The estimated risks of infertility in childhood cancer due to radiation, chemotherapy and surgery are well known. The involvement of professionals and advances in the different methods of preservation are increasing. However, many patients do not receive information or perform any method of preservation.
MaterialQuestionnaires to paediatric onco-haematology institutions throughout Spain. The questionnaire consisted of 22 questions assessing their usual practices and knowledge about fertility preservation.
ResultsFifty members of the Spanish Society of Paediatric Haematology and Oncology, representing 24 of 43 centres, responded. These represented 82% of centres that treated higher numbers of patients. The effect of treatment on fertility was known by 78% of those who responded, with 76% admitting not knowing any guideline on fertility in children or adolescents. As for the ideal time and place to inform the patient and/or family, only 14% thought it should be done in the same cancer diagnosis interview. In clinical practice, 12% of those surveyed never referred patients to Human Reproduction Units, another 12% only did so if the patients showed interest, and 38% only refer patients in puberty. Just over one-third (34%) of those referrals were going to receive highly gonadotoxic treatment.
ConclusionsThere are clear differences between pre-puberty and puberty patients. The frequency with which some method of fertility preservation is performed in patients is low. All respondents believe that the existence of national guidelines on the matter would be of interest.
Los riesgos de infertilidad en cáncer infantil, en función de la radioterapia, quimioterapia y/o cirugía son bien conocidos. La implicación de los profesionales y los avances en los métodos de preservación son cada vez mayores. Sin embargo, muchos pacientes no reciben información ni realizan ningún método de preservación.
MaterialSe realiza una encuesta nacional de 22 preguntas a especialistas en hematología y/o oncología infantil para valorar sus conocimientos, la posibilidad de realizar preservación en sus centros y la práctica habitual.
ResultadosRespondieron 50 miembros de la Sociedad Española de Hematología y Oncología Pediátrica, que representan 24 de 43 centros. Están representados el 82% de los centros que tratan un mayor número de pacientes. El 78% de los encuestados refiere conocer los efectos sobre la fertilidad de los tratamientos. El 76% admite no conocer ninguna guía sobre fertilidad en niños y adolescentes. En cuanto al momento para informar al paciente y/o su familia solo un 14% opina que debe hacerse en la entrevista del diagnóstico del cáncer. En su práctica clínica el 12% de los encuestados nunca deriva pacientes a las unidades de reproducción humana. Otro 12% solo lo hace si los afectados demuestran interés. El 38% deriva solo a pacientes púberes. El 34% remite a aquellos que vayan a recibir tratamiento altamente gonadotóxico.
ConclusionesUn gran porcentaje de especialistas manifiestan su falta de conocimientos y el valor de guías clínicas al respecto. Existen claras diferencias en preservación entre pacientes púberes y prepúberes. La frecuencia de preservación es baja.
Advances in cancer treatment for children and adolescents have improved overall survival rates in these patients. Future infertility is one of the potential long-term sequelae of many of these treatments. This complication is a source of stress for cancer survivors and impacts their quality of life.1–3
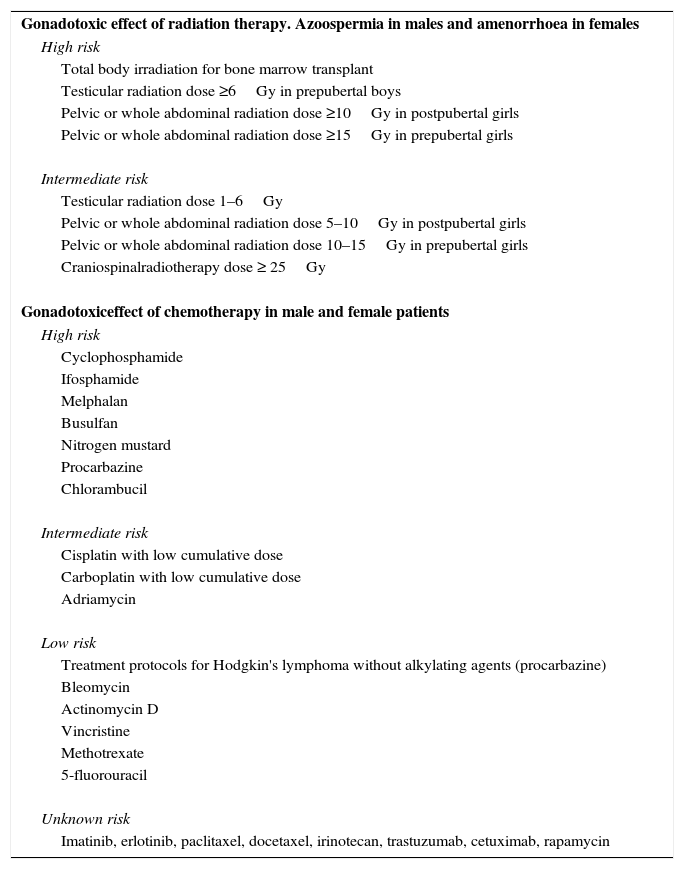
The estimated risks of gonadal dysfunction in both sexes based on the use of radiation therapy, chemotherapy and/or surgery have been studied thoroughly and recorded in multiple publications and guidelines developed by various medical organisations: the American Society of Clinical Oncology, the American Society for Reproductive Medicine and the National Comprehensive Cancer Network, among others (Table 1).1,4–8
Risk of sterility secondary to chemotherapy and/or radiotherapy.
| Gonadotoxic effect of radiation therapy. Azoospermia in males and amenorrhoea in females |
| High risk |
| Total body irradiation for bone marrow transplant |
| Testicular radiation dose ≥6Gy in prepubertal boys |
| Pelvic or whole abdominal radiation dose ≥10Gy in postpubertal girls |
| Pelvic or whole abdominal radiation dose ≥15Gy in prepubertal girls |
| Intermediate risk |
| Testicular radiation dose 1–6Gy |
| Pelvic or whole abdominal radiation dose 5–10Gy in postpubertal girls |
| Pelvic or whole abdominal radiation dose 10–15Gy in prepubertal girls |
| Craniospinalradiotherapy dose ≥ 25Gy |
| Gonadotoxiceffect of chemotherapy in male and female patients |
| High risk |
| Cyclophosphamide |
| Ifosphamide |
| Melphalan |
| Busulfan |
| Nitrogen mustard |
| Procarbazine |
| Chlorambucil |
| Intermediate risk |
| Cisplatin with low cumulative dose |
| Carboplatin with low cumulative dose |
| Adriamycin |
| Low risk |
| Treatment protocols for Hodgkin's lymphoma without alkylating agents (procarbazine) |
| Bleomycin |
| Actinomycin D |
| Vincristine |
| Methotrexate |
| 5-fluorouracil |
| Unknown risk |
| Imatinib, erlotinib, paclitaxel, docetaxel, irinotecan, trastuzumab, cetuximab, rapamycin |
The involvement of health professionals in fertility preservation in cancer patients is growing steadily, as are the advances in the different methods of preservation.9–13 For paediatric cancer patients, both radiation and chemotherapy with alkylating agents are particularly gonadotoxic, affecting oocytes and spermatogenesis.3,14–16
Semen cryopreservation is the approved method for male patients in Spain. In prepubertal male patients, currently available therapies are still experimental, and consist in the preservation of testicular tissue for future retransplantation. To date, there are no published reports of patients that have achieved fertility through this method.9,11,12,14,16,17
In women, embryo and oocyte cryopreservation are methods that are approved and available in Spain for postpubertal female patients since 2013. At present, ovarian stimulation can be performed in any phase of the cycle, which reduces delays in the initiation of cancer treatment. In girls and prepubertal adolescents, ovarian tissue cryopreservation is considered an experimental method. The immediacy of this method and the possibility of retrieving multiple follicles and oocytes are its main advantages. This approach employs laparoscopy. At least 40 cases of babies born following the use of this method have been reported in the literature.10,13,14,18
Despite all of the above, a considerable proportion of patients and their families are not given any information or the chance to pursue fertility preservation. Between 30% and 60% of cancer survivors in the United States and the United Kingdom have not been informed on the subject by the different providers in charge of their care.19,20 No data are available for Spain.
The aim of this study was to assess the concern and level of knowledge of paediatric oncologists and haematologists regarding infertility in cancer patients, the resources available in public and private hospitals in Spain that offer fertility preservation services to children and adolescents, and the need for information, training or the development of national guidelines on the subject.
Materials and methodsAfter performing an exhaustive literature review, we developed a survey based on clinical practice guidelines on fertility to explore different issues regarding the information and services on fertility preservation for children and adolescents. The survey targeted paediatricians specialised in haematology and/or oncology. It was developed by the Committee on Adolescents of the Spanish Society of Paediatric Haematology and Oncology (Sociedad Española de Hematología y Oncología Pediátrica [SEHOP]) and submitted from the administrative department of the SEHOP to two hundred of its members, followed by a reminder one month after sending the survey.
The survey consisted of 22 items. It can be consulted at the following address: https://docs.google.com/forms/d/1hVAe7_Q9F3O6asj5hZ5nkVHHWua3Daw2S_PfVb6vOHg/edit#.
We conducted a cross-sectional descriptive study in three parts. In the first, we analysed the importance that health professionals place on this issue, in the second, we assessed their knowledge on fertility, and in the last one, we assessed current clinical practice.
Statistical analysisWe have described categorical variables as frequencies and percentages for each category, and compared them by means of Pearson's chi squared test when the necessary assumptions were met, and otherwise by Fisher's exact test. We set the level of statistical significance at P≤.05. All calculations were performed using the Epidate statistical software version 3.1.
ResultsThe overall response rate was 25%: 50 of the total of 200 surveyed members of the SEHOP.
Analysis by institutionOf the 50 responses, nine did not specify the institution, and were therefore excluded from the analysis to avoid the unwitting duplication of responses from a single institution. Therefore, the final analysis included 41 responses corresponding to a total of 24 hospitals (median, 2 responses/centre; range, 1–3). When we analysed the results by institution, we only took into account one response for each hospital. For hospitals for which we had received more than one response, we integrated the answers into a single response for each. In most cases the answers were similar, but if we found small discrepancies in the number of patients, we used the mean of the different values. This may have been a source of bias in the results, but no greater than expected in this type of survey.
Twenty-four hospitals of a total of 43 submitted the completed survey (56% response rate). When we made the analysis by the number of new cases per year (using data from the SEHOP), the response rate for hospitals managing 25 or more new cases per year was 82% (14/17) compared to 38% of hospitals managing fewer than 25 new cases per year (10/26) (P=.005).
Eighty-five percent of the hospitals that submitted responses to the survey had a reproductive health unit, while thirteen percent did not.
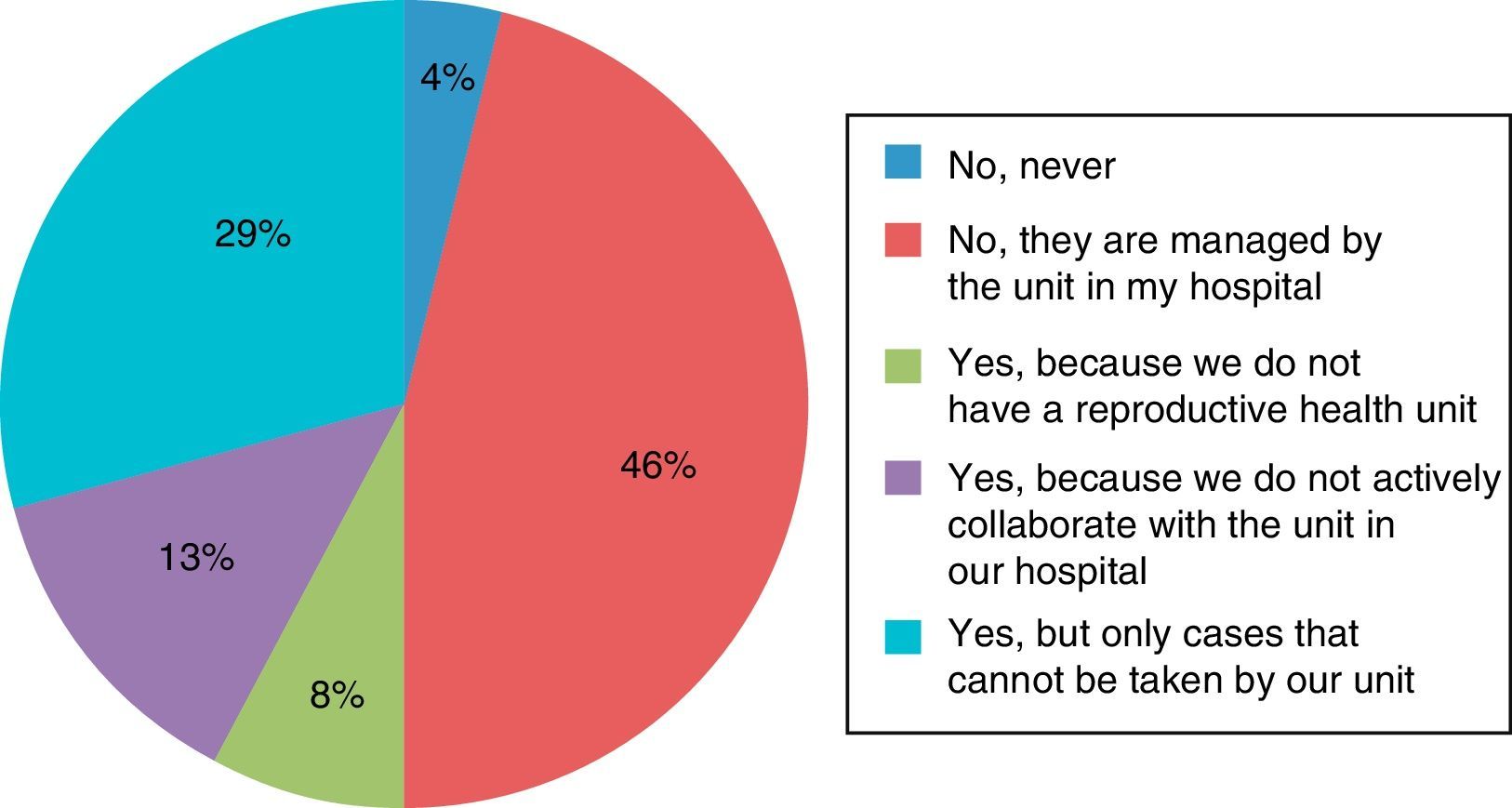
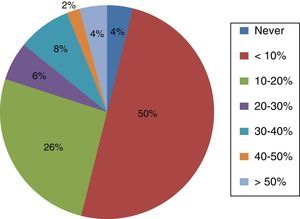
Fig. 1 summarises the answers to the question regarding the referral of patients to reproductive health units for fertility preservation.
In answer to the question “Assuming the absence of a reproductive health unit, would you consider having online or telephonic access to a referral hospital for consultation on your cases important?” all hospitals without a reproductive health unit3 and most hospitals with a reproductive health unit (16/21) said yes.
Analysis by specialty of respondentsSince some of the questions in the survey may have elicited personal opinions rather than institutional positions, we analysed the rest of the questions individually. For this part, we also included the nine responses that had been excluded from the analysis by institution.
Of all respondents, thirty-eight percent were aged 30–39 years, twenty-seven percent 40–49 years, thirty-two percent 50–59 years, and only three percent more than 60 years.
Questions 5 and 6 addressed the interest of clinicians and families regarding fertility. Every respondent stated that they considered it an important subject that had to be discussed with patients and/or their parents. Furthermore, eighty percent (40/50) of respondents reported perceiving an interest in the patients and/or their families, six percent not perceiving an interest on the part of the families, and fourteen percent that they did not know.
Thirty-eight out of fifty respondents (76%) admitted knowing of any guidelines on fertility for children, adolescents and/or young adults with cancer.
When we compared the extent to which clinicians were knowledgeable of the methods approved in Spain for fertility preservation, only 28% (6/50) of respondents reported knowing the methods approved for prepubertal patients, while 50% (25/25) knew the methods approved for postpubertal patients (P=.02).
Seventy-eight percent of respondents (39/50) knew the impact on fertility of the different chemotherapy and radiation treatments, while 32% (16/50) reported needing to update their knowledge.
The last part of the survey explored current clinical practice in paediatric haematology and oncology units. Thirty-two percent of respondents (16/50) believed that information on fertility was not restricted to the scope of paediatricians and could be provided by other health professionals (psychologists, nurses, gynaecologists, radiation therapists), while 54% (27/50) believed this fell within the scope of paediatric haematologists and oncologists, and 6% that this is the task of gynaecologists specialised in reproductive health. The rest of respondents did not answer this question.
When asked about the best time to inform the patient and/or family, 14% (7/50) responded that fertility should be discussed at the time of cancer diagnosis. Eighty-two percent (41/50) responded that it should be discussed as early as possible, but at a different time. Four percent (2/50) believed it should be addressed at a different time and without hurry.
When it came to their clinical practice, six respondents (12%) reported never referring patients to reproductive health units. Another 12% (6/50) referred patients only if they or their families seem to be interested in it. Thirty-eight percent (19/50) only referred postpubertal patients. Thirty-four percent (17/50) referred patients that were going to received highly gonadotoxic treatments. Four respondents did not answer.
As for the treatment that respondents recommended for postpubertal males, 96% (48/50) recommended sperm banking and the remaining 4% (2/50) did not recommend any. This was reversed for prepubertal patients: 96% (48/50) did not recommend any method, and 4% (2/50) testicular tissue cryopreservation.
For postpubertal female patients, 20% (10/50) recommended no preservation methods, 40% (20/50) favoured oocyte cryopreservation orvitrification, 36% (18/50) recommended ovarian tissue cryopreservation, and one respondent answered that this judgement should be made by the reproductive health unit. For prepubertal female patients, 60% of the specialists (30/50) thought no method should be used, 36% (18/50) recommended ovarian tissue cryopreservation, and the rest oocyte vitrification.
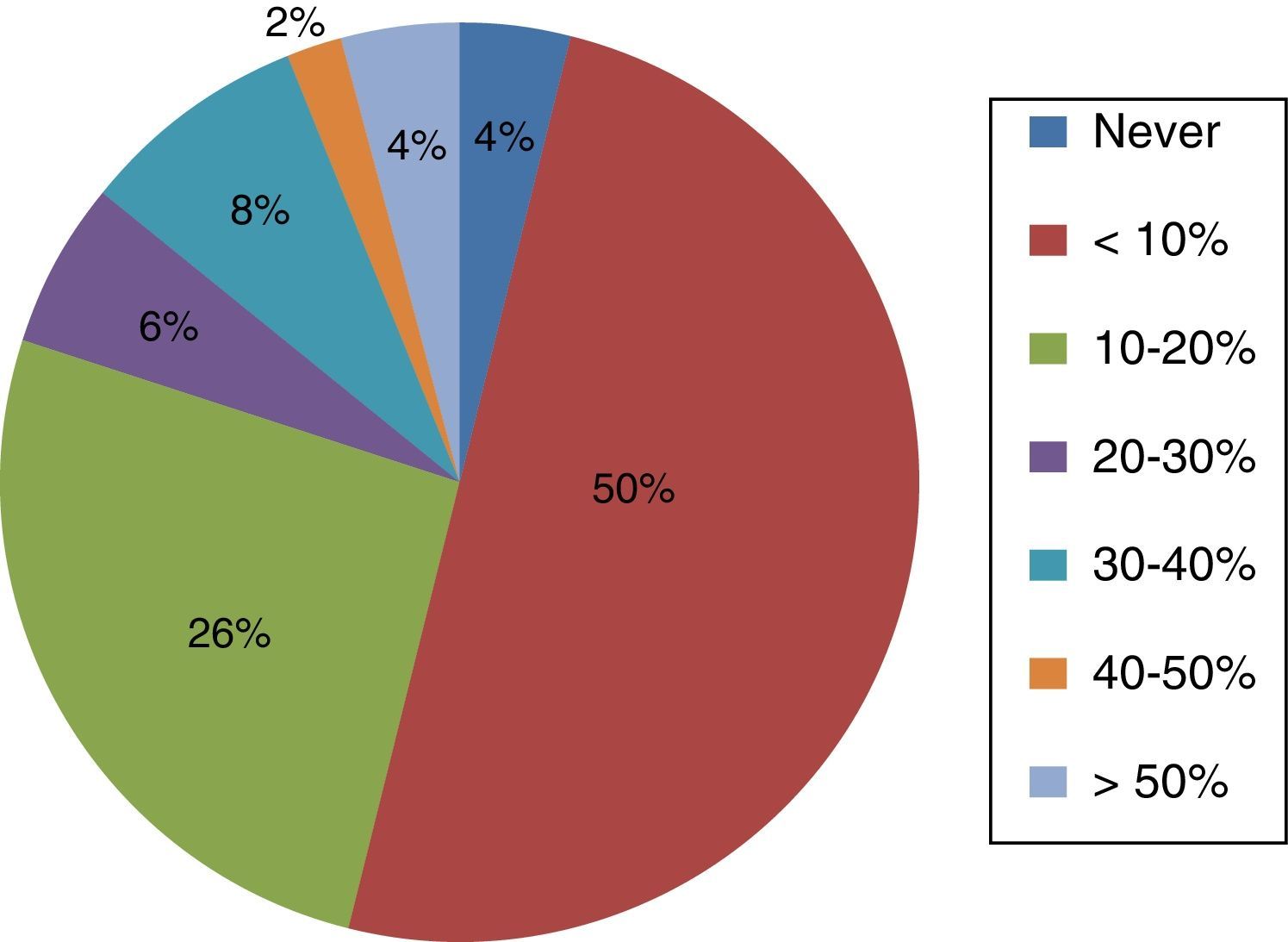
The actual proportion of patients that undergo some type of fertility preservation is very low, and half of the surveyed hospitals reported using these methods in fewer than 10% of patients, as Fig. 2 shows.
Last of all, all paediatricians (50/50, 100% of respondents) considered that it would be very useful to have a clinical guideline on fertility developed and updated through the SEHOP for consultation, provided that adherence to it was not mandatory.
DiscussionBased on the national tumour register in Spain, 43 public and private hospitals provide care for paediatric cancer patients. There have been considerable advances in the treatment and management of cancer in the past few decades that have led to current survival reaching an overall cure rate of approximately 70%.21 This increase in survival entails an increase in the number of individuals at risk of experiencing late side effects. One of the side effects that may result from surgery or the toxicity of chemotherapy and/or radiation is infertility. The approach to fertility preservation appears to be a secondary concern for most paediatric oncologists and haematologists, as reflected by the results of this survey, to which many hospitals did not respond. Most responses came from the hospitals serving the largest numbers of patients. This preoccupation with offering the best possible cancer treatment to the patient while deferring considerations of future fertility has been described extensively in the literature.2,22,23
There also seem to be multiple factors at play in the scarcity of the information provided to paediatric patients compared to adult ones.23,24 The main health provider-related barrier identified in our survey was a lack of knowledge on the subject: while 78% reported knowing the effects of chemotherapy and/or radiation on fertility, only 24% knew of at least one up-to-date guideline on fertility preservation in these patients. The same problem has been reported in other countries.25,26
When we compared how well clinicians were acquainted with fertility preservation methods approved in Spain (semen collection and oocyte preservation) compared to experimental methods (testicular or ovarian cortex tissue cryopreservation), 50% reported knowing the methods used in postpubertal patients, compared to 28% that knew methods used in prepubertal patients. Ninety-six percent recommended semen cryopreservation in postpubertal patients, and only 5% recommended testicular tissue cryopreservation in prepubertal patients. When it came to female patients, 20% did not recommend any method in postpubertal patients, and the percentage rose to 60% for prepubertal patients. Last of all, 38% of respondents reported referring only postpubertal patients to reproductive health units. This discrepancy in the data has also been reported in publications outside of Spain. A survey conducted in the United Kingdom found that while 73% of paediatric oncologists agreed that all postpubertal female patients should be referred to reproductive health units, only 20% eventually access those services.25 Furthermore, 30% to 60% of cancer survivors in the United Kingdom and the United States reported receiving no information regarding fertility prior to initiating cancer treatment.12,27 Fewer than 10% of patients end up undergoing fertility preservation before initiating chemotherapy in 50% of Spanish hospitals, which does not seem to be consistent with other answers, such as the interest of patients and their families to preserve fertility perceived by 80% of respondents. Similarly, based on the existence of a reproductive health unit in 21 hospitals and the ease with which patients can be referred to tertiary care hospitals in Spain, one would expect a higher rate of fertility preservation.
While 54% of respondents considered that paediatric oncology and haematology specialists were responsible for informing the patient on fertility preservation options, the survey did not explore other variables that cannot but influence the attitudes of clinicians towards providing this information, such as the patient's chance of survival, delays in treatment initiation, associated costs, and ethical concerns.28
Furthermore, the survey did not assess factors that influence decision-making in children and their families. The literature reflects the complexity of this process due to the inability of the child—in most cases—to understand the repercussions of fertility preservation. Furthermore, parents are put in the position of having to consider their children's future desire to reproduce at a very difficult time when they are confronted with a cancer diagnosis. The quality of the information received and the pressure of the doctor to initiate cancer treatment are the factors that most influence the final decision of families and patients.29,30
The current clinical guidelines recommend discussing fertility preservation with all cancer patients as early as possible, including experimental methods used in children.7,31,32
Despite the bias that may result from the low percentage of clinicians that responded to the survey, its results seem to suggest a few important conclusions: the first is that clinicians seem not to be greatly concerned with this subject based on the low number of responses received, and that at present, a large part of paediatric cancer patients in Spain do not receive accurate and necessary information on the risk of infertility associated with their cancer treatment; the second is that these patients should be given access to facilities that perform the fertility preservation techniques currently available, so that they can benefit from them in the future should they be unable to reproduce without assistance. The third is that the availability of information or national guidelines would be very helpful to health professionals and patients. The SEHOP Committee on Adolescents with cancer considers these three aspects priority objectives, and commits to continue working to advance the quality of paediatric cancer treatments.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Garrido-Colino C, Lassaletta A, Vazquez MÁ, Echevarria A, Gutierrez I, Andión M, et al. Situación de la preservación de fertilidad en pacientes con cáncer en nuestro medio: grado de conocimiento, información e implicación de los profesionales. An Pediatr (Barc). 2017;87:3–8.