Intervention for childhood obesity is a public health priority. The purpose of this study was to evaluate the effectiveness of an elementary school-based intervention against obesity in children.
Materials and methodsNon-randomised controlled trial was conducted on children from first to fifth grade from two public schools of Avilés (Spain). The intervention lasted for 2 school years comprising healthy diet workshops, educational chats, educational meetings, informative written material, and promotion of physical activities. Primary outcome measure was body mass index z-score. Secondary outcomes included obesity and overweight prevalence, waist circumference, dietary habits, and physical activity.
ResultsA total of 382 (177 girls, 205 boys) out of 526 pupils of both schools were included in the study. Complete anthropometric data were obtained in 340 of the 382 individuals. Compared to children in the control group, those in the intervention group decreased body mass index z-score from 1.14 to 1.02 (P=0.017), and improved KIDMED score from 7.33 to 7.71 points (P=0.045). The percentage of students who carried on an optimal diet increased from 42.6% to 52.3% (P=0.021). There were no statistical differences in the prevalence of obesity and overweight, or in waist circumference between the intervention and control groups.
ConclusionsThis school-based programme resulted in modest beneficial changes in body mass index and diet quality.
Las intervenciones sobre la obesidad infantil son una prioridad para la salud pública. El objetivo de este estudio fue evaluar la efectividad de un programa de intervención contra la obesidad en un colegio de Educación Primaria.
Material y métodosEstudio de intervención controlado no aleatorizado en alumnos de primero a quinto cursos de Educación Primaria en 2 colegios públicos de Avilés (España). La intervención se desarrolló durante 2 cursos escolares, incluyendo talleres sobre alimentación saludable, charlas educativas, material informativo escrito y promoción de la actividad física. La variable de resultado principal fue la puntuación z del índice de masa corporal (IMC). Como variables de resultado secundarias se consideraron: prevalencia de obesidad y sobrepeso, perímetro abdominal, hábitos de dieta y actividad física.
ResultadosFueron incluidos en el estudio 382 (177 niñas, 205 niños) de 526 alumnos de ambos colegios. En 340 individuos se obtuvieron datos antropométricos completos. A diferencia del grupo control, los pertenecientes al grupo de intervención disminuyeron la puntuación z del IMC desde 1,14 a 1,02 (p=0,017), mejoraron el índice KIDMED de adhesión a la dieta mediterránea de 7,33 a 7,71 puntos (p=0,045) y aumentaron la proporción de estudiantes con una dieta óptima del 42,6% al 52,3% (p=0,021). No se encontraron diferencias estadísticamente significativas en la prevalencia de obesidad y sobrepeso, ni en el perímetro abdominal, entre los grupos de intervención y control.
ConclusionesEste programa escolar consiguió pequeñas mejoras en el IMC y la calidad de la dieta.
The prevalence of childhood overweight and obesity has increased considerably worldwide since the 1990s,1,2 although recent studies show that it is stabilising in some developed countries.3 The high prevalence of overweight and obesity in the young population has been attributed partly to a decrease in physical activity and an increase in sedentary behaviours. There is also a clear trend for individuals to have a combination of several cardiovascular risk factors that is more marked in obese children and adolescents. Nearly half of the children with severe obesity meet the criteria for metabolic syndrome.4 The cardiovascular and metabolic consequences of obesity, such as hypertension, insulin resistance and dyslipidaemia, which may already be present in childhood, are particularly worrisome.
Childhood overweight and obesity carry an increased risk of becoming an overweight or obese adult.5 It is also known that treating obesity with lifestyle changes is extremely difficult in adults.6 Thus, interventions should focus on treatment and prevention in the paediatric population.
Public health strategies have been advocated to improve cardiovascular health in children, as research shows that they are more effective and easier to implement than other, more selective strategies based on risk factors.7 The school setting offers ample opportunity for intervention programmes. For all of the above, school-based programmes have been developed that aim at reducing childhood obesity and other cardiovascular risk factors, usually by attempting to improve diet and physical activity.
The early literature reviews on school-based interventions for the prevention of childhood obesity have shown inconsistent results.8–14 However, studies on this subject published in recent years and new literature reviews and meta-analyses have found strong evidence that integral school-based interventions can be effective in reducing body mass index (BMI).15–17
The aim of our study was to assess the effect of an integral school-based intervention on BMI, as well as on the prevalence of overweight and obesity and lifestyle habits such as diet and physical activity.
Materials and methodsType of studyWe carried out a school-based programme for preventing obesity designed as a non-randomised controlled trial. We selected two public elementary schools in the town of Avilés (Asturias, Spain). The intervention group consisted of the first- to fifth-year students of the Villalegre public school. This school was chosen for the intervention because the previous year its teaching staff had expressed an interest in implementing a programme to fight obesity in collaboration with the Hospital San Agustín of Avilés. The control group included the students enrolled in the same years at the El Quirinal public school, located in another Avilés neighbourhood of similar socioeconomic characteristics. The two schools are 3.5km apart, separated by a national highway. The school principals and the parent associations were given detailed information about the study and agreed to participate. The study was approved by the Comité de Ética de la Investigación (Committee on Research Ethics) of the Principality of Asturias, and we obtained the written informed consent of the parents or legal guardians of participating students.
InterventionThe intervention project, called “Tú decides tu salud. ¡Ponte a vivir!” (Your health is up to you. Start living!) was implemented for 2 consecutive academic years (September through June) The activities of the programme were designed by the teaching staff of the school under the guidance of the paediatricians of the research team, and were carried out in the school. The programme was supported by the Asociación de Madres y Padres de Alumnos (Association of Students’ Mothers and Fathers), with whom we held several meetings prior to the study to explain the project and receive suggestions.
The activities carried out consisted of: (1) workshops on healthy nutrition for the students, offered every term (trimester) of the academic year. Once each term, a workshop for all the students of approximately 60min of duration was conducted by two paediatricians from the research team, and supplemented with activities on the same subject led by teachers in the classrooms every two weeks or every month. The first term emphasised the importance of having breakfast to achieve an optimal diet; in the second term, the focus was on the need of having a varied diet; and in the third term there was a discussion of which foods are more or less healthy. In the second year of the intervention, the workshops focused on healthy snacks and the importance of eating fish, fruits and vegetables; (2) educational talks for the parents, 60min long, offered once each term, on the same subjects covered in the workshops attended by the children, and given by a paediatrician from the research team; they took place in the evening hours to facilitate family attendance; (3) a joint 2-h long workshop on healthy cooking and nutrition, carried out collectively by paediatricians, teachers and students’ parents, offered once each academic year; (4) monthly meetings with teachers to study healthy lifestyle habits and nutrition and to resolve any doubts about these subjects; (5) printed informational materials for the parents developed by the school's teaching staff on recommendations and limits pertaining to physical and sedentary activities, and how to follow a healthy diet, and (6) promotion of physical activity in recesses, for example, by recovering traditional outdoor children's games. In agreement with the Asociación de Madres y Padres de Alumnos, the use of handheld game consoles and mobile phones was banned during school hours.
During the period of the study, no such interventions were scheduled to be performed in the control school.
Outcome variablesThe primary outcome measure was the BMI z-score (BMIz). The secondary outcome measures were the prevalence of obesity and overweight, waist circumference (WC), dietary habits and physical activity. The measurements were taken consecutively in both schools at the beginning of the intervention in October 2006 and at the end in June 2008.
Weight was measured with the students barefoot and in light clothing, and was rounded to an accuracy of 0.1kg with a calibrated scale (Seca GmbH & Co. KG, Hamburg, Germany). Height was measured with the students barefoot and rounded to the nearest millimetre using a rigid stadiometer (Año Sayol SL, Barcelona, Spain). Obesity and overweight were defined based on BMI (kg/m2) applying the cut-off points of the International Obesity Task Force.18 The World Health Organization (WHO) 2007 growth reference charts were used to calculate BMIz. We measured WCs with a measuring tape at the level of the waist, between the last rib and the iliac crest, at the end of a normal expiration.19
The quality of the diet was assessed by the KIDMED Mediterranean Diet Quality Index. It is a questionnaire comprising 16 questions concerning the Mediterranean diet, the final score of which gives the KIDMED index, used to categorise the diet into 3 levels: ≥8, optimal diet; 4–7, dietary habits requiring improvement for better adherence to the Mediterranean pattern, and ≤3, very low quality diet.20
Physical activity habits were assessed by means of the Physical Activity Scale,21 a self-administered questionnaire that has been previously used in children22 with questions covering time spent at school, spare time and sports activities.
Statistical analysisThe data were analysed with the SPSS 17.0 software (SPSS Inc., Chicago, USA). We assessed the normality of the distributions by means of the Kolmogorov–Smirnov test. We used Student's t test for independent or paired samples and the Mann–Whitney–Wilcoxon test as applicable. We compared proportions by means of the chi square test. We used McNemar's test to compare proportions before and after the intervention. The level of statistical significance was set at P<0.05. We have expressed discrete variables as percentages and continuous variables as mean±standard deviation or median (interquartile range) depending on whether or not they followed a normal distribution.
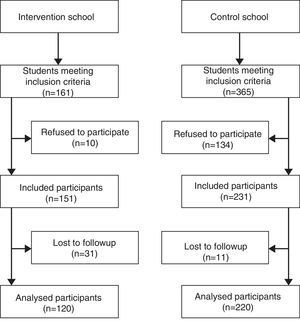
ResultsThe study included 382 of a total of 526 students enrolled in the first to fifth years of elementary education in the two schools (177 girls, 205 boys), with an initial mean age of 8.4 years (range, 5.8–11.8 years). One hundred and forty four students declined to participate. We obtained the full anthropometric data for 340 of the 382 participants (162 girls, 178 boys). Fig. 1 shows a flow chart of the study participants; losses to follow-up were due to students being absent at the time of the second measurement or changing schools. The Physical Activity Scale questionnaire was completed by 213 children, 150 from the control group and 63 from the intervention group. The initial characteristics of both groups are shown in Table 1. When the study started, the participants in the intervention and control groups did not differ in age, sex distribution, BMIz, WC or KIDMED index. The students in the intervention school spent less time on sedentary activities and more time on physical activities. We detected overweight or obesity in a total of 141 students from both groups (41.5%). In both groups, the prevalence of overweight or obesity was greater in boys than in girls (42.0 vs 38.9% in the control school and 48/5 vs 37.0% in the intervention school), although this difference was not statistically significant.
Participant characteristics at the beginning of the study.
| Variable | Control | Intervention | P |
|---|---|---|---|
| n | 220 | 120 | |
| Female, % | 49.1 | 45.0 | 0.497 |
| Age (in years) | 8.5±1.46 | 8.19±1.5 | 0.067 |
| BMIz | 0.92±1.18 | 1.14±1.25 | 0.245 |
| WC, cm | 64.62±8.61 | 65.18±10.94 | 0.625 |
| KIDMED index | 7.57±1.74 | 7.4±1.64 | 0.420 |
| Sedentary activities, h/day | 17.92±2.17 | 17.01±2.89 | 0.009 |
| Physical activities, h/day | 5.13±2.38 | 5.96±3.21 | 0.020 |
| Obesity, % | 10.5 | 16.7 | 0.124 |
| Overweight, % | 30.0 | 26.7 | 0.534 |
| Obesity or overweight, % | 40.5 | 43.3 | 0.646 |
| WC>95th %ile, % | 55 | 55 | 1 |
Data are expressed as mean±standard deviation or as percentages.
BMIz, body mass index z-score; WC>95th %ile, waist circumference>95th percentile.
Table 2 shows the observed changes in BMIz in the intervention and control groups. The BMIz decreased significantly in the intervention group (initial, 1.14±1.25; final, 1.02±1.23; P=0.017), while no significant changes were observed in the control group (initial, 0.92±1.18; final, 0.98±1.09; P=0.150). When we analysed the results stratifying by sex, we observed that in the intervention school the BMIz only decreased significantly in girls, while in the control school it increased significantly in boys.
Evolution of the body mass index z-score (BMIz) in the intervention and control schools, overall and by sex.
| Control | Intervention | |||||
|---|---|---|---|---|---|---|
| Initial | Final | P | Initial | Final | P | |
| Total | 0.92±1.18 | 0.98±1.09 | 0.150 | 1.14±1.25 | 1.02±1.23 | 0.017 |
| Girls | 0.75±1.00 | 0.73±1.02 | 0.680 | 0.74±1.23 | 0.60±1.24 | 0.042 |
| Boys | 1.09±1.31 | 1.23±1.10 | 0.032 | 1.46±1.18 | 1.35±1.12 | 0.145 |
The data are expressed as mean±standard deviation.
There was a decrease in the prevalence of obesity in both groups that was not statistically significant, of 3.3% (95% confidence interval [CI], −9.6% to 2.7%) in the intervention group and 1.8% (95% CI, −5.2% to 1.3%) in the control group. When we considered the combined prevalence of overweight and obesity, the differences were more pronounced in both groups, although they still did not reach statistical significance: in the intervention group, it decreased by 3.3% (95% CI, −10.7% to 4.1%), while in the control group it increased by 2.3% (95% CI, −2.9% to 7.4%).
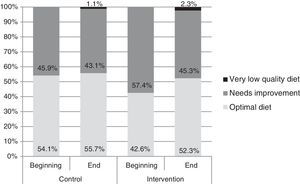
As for the impact of the programme on eating habits, the KIDMED index of the intervention group improved, changing from 7.33±1.61 to 7.71±1.77 points (P=0.045), while we found no statistically significant differences in the control group, the index of which changed from 7.61±1.76 to 7.55±1.66 (P=0.603). The number of students that followed an optimal diet also increased in the intervention group (Fig. 2), from 42.6% to 52.3% (P=0.021), while no significant differences were observed in the control group (from 54.1% to 55.7%; P=0.742).
The effects on physical activity habits are shown in Table 3. We did not find statistically significant differences in the intervention group between the beginning and the end of the intervention. In the control school, we only found a small increase in the time spent on helping with house chores and using computers and videogames, along with a decrease in the duration of sleep and rest. When we compared both schools at the end of the programme, we found no statistically significant differences in the time spent on physical activities.
Distribution of physical and sedentary activities at the beginning and the end of the intervention.
| Activity | Control, n=150 | Intervention, n=63 | ||||||
|---|---|---|---|---|---|---|---|---|
| Initial (h/day) | Final (h/day) | Difference (min/day) | P | Initial (h/day) | Final (h/day) | Difference (min/day) | P | |
| Sleeping, resting | 10.0 (10.0–10.0) | 10.0 (9.0–10.0) | 0 (−60 to 0) | 0.026 | 10.0 (9.0–10.0) | 10.0 (9.0–10.0) | 0 (−45 to 30) | 0.599 |
| Sitting, in class, TV, or reading | 7.0 (6.0–8.0) | 7.0 (6.0–8.0) | 0 (−60 to 60) | 0.720 | 6.0 (5.0–7.5) | 6.0 (5.0–7.0) | 0 (−71 to 60) | 0.165 |
| Computer, videogames | 0.5 (0.25–1.0) | 1.0 (0.5–1.5) | 15 (0 to 30) | 0.002 | 0.5 (0.25–1.0) | 1.0 (0.5–1.75) | 15 (0 to 30) | 0.732 |
| Organising, cleaning up | 0.25 (0.25–0.5) | 0.5 (0.25–0.5) | 0 (−15 to 15) | 0.464 | 0.5 (0.25–0.5) | 0.5 (0.25–0.5) | 0 (−3 to 15) | 0.403 |
| Playing outdoors, running errands | 1.38 (1.0–2.0) | 1.9 (1.0–2.1) | 0 (−30 to 31) | 0.737 | 2.0 (1.0–2.5) | 1.9 (1.0–2.1) | 0 (−37 to 30) | 0.610 |
| Helping with house chores | 0.25 (0.0–0.5) | 0.5 (0.25–1.0) | 15 (0 to 15) | 0.002 | 0.25 (0.0–0.5) | 0.5 (0.25–1.0) | 0 (0 to 15) | 0.169 |
| Walking | 1.0 (0.5–1.25) | 1.0 (0.5–1.25) | 0 (−30 to 15) | 0.136 | 0.75 (0.5–1.5) | 1.0 (0.5–1.25) | 0 (−33 to 45) | 0.848 |
| Exercising, riding bicycle | 1.0 (0.5–1.75) | 1.0 (0.56–2.0) | 0 (−30 to 30) | 0.845 | 1.0 (0.5–2.0) | 1.0 (0.56–2.0) | 0 (−30 to 45) | 0.507 |
| Sports | 1.0 (0.5–1.5) | 1.0 (0.75–2.0) | 15 (−15 to 45) | 0.101 | 1.0 (0.5–1.5) | 1.0 (0.75–2.0) | 0 (−19 to 60) | 0.169 |
| Sedentary activities | 18.0 (16.8–19.3) | 18.5 (17.3–18.3) | 0 (−60 to 90) | 0.647 | 17.3 (15.5–19.0) | 17.5 (16.5–18.7) | 0 (−134 to 90) | 0.342 |
| Physical activities | 5.0 (3.6–6.1) | 5.0 (4.0–6.0) | 1 (−60 to 90) | 0.368 | 5.5 (4.0–6.8) | 6.0 (4.25–6.8) | 45 (−97 to 120) | 0.966 |
Data are expressed as median (interquartile range) in hours a day (h/day) or minutes a day (min/day). The difference corresponds to the final value minus the initial value.
The proportion of individuals with a WC above the 95th percentile did not change in a statistically significant manner compared to the beginning of the study: from 55.0% to 57.5% (P=0.664) in the intervention group and from 54.8% to 56.1% (P=0.719) in the control group.
DiscussionThe main finding of our study was a significant decrease in BMI in students in the intervention school compared to students in the control school. This decrease was only found in girls, but boys also benefitted, as the intervention prevented the increase in BMI observed in the control school. The intervention was also associated to changes in lifestyle, with an improvement in the quality of the diet.
The results of this study are consistent with the most recent literature reviews, which show strong evidence that school-based interventions may be moderately effective in helping reduce BMI in the paediatric population.16,17 However, these small changes achieved through population-based strategies – in this case, focused on the population of schoolchildren and their families – may have a more considerable influence on overall cardiovascular risk and a greater probability of having a long-lasting effect than results achieved with interventions that focus solely on high-risk individuals.7,23
Few studies have evaluated this type of intervention in Spain. The Avall study,24 an intervention over the course of 2 academic years on the dietary and physical activity habits of first-year elementary school students in Granollers, found that BMI and the combined prevalence of overweight and obesity increased less in the intervention group. The Movi programme,25 a two-year long project of physical activity during leisure time conducted in Cuenca with schoolchildren 9–10 years of age did not find differences in BMI between the intervention and the control groups. The best results were obtained in the EdAl study,26 a programme implemented over 3 academic years in school children 7–8 years of age in Reus that achieved significant reductions both in BMI and the prevalence of obesity in the intervention group.
Despite the reduction in BMI, this study did not show a decrease in the prevalence of overweight or obesity. This circumstance has been described in other studies with similar methodologies.27,28 While it was not statistically significant, we did observe a decreasing trend in the combined prevalence of overweight and obesity in the intervention group, compared to an increase in the control group. Something that stood out in our study was the high prevalence of overweight and obesity observed, higher than the prevalences found in other interventions or reported in prevalence studies conducted in the same autonomous community under similar circumstances.1 It may be that children with overweight and obesity are less susceptible to community-based strategies, but it is also possible that the effects on weight category are harder to prove in a small study than overall changes in BMI. At present, there is evidence that school-based interventions, especially those of long duration, are effective in reducing the prevalence of childhood obesity.11
Systematic reviews show that nutrition education, the promotion of physical activity and the fight against sedentary behaviours are key elements in the long-term prevention of childhood obesity.9,12,13,17 This is consistent with the findings in the intervention group of a higher KIDMED index and a greater proportion of children following an optimal Mediterranean diet at the end of the study. We found no differences in physical activity between the two groups.
There are limitations to this study. The sample size was small, and with only 2 schools participating, it was not possible to perform a cluster randomisation. We were careful to choose two public schools in neighbourhoods of similar socioeconomic characteristics, but far enough from each other so as to avoid group contamination to the extent possible. The intervention school was selected for the interest expressed in the past by its teaching staff in implementing a programme to fight obesity. The collaboration of educators is indispensable to carry out an intervention programme of this nature, so the results may not be generalisable to every school.
Another possible limitation of the study is that when it started, the students in the intervention school spent less time engaged in sedentary activities and more time engaged in physical activities than the students in the control school. This may be due to a previous greater involvement in health education on the part of the intervention school, but nevertheless the intervention improved its past results, as it obtained a higher KIDMED index of adherence to the Mediterranean diet. Thus, it is plausible that the observed reduction in BMI was due to the intervention.
Another limitation was the use of the Physical Activity Scale, a self-administered questionnaire to measure physical activity validated in the adult population but rarely used in children. Self-administered instruments provide information on the type and context of physical activity, but pedometers or accelerometers are more objective measurement tools.
This kind of school-based programme may be a feasible way to improve children's health without a large investment of human and material resources. In 1995, the WHO launched the Global School Health Initiative, an integral strategy that pursues teaching health information and skills in the classrooms, changing the school environments, and developing bonds with the community. According to the Health Evidence Network of the WHO, school-based programmes that promote good dietary and physical activity habits are among the most effective interventions.29
In conclusion, this school-based programme achieved improvements in BMI and dietary habits. More studies are needed to establish the real effectiveness of these interventions and learn whether the improvements achieved last through adulthood.
FundingThis project has been funded with a clinical and epidemiological research grant from the Fundación Ernesto Sánchez Villares (2006/02).
Conflicts of interestThe authors have no conflicts of interest to declare.
We want to thank all the teachers, students and families that participated in the project. We thank Isabel Aguilera, a teacher at the Villalegre public school, for her outstanding work and leadership in launching the school-based programme.
Please cite this article as: Pérez Solís D, Díaz Martín JJ, Álvarez Caro F, Suárez Tomás I, Suárez Menéndez E, Riaño Galán I. Efectividad de una intervención escolar contra la obesidad. An Pediatr (Barc). 2015;83:19–25.