exception of the identity of the donors, should be made available to the recipient and the recipient’s partner or the child born after use of these techniques or the legal representatives of the child once the child is of age, if they so request.” That is, the law itself establishes that the child, having reached adulthood, can access this information.
Health care records of gamete recipients in health care facilitiesThe law on PA establishes that the HR will include any information considered clinically relevant and that its ultimate purpose is to facilitate the delivery of health care by documenting any data that, in the judgment of the clinician, will provide an accurate and up-to-date picture of the health condition of the patient. Thus, health care providers are the individuals responsible for deciding which data should be included in the HR and for how long based on the relevance of the information, and it would be difficult to find arguments to support the notion that, at least during pregnancy and delivery, information concerning conception after ART is not relevant.
Health care records of individuals born after assisted reproductive technology in health care facilitiesAs we said, clinical relevance is what determines whether the biological origin of the child should or not be included in the HR. Another issue is how to adequately protect this information so that it does not appear by default in any form of clinical documentation unless it is necessary.
In addition to the relevance criterion, the law on PA establishes that when it comes to the delivery of the child, the HR must include all biometric, clinical and laboratory findings required to establish the relationship with the mother and that these data will remain in the record indefinitely. It is obvious that in the case of ART with donated eggs it will not be possible to add this information to the HR, but in this case a note must be included somewhere in the record to justify this apparent failure to comply with the law.
The right to anonymity of gamete donorsDonor anonymity in current lawWe ought to note that the law on ART does not provide for absolute anonymity. It establishes that while donation may be anonymous, both gamete recipients and the offspring have the right to obtain general information about the donors excluding their identity, and allowing, under extraordinary circumstances that pose a certain risk of death or to the health of the child, disclosure of the identity of the donor.
The diagnosis of a genetic disorder in the child that could pose a serious threat to the health of the donor has been proposed as a potential exception to anonymity.8 In such cases, it would be possible for the health care team to contact the facility where the ART procedures were performed to inform the donor and prevent the use of the donated gametes, or, if the latter have already been used, to inform any other offspring of the risk. These exchanges of information can be performed without breaking the anonymity of donors, as they do not require disclosure of their identity.
Thus, when there is an important health reason, what needs to be shared is the health information and disclosing the identity of the donor is not necessary, with very rare exceptions. Therefore, the debate about anonymity does not arise from arguments related to health, as current law contemplates breaking anonymity when necessary.
New tendencies toward the abolition of anonymity and arguments in support of anonymityThe Spanish law on ART settled on donor anonymity, following the general trend in Europe years ago. However, the prevailing tendency at present is to consider that the offspring have the right to know the identity of the donor, upon reaching age 18 years, if they so desire.9 Neighbouring countries such as Norway (2003), the Netherlands (2004), the United Kingdom (2005) and Finland (2006) repealed the right to anonymity originally established; Austria, the Netherlands, Switzerland and Germany allow disclosure of the donor; Portugal (2018) considers anonymity unconstitutional. United States law allows the donor to choose whether or not to remain anonymous.
In Spain, this issue has been subject to substantial debate, but nearly exclusively from a legal standpoint. Those who oppose anonymity argue that it infringes the constitutional principle of equality, as individuals born after spontaneous conception have a right to research biological paternity and maternity, an option that is denied to individuals born after ART.10,11 One relevant consideration is that Law 26/2015 amending the system for child and youth protection has repealed anonymity in adoption, stipulating that adopted or foster care children have a right to know their biological origin once they reach the age of majority or before that time through their legal guardians. As early as 1999, the Supreme Court12 had declared the regulation of the Civil Register that allow anonymous delivery unconstitutional on account of violating the dignity of the child and their right to know their maternal filiation.
What will definitely affect legislation changes in Spain is the position adopted by the European Union, which has already been announced in the provisional version of Recommendation 2156/2019.13 This Recommendation already reflects the movement in support of recognising the right of offspring to know their biological origins, seeks to repeal anonymity in future gamete donations and forbids the use of anonymously donated gametes, and establishes that the identity of the donor should be disclosed to the offspring once they reach the age of maturity while maintaining their right to not know.
Ethical aspectsThe diversity in the origins of children is as old as humanity itself. There have always been children that were adopted, given away, bought or fruit of known or agreed-on extramarital relations. In Spain, until a few years ago, domestic adoption in the absence of divorce, blended families or same-sex parents corresponded to an invisible minority within a social context that favoured secrecy.
The current situation is quite different, with an evident and visible change in recent decades in maternity, paternity and the ways to start a family. These changes have been brought on by international adoption, same-sex and single-parent parenthood and birth after ART with gamete donation, embryo adoption or surrogacy.14 All of these give rise to a complex and diverse spectrum of families, both in visible and invisible ways. Families held together by emotional bonds rather than genetic ones. A revolution that is also an enrichment.
Moving away from paternalism, the need to inform the offspringSocial progress and change clash with the regressive tendency to conceal from offspring their conception using ART, made invisible by the absence of external factors that would make them identifiable, which is similar to what occurred with domestic adoptions in the past. However, leaving aside the appropriateness of these methods, confusing privacy with concealment impinges on values like transparency, truth or the right to know one’s own origins and may actually mask a paternalistic attitude that runs counter to the pursuit of patient autonomy.
Recently, in addition to changes in legislation, the attitude of parents and health care professionals has been shifting towards more transparent and responsible communication based on the experience of adults conceived using ART and adult adoptees.15
Many studies have evaluated the appropriateness of parents informing their children about their conception through the use of donated gametes. This disclosure, which may be made at an early age (3–4 years), in adolescence or in adulthood, tends to be traumatic and difficult; many of these individuals express that they wish they had been informed by their parents when they were children, would like to have information about the donor or even meet the donor and their potential siblings, which brings up another important issue: the possibility of identifying the biological parent that donated the gamete.
The main concern for some parents is that their child will develop an emotional bond with the donor, and the absence of a genetic connection or the experience of childbearing seems to make fathers more likely to maintain secrecy compared to mothers.16
Despite these changing trends, it is worth noting that a high percentage of Finnish fathers (66.7%) and mothers (49.6%) reported that they had not disclosed the use of ART to their health care providers and expressed upset that health care staff mentioned the subject in the presence of the child.15
The need for honesty and the right of the child to know, in addition to the risk that the child discovers the truth by accident, are the main reasons for disclosure. Chief among the arguments in support of concealment is that this information may not be needed, followed by fear that it may hurt the child.17
Controversies regarding donor anonymityThe Committee of Bioethics of Spain,18 in line with other European countries and focusing on the best interests of the child, has proposed a law reform to eliminate the current provision of anonymity in gamete donation in Spain, noting that this change in legislation must be accompanied by a true cultural shift in the field of assisted reproduction and in the relationships between parents, individuals born after ART and genetic progenitors.
In contrast to these positions, others argue that donor anonymity should be maintained. The main argument used in support of it is that repealing anonymity could lead to a decrease in donations, thus affecting treatments and the quality of care.19 This is the position of the Sociedad Española de Fertilidad (Spanish Society of Fertility),20 which has stated that the elimination of anonymity “would have a significant deleterious impact on the care offered in Spain to the group of individuals that need donated gametes to reproduce”. It also proposes that there is a risk that the role of the parent may be undermined by the figure of the donor, which could have a negative impact on the family and interfere with the healthy development of attachment and identity.
Another potential consequence of repealing anonymity would be a decrease in the number of donors. But even then, there may be positive consequences of this, such as a potential shift in the donor profile toward more altruistic and responsible individuals moved by solidarity with a decrease in donors motivated by economic gain, such as socially disadvantaged individuals that are more vulnerable to economic exploitation.21
We cannot neglect to mention that in a field in which economic aspects are very important, potential conflicts of interest surrounding ART may result in the silencing of ethical arguments concerning the protection of the best interests of the child.22 Establishing values like trust and truth in the family sphere or responsibility, honesty and transparency in the science sphere requires placing the children, the often forgotten party that is also the most vulnerable, at the centre of the debate.
Although some believe that knowledge of their biological origin could generate confusion and not be good for donor-conceived individuals,23 the arguments in support of the right to know the so-called “biological truth” seem to carry more weight, along with the emotional need of every person to know their origin and the identity of their parents,18 which would prevent the feeling of “genetic orphanhood” and loss of identity experienced by some donor-conceived individuals.
Lastly, although it is the parents that have the power to decide whether or not to share this information and should exert it responsibly, all involved health care professionals must encourage them to do so, as recommended by the Nuffield Council on Bioethics.24
Offering counselling prior to performance of fertility treatments is key to achieve real change towards increased transparency, which unquestionably requires providing parents with additional psychological support and guidance on how to share the information with their children.
The need for registriesFrom the scientific and clinical standpoints, sharing the information of ART registries and HRs of individuals born after ART is essential.25 These records will allow evaluation of the data on the safety and cost-effectiveness of the different ART modalities26 and to carry out long-term surveillance to determine the actual incidence of associated health problems,27,28 such as genomic imprinting disorders (Wiedemann-Beckwith, Angelman, Silver-Russell, Prader Willi).29 Families should be informed of this association, as there is an increase in the relative risk of these disorders, even if the absolute risk is low. Furthermore, donor registries should be managed appropriately in accordance with the law, ensuring their responsible use and minimising the risk of future inadvertent consanguinity.
On the other hand, the widespread application of genomic techniques to medical diagnosis calls for the creation of DNA banks to make it possible to trace the genetic origins of inherited diseases.30,31
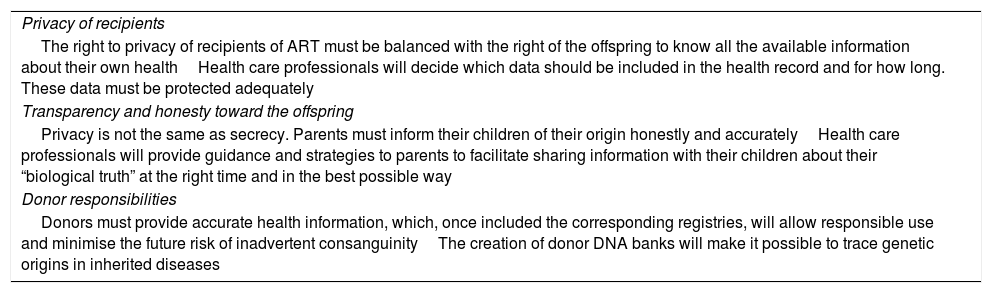
Table 2 presents the main ethical concerns that arise in relation to gamete donation.
Ethical considerations in gamete donation.
| Privacy of recipients |
| The right to privacy of recipients of ART must be balanced with the right of the offspring to know all the available information about their own healthHealth care professionals will decide which data should be included in the health record and for how long. These data must be protected adequately |
| Transparency and honesty toward the offspring |
| Privacy is not the same as secrecy. Parents must inform their children of their origin honestly and accuratelyHealth care professionals will provide guidance and strategies to parents to facilitate sharing information with their children about their “biological truth” at the right time and in the best possible way |
| Donor responsibilities |
| Donors must provide accurate health information, which, once included the corresponding registries, will allow responsible use and minimise the future risk of inadvertent consanguinityThe creation of donor DNA banks will make it possible to trace genetic origins in inherited diseases |
In short, it is important to differentiate the issue of donor anonymity from the issue of informing offspring of their biological origin through the use of ART. New social realities and family forms pose challenges that require reconsidering the rights of children whose genetic origin does not correspond to their parents. Parents require more psychological support and to be given strategies on how to disclose this information to their children. Fostering a social environment in which being conceived through gamete donation is not stigmatised will help diminish the current secrecy surrounding disclosure of this health-related information, along with an increased commitment of health care professionals and institutions to the protection of these data.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Riaño-Galán, C. Martínez González, Gallego Riestra S, Cuestiones éticas y legales del anonimato y la confidencialidad en la donación de gametos. An Pediatr (Barc). 2021;94:337.