Traumatic brain injury (TBI) is one of the main reasons for visiting paediatric emergency and, in the case of severe TBIs, for admission to paediatric intensive care units (PICUs).
It is crucial to avoid periods of cerebral hypoperfusion secondary to increases in intracranial pressure (ICP) and decreases in arterial blood pressure, which are associated with an increased morbidity and mortality.1 There is controversy regarding the optimal drugs to use for sedation and analgesia in its management, given that some, such as fentanyl, midazolam or propofol, cause secondary hypotension.
Ketamine could be an ideal option in the management of TBI, as it does not cause vasodilation, but there have been concerns regarding whether it could increase ICP.2 Recent studies conducted in adults have evinced a neuroprotective effect through the reduction of seizures and nonconvulsive status epilepticus.
Intracranial pressure can be measured invasively through an intracranial catheter or non-invasively with transcranial colour-coded Doppler (TCCD) sonography using the Gosling pulsatility index (PI), which has been found to be linearly correlated to changes in ICP.3
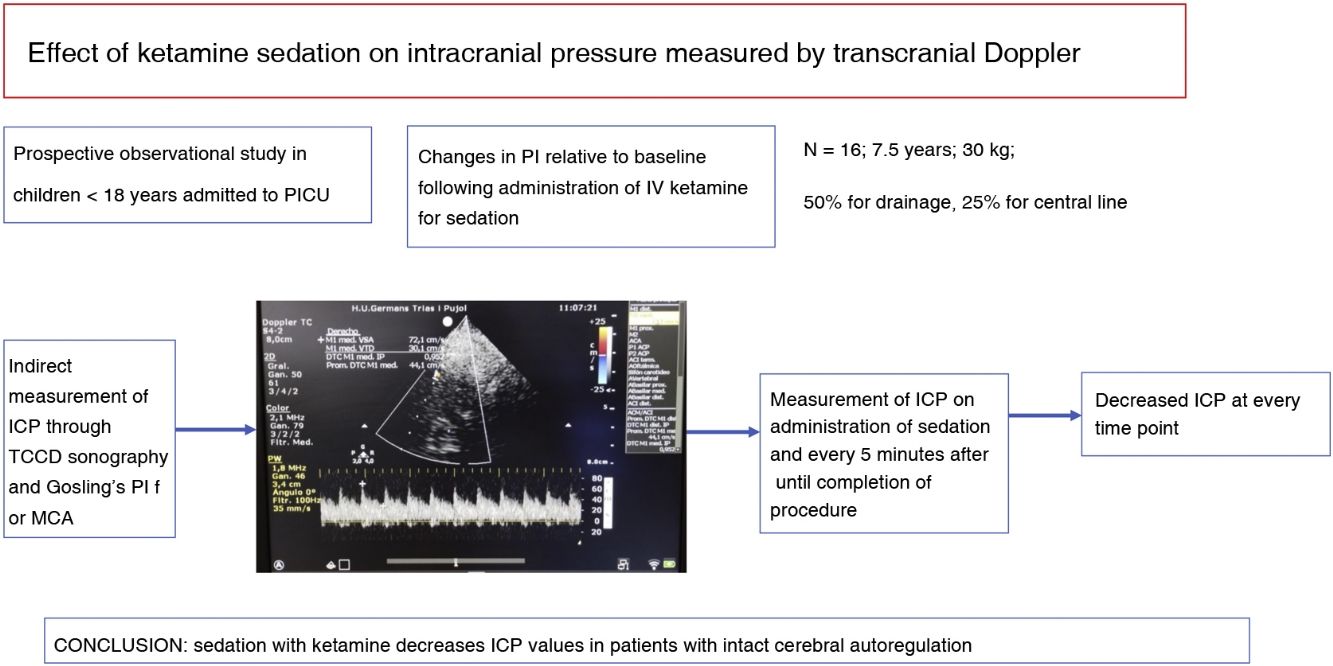
The aim of our study was to assess changes in cerebral blood flow that could lead to changes in ICP by means of TCCD sonography.
We conducted a prospective observational study. The study was approved by the local ethics committee. We obtained the informed consent of the parents or legal guardians of the participants.
The sample consisted of paediatric patients admitted to the PICU who required sedation for a procedure, including patients with mild TBI. We excluded patients who were mechanically ventilated, who were already receiving another sedative and/or analgesic drug or with moderate to severe TBI.
The TCCD ultrasound examination was carried out per the protocol of the hospital with a 2.5 MHz convex probe and a Canon Xario 100 ultrasound machine. The patient was placed in the supine position and the left internal carotid artery was insonated through the left transtemporal window at different time points: before sedation, immediately after initiation of analgesia with ketamine (onset of nystagmus) and every 5 min thereafter until the procedure was completed.
The Gosling PI was calculated at the middle cerebral artery (MCA) as the difference between the peak systolic flow velocity and peak diastolic flow velocity divided by the mean flow velocity, and to assess the potential effect of vasospasm on the PI, we also calculated the Lindegaard ratio (mean flow velocity in the MCA/mean flow velocity in the ipsilateral extracranial internal carotid artery).3
The primary endpoint was the change in PI (ΔPI) following the administration of ketamine (1–2 mg/kg IV) compared to baseline.
We used the formula published by Bellner et al.,4 who found a +1 change in the IP compared to baseline with a correlation coefficient of 0.938, which corresponded to an increase in ICP of 5–6 mmHg.
The sample included 16 patients. Four of them had mild TBI. Table 1 presents the demographic and clinical characteristics of the patients. Table 2 presents the secondary clinical variables.
Demographic and clinical characteristics.
| n | 16 |
|---|---|
| Age (years) | 7.5 (3.2−12.7) |
| Female | 9 (56%) |
| Weight (kg) | 30.0 (16.2−48.9) |
| Reason for admission to the ICU | |
| Polytrauma | 6 (37.5%) |
| Central line placement | 4 (25%) |
| Pneumonia | 6 (37.5%) |
| Pneumothorax | 2 (12.5%) |
| Procedure requiring sedation | |
| Drainage placement | 8 (50%) |
| Vascular access | 4 (25%) |
| Burn care | 4 (25%) |
| Baseline pulsatility index | 0.85 (0.73–0.92) |
| Initial ketamine dose (mg/kg) | 1.5 (1.2–1.8) |
| Patients requiring a second ketamine dose | 4 (25%) |
| Second dose of ketamine (mg/kg) | 0.6 (0.5–0.7) |
| Timing of second dose (min) | 10.2 (6.8–12.9) |
Data expressed as median (IQR).
Secondary variables analysed at each time point.
| Pre sedation | At administration (P) | 5 min (P) | 10 min (P) | 15 min (P) | 20 min (P) | |
|---|---|---|---|---|---|---|
| HR | 95 (85–105) | 102 (90−118) (0.24) | 109 (95−120) (0.18) | 106 (93−116) (0.15) | 105 (95−115) (0.16) | 104 (96−112) (0.21) |
| SBP | 120 (115−125) | 125 (120−128) (0.56) | 130 (120−136) (0.37) | 135 (125−140) (0.12) | 138 (135−145) (0.11) | 132 (125−135) (0.16) |
| DBP | 65 (60−70) | 68 (65−75) (0.44) | 72 (68−75) (0.25) | 71 (65−75) (0.28) | 70 (64−74) (0.39) | 67 (60−76) (0.55) |
| RR | 22 (18−25) | 24 (22−26) (0.76) | 25 (23−27) (0.63) | 25 (23−27) (0.57) | 24 (22−26) (0.71) | 26 (24−28) (0.26) |
| SpO2 | 99 (98–100) | 99 (98−100) (0.83) | 99 (98−100) (0.83) | 99 (98−100) (0.84) | 99 (98−100) (0.83) | 99 (98−100) (0.83) |
| ΔLR | N/A | 0.18 (0.15−0.24) (0.31) | 0.19 (0.16−0.26) (0.25) | 0.22 (0.18−0.24) (0.18) | 0.24 (0.2−0.27) (0.29) | 0.21 (0.18−0.23) (0.36) |
| ΔPI | N/A | –0.18 (0.1−0.22) (<0.001) | –0.21 (0.15−0.23) (<0.001) | –0.15 (0.1−02) (<0.001) | –0.16 (0.15−0.17) (<0.001) | –0.18 (0.16−0.2) (<0.001) |
Data expressed as median (IQR) and P (P value for comparison to baseline value).
DBP, diastolic blood pressure; HR, heart rate; RR, respiratory rate; SBP, systolic blood pressure; SpO2, oxygen saturation; ΔLR, change in Lindegaard ratio compared to baseline; ΔPI, change in pulsatility index compared to baseline.
The PI was decreased relative to baseline at every time point after the administration of ketamine (Table 2). No episodes of vasospasm were detected.
Our findings corroborate the results of a recent study5 conducted in a sample of paediatric patients with severe TBI and haemodynamic instability, in which the authors observed a decrease in ICP values following the administration of ketamine. Our study confirms these results in patients with intact cerebral autoregulation, with findings similar to those of Stem et al.,6 but including patients with mild TBI and carrying out the assessments with color-coded instead of conventional transcranial Doppler ultrasound.
Studies assessing the effects of ketamine on ICP have been carried out in patients admitted to intensive care units,5 likely to require mechanical ventilation, inotropic support and hyperosmolar therapy, which may lead to changes in osmolality and oxygen and carbon dioxide concentrations and Doppler artifacts in the assessment of ICP, which hinders the interpretation of the real effects of ketamine.
Therefore, further studies are required to establish strong recommendations regarding the use of ketamine in paediatric patients who do not require respiratory support.
Previous meeting: This study was presented at the 37th Congress of the Sociedad Española de Cuidados Intensivos Pediátricos.