Malaria causes around 863,000 deaths per year, most of them in children under 5 years old.
Material and methodsWe have reviewed the epidemiological data of malaria cases in a paediatric department in a hospital in the Community of Madrid, in the period 1996–2011.
ResultsIn the period reviewed, 103 cases of malaria were diagnosed in children under 14 years old. Sixty percent were males and the average age was 4.5 years. In most cases, the infection arose during a visit to relatives in the country of origin. The vast majority did not have malaria prophylaxis. Twenty-five percent of the cases were diagnosed as complicated malaria, the main criteria being hyperparasitemia, of which 80% of the patients did not present any other complications.
ConclusionsA high level of suspicion must be maintained in any patient who comes from a malaria endemic area. The key factor responsible for the infection was the lack of chemoprophylaxis.
La malaria causa la muerte de unas 863.000 personas al año, la mayoría menores de 5 años.
Material y métodosSe realizó un estudio retrospectivo-descriptivo de los casos diagnosticados desde 1996 hasta 2011 en el Hospital Príncipe de Asturias de Madrid.
ResultadosEn el período estudiado se diagnosticaron 103 casos en menores de 14 años. El 60,2% de los pacientes fueron varones y la mediana de edad 4,5 años. La mayoría de los pacientes eran inmigrantes africanos recién llegados o inmigrantes residentes en España que viajaron para visitar familiares sin realizar profilaxis antipalúdica. El 25% de los casos fueron diagnosticados de malaria complicada, siendo el criterio principal la hiperparasitemia. De los pacientes que solo cumplían ese criterio, el 80% no presentó complicaciones.
ConclusionesEs importante mantener un elevado nivel de sospecha en pacientes que pro- ceden de zonas endémicas. El principal factor responsable de la infección fue la falta de quimioprofilaxis.
Malaria is the most important parasitic disease across the world. It is estimated that every year it causes new episodes in about 225 million patients, and the death of about 781,000 people,1 most of them children younger than 5 years.2 Due to increased migration flows from Africa in recent decades, malaria has become one of the most relevant imported parasitic infections in Spain.3 The global incidence of malaria has decreased in the past few years, thanks to control measures established by the World Health Organisation (WHO).4
We reviewed the cases diagnosed in our hospital over a period of 15 years (1996–2011) to get a global perspective of the characteristics of malaria in our setting.
MethodsThe Hospital Príncipe de Asturias is a secondary level hospital in the autonomous community of Madrid. We performed a retrospective descriptive study of the cases of malaria diagnosed in this hospital in children younger than 14 years between 1996 and 2011. We included cases diagnosed by malaria antibody detection, thick blood film, and/or polymerase chain reaction (PCR). We analysed the following variables: sex, age, country of origin, presenting clinical signs and symptoms, abnormal laboratory findings, treatment, complications, and outcome. We entered the collected data into an Excel database, and analysed them using descriptive statistical methods.
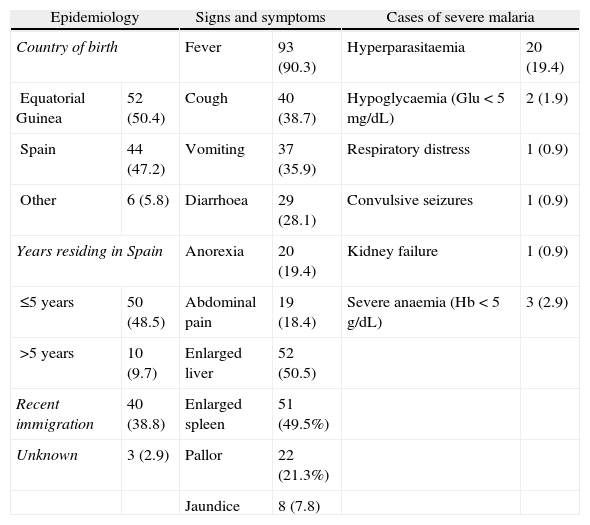
ResultsIn the 1996–2011 period, 103 cases of malaria in children younger than 14 years were diagnosed. Of all patients, 60.2% were male and 39.8% female. Patients younger than 5 years accounted for 54.4% of the total. Most patients were African immigrants who had just arrived in Spain, or immigrants residing in Spain that had travelled to their countries of origin to visit family (Table 1).
Most patients did not receive malaria chemoprophylaxis (73.8%), 2.9% received an incomplete course, and only 9.7% completed the treatment. Data about chemoprophylaxis were not available in 13.6% of the patients.
The distribution of cases by species was the following: Plasmodium falciparum (P. falciparum) 82 cases (79.6%), P. ovale 8 (7.7%), P. malariae 4 (3.8%), mixed parasitaemia 2 (1.9%), unknown 7 (6.8%). Diagnosis was based on detection of malaria antibodies in the emergency room, thick blood film, and PCR. Thirty-nine patients (37.9%) had low parasitaemia (less than 1% infected erythrocytes, or < 20,000 trophozoites/μL), 23 (22.3%) had moderate parasitaemia (1–5% infected erythrocytes, or 20,000–50,000 trophozoites/μL), and 20 patients (19.4%) had high parasitaemia (more than 5% infected erythrocytes, or >50,000 trophozoites/μL). Data on parasitaemia were not available for 20 patients.
Anaemia, defined as haemoglobin concentration below 11g/dL, was the most common abnormal laboratory finding (74.5%), followed by thrombocytopaenia (48.5%) and hyperbilirubinaemia (20.4%).
Severe complications of malaria5 developed in 25% of cases (Table 1). Of the 19.4% of cases meeting the criteria for high parasitaemia (parasitaemia>5% in stable transmission areas, and parasitaemia> 2% in low transmission areas), the majority (80%) did not develop any other complications. Thirteen patients (11.6%), 2 of whom had underlying sickle-cell anaemia, required a blood transfusion. Two patients were admitted to the paediatric intensive care unit (PICU). One of them was a patient diagnosed with human immunodeficiency virus infection with parasitaemia nearing 30%, who was consequently treated with intravenous quinine. The other patient admitted to the PICU was diagnosed with nephrotic syndrome and kidney failure. Both patients survived.
Epidemiological, clinical presentation, clinical examination, and laboratory data of patients with uncomplicated malaria and with severe malaria (absolute frequency and percentage).
| Epidemiology | Signs and symptoms | Cases of severe malaria | |||
| Country of birth | Fever | 93 (90.3) | Hyperparasitaemia | 20 (19.4) | |
| Equatorial Guinea | 52 (50.4) | Cough | 40 (38.7) | Hypoglycaemia (Glu<5mg/dL) | 2 (1.9) |
| Spain | 44 (47.2) | Vomiting | 37 (35.9) | Respiratory distress | 1 (0.9) |
| Other | 6 (5.8) | Diarrhoea | 29 (28.1) | Convulsive seizures | 1 (0.9) |
| Years residing in Spain | Anorexia | 20 (19.4) | Kidney failure | 1 (0.9) | |
| ≤5 years | 50 (48.5) | Abdominal pain | 19 (18.4) | Severe anaemia (Hb<5g/dL) | 3 (2.9) |
| >5 years | 10 (9.7) | Enlarged liver | 52 (50.5) | ||
| Recent immigration | 40 (38.8) | Enlarged spleen | 51 (49.5%) | ||
| Unknown | 3 (2.9) | Pallor | 22 (21.3%) | ||
| Jaundice | 8 (7.8) | ||||
The most frequent treatment was administration of quinine sulphate in conjunction with sulphadoxine-pyrimethamine in 57 cases (56.1%), followed by atovaquone-proguanil (14.6%), chloroquine (5.8%), mefloquine (5.8%), quinine sulphate in conjunction clindamycin (7.8%), and in a single case, quinine sulphate combined with doxycycline.
DiscussionMigratory flows have changed the epidemiology of malaria in Spain, where it had been eradicated since 1964, with a mean of 400 cases of imported malaria diagnosed each year.3
Of the patients under study, 54.4% were younger than 5 years at diagnosis, a relevant finding considering that malaria causes 8% of the deaths worldwide in children under the age of 5 years,2 making this age group particularly vulnerable.
In our case series, 32% of the patients were immigrants newly arrived to Spain, and 63.1% immigrants residing in Spain that contracted the disease when they returned to an endemic region to visit family and friends (referred to as visiting friends and relatives [VFR]).6 It was noteworthy that of all patients in our series with documented recent travel to their countries of origin, only 9.7% had completed the course of chemoprophylaxis. This compliance is low compared to other countries, such as France, where the reported figures of prophylactic treatment are near 40%,7 although our results are similar to those obtained in southern areas of the autonomous community of Madrid, where it was observed that only 1.8% have completed prophylaxis correctly.6 The children of immigrants living in Spain who travel with their parents to their country of origin are one of the most vulnerable population groups due to various circumstances, such as the loss of acquired immunity and a low risk awareness in parents. Furthermore, immigrants tend to travel for longer periods of time and in conditions of higher risk where the elements to fight the vector are not always set in place. Thus, even though tourism to malaria-endemic areas has increased in recent years, tourists account for a lower proportion of those infected.6
Equatorial Guinea, a former Spanish colony, was the most common country of acquisition in our series. P. falciparum was the infecting species in 80% of the cases, as it is the most prevalent species in sub-Saharan Africa. No cases of P. vivax were diagnosed, unlike in other countries such as the United Kingdom,8 where the population of South East Asian immigrants is larger than in Spain.
Treatment protocols have changed in the 15 years of the study due to the emergence of resistant pathogens, and while the most frequently used treatment was quinine in combination with sulphadoxine-pyrimethamine, it is being replaced by atovaquone-proguanil in adherence to current recommendations. Current guidelines already include artemisin-based therapies as the first-line treatment, even in countries with low transmission intensity.4,9 And a new formulation of dihydroartemisinin-piperaquine has recently been introduced in the European market.
Based on the criteria established by the OMS,4 25% of our cases met the criteria for severe malaria, with hyperparasitaemia being the most frequent one. Semi-immune patients (residents in a malaria-endemic area, or immigrants from an endemic area who have been living in a non-endemic area for less than 5 years) in stable transmission areas can tolerate parasitaemias of 20–30% with few or no symptoms,10 although in the absence of other data, parenteral treatment should be considered for parasitaemias higher than 20%.4–11 Recently, parenteral artesunate has been shown to be more efficacious than intravenous quinine.9 Most of the patients in our series who met only the criterion of hyperparasitaemia for severe malaria had favourable outcomes with oral treatment.4
In conclusion, given the nonspecificity of the clinical presentation of malaria, a high level of suspicion should be maintained in any immigrant patient with a history of recent travel to his or her country of origin, as early diagnosis is a key factor in the prognosis. The main factor accounting for infection acquisition in our series was not having undergone chemoprophylaxis. Since we performed a retrospective study, we could not analyse the reasons leading to the lack of chemoprophylactic treatment, or to the low compliance with it. New research is needed to elucidate the causes for this in order to address them and reduce the incidence of imported malaria in the paediatric age group. The latest recommendations indicate parenteral treatment for cases of severe malaria, but depending on the results, if hyperparasitaemia is the only met criteria for severe malaria, oral treatment could be considered, as most of these patients respond well to oral treatment.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Paredes P, Perez E, Guizar M, Penin M, Carrasco JG. Estudio descriptivo de los casos de paludismo en la poblacion pediatrica en un hospital general de Madrid entre 1996 y 2011. An Pediatr (Barc). 2014;81:322–325.