Pain anxiety is a psychological component that can regulate and modulate the experience of pain in children and adolescents. It can also have an impact on the outcomes of surgical procedures, chronic pain management and psychological interventions. The aim of our study was to translate the Child Pain Anxiety Symptoms Scale (CPASS) into Spanish and assess the psychometric properties of the Spanish version.
Patients and methodsFirst, the CPASS was translated according to international guidelines. Secondly, to assess the psychometric properties of the translated version, we conducted an analysis in a paediatric sample. A total of 160 children, 49.37% female, with a mean age of 14.5 years (SD, 2.3; range, 8−18 years) completed pain catastrophising, health-related quality of life, pain interference and pain intensity scales. We assessed the following psychometric properties: construct validity (exploratory and confirmatory factor analysis), internal consistency, floor and ceiling effects and convergent validity (correlation of CPASS to the other completed questionnaires completed and with objective aspects of the health history).
ResultsIn the exploratory factor analysis, the final 18-item version (having excluded items 18 and 19) of the CPASS was the best fit, with all items included in the hypothetical construct and exhibiting optimal factor loadings. The confirmatory factor analysis showed that the final 18-item, 4-factor model was adequate for the scale structure. We did not detect any floor or ceiling effects in the final version. Lastly, the results confirmed that the Spanish version has good internal consistency (Cronbach α, 0.88) and an adequate convergent validity.
ConclusionThe Spanish CPASS exhibits good psychometric proprieties and it can be used to assess pain anxiety in the paediatric population.
La ansiedad relacionada con el dolor es un componente psicológico que es capaz de regular y modificar la experiencia de dolor en niños y adolescentes. Además, puede modificar el éxito del tratamiento en procedimientos quirúrgicos, dolor crónico e intervenciones psicológicas. El objetivo de este estudio fue traducir al español la Child Pain Anxiety Symptoms Scale (CPASS) y analizar sus propiedades psicométricas.
Pacientes y métodosEn primer lugar, la CPASS se tradujo al español de acuerdo con las recomendaciones internacionales. En segundo lugar, para evaluar las propiedades psicométricas de la CPASS, se analizó una muestra pediátrica. 160 niños (mujeres = 49,37%; edad media = 14,5 ± 2,3 [8−18 años]) completaron cuestionarios de catastrofismo relacionado con el dolor, calidad de vida relacionada con la salud, interferencia del dolor e intensidad del dolor. Se evaluaron las siguientes propiedades psicométricas: validez de constructo (análisis factorial exploratorio y confirmatorio), consistencia interna, efecto suelo/techo y validez convergente (relación del CPASS con el resto de los cuestionarios cumplimentados y con aspectos objetivos de la historia clínica).
ResultadosEn el análisis factorial exploratorio, la versión final de 18 ítems (sin los ítems 18 y 19) de la CPASS fue la que mejor se ajustó, con todos los ítems incluidos en el factor teórico supuesto y mostrando una carga factorial óptima. El análisis factorial confirmatorio mostró que la versión final de 18 ítems incluidos en 4 factores es un modelo adecuado para la estructura de la escala. No se detectaron efectos suelo o techo en la versión final. Finalmente, los resultados confirman que la versión española presenta una buena consistencia interna (coeficiente alfa de Cronbach = 0,88) y una validez convergente adecuada.
ConclusionesLa versión española de la CPASS muestra buenas propiedades psicométricas y puede ser utilizada para evaluar la ansiedad por dolor en la población pediátrica.
Pain is a serious problem that affects millions of children and adolescents around the world, with a considerable impact on quality of life.1,2 The emotional component of pain plays an important role in its regulation and development. The emotional factors involved in pain have been studied extensively, and there is evidence that their modification and treatment can reduce pain, thereby decreasing its impact on daily life and improving quality of life.3–6
Pain-related anxiety refers to the thoughts, feelings, behaviours and physical sensations that accompany the experience and anticipation of pain.7 It manifests through (a) cognitive responses to pain, which can lead to difficulty performing cognitive tasks such as concentrating or paying attention; (b) emotional reactions, the most frequent of which is fear of experiencing sensations associated with pain or its intensification; (c) physiological responses in the form of somatic symptoms, such as increased muscle tension, heart rate or breathing rate; and (d) behavioural responses by which efforts are made to reduce or avoid pain. Anxiety is a psychological factor that, in addition to being present in chronic pain, also plays an essential role in stressful acute situations such as surgeries or painful procedures, in which it has been found to have the potential to affect patient outcomes and recovery.6,8
A growing body of research has not only yielded knowledge about these factors, but also tools for their diagnosis and assessment.9 When it comes to pain-related anxiety, in 2010, Pagé et al.10 developed the Child Pain Anxiety Symptoms Scale (CPASS) by modifying the 20-item Pain Anxiety Symptoms Scale (PASS-20) for adults. This initial psychometric study10 was followed by a second one in a sample of surgical patients, and the scale is now widely used for evaluating pain-related anxiety in children and adolescents.11 In Spain, the 25-item Patient Reported Outcomes Measurement Information System (PROMIS) paediatric self-report scale,12 which includes a specific subscale on anxiety, is one of the scales frequently used to assess paediatric pain-related anxiety.13 However, this subscale has only 4 items, so it does not assess the different factors that may contribute to pain-related anxiety comprehensively. In contrast, the CPASS includes 4 different domains aimed at assessing pain-related anxiety from different perspectives. Although its use is widespread, to our knowledge it has not been translated and adapted into Spanish. A Spanish version could increase and improve our knowledge of pain-related anxiety, and therefore of the role of psychological factors in paediatric and adolescent pain.
The aims of this study were to translate the CPASS to Spanish and to evaluate its psychometric characteristics (construct validity, internal consistency, floor/ceiling effects and convergent validity) in a paediatric sample in Spain.
MethodsThe study was approved by the Ethics Committee of the universitary hospital 12 de Octubre and adhered to the principles of the Declaration of Helsinki. The article was written according to the Standards for Reporting Diagnostic Accuracy Studies (STARD).14
ParticipantsChildren and adolescents (aged 8–18 years) managed in a paediatric surgery clinic in a tertiary care hospital were informed of the possibility of participating in this study before undergoing surgery. The study included paediatric surgical patients (see Table 1) with an American Society of Anesthesiologists (ASA) Physical Status Classification15 of 3 or less, thus excluding patients with severe disease or requiring urgent surgery. We obtain the assent of children (age < 12 years) as well as the consent of the parents or guardians and of adolescent participants as an inclusion criterion. Participants had to have good Spanish speaking and reading skills. Patients were excluded if they had a developmental (not related to movement) or cognitive delay or intellectual disability.
Anthropometric and sociodemographic characteristics of the children and their parents/guardians (n = 160).
| Mean ± SD or n (%) | Range (min-max) | |
|---|---|---|
| Patient age (years) | 14.5 ± 2.3 | 8−18 |
| Patient sex (male: female) | 81 (50.62%): 79 (49.37%) | |
| Patient height (cm) | 164.57 ± 20.52 | 100−190 |
| Patient height (kg) | 61.74 ± 25.23 | 23−121 |
| Educational attainment of patient | ||
| Primary education | 63 (38.37%) | |
| Secondary school/high school | 87 (54.37%) | |
| Vocational training | 10 (6.25%) | |
| Previous surgeries | 0.9 ± 1.26 | 0−18 |
| Prior surgery | ||
| No | 99 (61.87%) | |
| Yes | 61 (38.13%) | |
| Number of previous surgeries | ||
| 1−3 | 53 (86.88%) | |
| 3−6 | 6 (9.83%) | |
| >6 | 2 (3.26%) | |
| Type of disease and surgery | ||
| Urology | 43 (26.87%) | |
| Maxillofacial | 16 (10%) | |
| Plastic surgery | 25 (15.62%) | |
| Otorhinolaryngology | 32 (20%) | |
| Pneumology | 10 (6.25%) | |
| Neurology | 3 (1.87) | |
| Traumatology | 16 (10%) | |
| Cardiac | 10 (6.25%) | |
| Ophthalmology | 5 (3.12%) | |
| Medical consultations in the last year | ||
| 1−3 | 66 (41.2%) | |
| 4−6 | 50 (31.2%) | |
| 7−10 | 27 (16.8%) | |
| 11−14 | 12 (7.5%) | |
| 15−20 | 2 (1.2%) | |
| >20 | 3 (1.8%) | |
| Parent/guardian age (years) | 45.62 ± 7.1 | 24−57 |
| Parent/guardian sex (male: female) | 30 (18.75%):130 (81.25%) | |
| Parental educational attainment | ||
| Primary education | 19 (11.87%) | |
| Secondary education | 50 (31.25%) | |
| Vocational training | 45 (28.12%) | |
| University education | 46 (28.75%) | |
| Family socioeconomic status | ||
| Low | 64 (39.3%) | |
| Middle | 93 (58.12%) | |
| High | 3 (1.8%) |
SD, standard deviation.
The CPASS is a 20-item self-administered scale through which children and adolescents aged 8–18 years self-report the level of their anxiety symptoms when in pain.10 The answers range from 0 (never think, act, or feel that way) to 5 (always think, act, or feel that way). The CPASS has 4 dimensions: cognitive (eg, “I cannot think straight or think clearly when I feel pain”); physiological anxiety (eg, “When I feel pain, my heart beats faster”); fear (eg, “When I feel pain I am afraid that something terrible will happen”); and escape and avoidance (eg, “I will stop any activity when I start feeling pain”). The CPASS has demonstrated an excellent internal consistency (ranging from 0.90 to 0.92) and item-total correlations (ranging from 0.20 to 0.70) in various paediatric samples. Previous studies have found moderate correlations between the CPASS and pain-related catastrophising, and positive correlations with pain intensity and functional disability.10,11,16
Pain intensityWe used the Faces Pain Scale-Revised17 to assess pain intensity in participants. The FPS-R is a self-report scale in which the child or adolescent indicates the intensity of the pain they experience by choosing the appropriate facial expression corresponding to it, and the scores range from 0 (“no pain”) to 10 (“a lot of pain”).
The parents or guardians reported the pain intensity perceived in their children with the Parent’s Postoperative Pain Measure (PPPM).18 The scale comprises 15 items through which parents rate their child’s pain based on behaviours and attitudes related to pain.
Health-related quality of lifeTo asses health-related quality of life (HRQoL), we used the Spanish version of the 23-item Pediatric Quality of Life Inventory 4.0 Generic Core Scales (PedsQL).19 This instrument is composed of parallel scales: 1) Child self-report scale; and 2) Parent proxy-report scale. The internal consistency of both scales in this study was adequate (Cronbach α of 0.90 for the child self-report scale and 0.92 for the parent proxy-report scale).
Pain interferenceTo assess pain interference, we used the Spanish version of Patient-Reported Outcomes Measurement Information System-Pediatric Pain Interference scale (PROMIS-PI).20 Is an 8-item self-report scale in which the child rates how pain interferes with daily life. In this study, the PROMIS-PI exhibited an adequate internal consistency (Cronbach α, 0.90).
Pain-related catastrophisingTo assess this variable, we used the Pain Catastrophizing Scale version for children (PCS-C).21 Through 13-items, the PCS-C evaluates catastrophic beliefs associated with the child’s experience of pain. In this study, the PCS-C showed an adequate internal consistency (Cronbach α, 0.89).
More information on the characteristics of these scales and their psychometric properties is available on Supplementary Document I.
Translation processThe CPASS was translated to Spanish in 3 steps, following international recommendations.22 First, it was translated from English to Spanish by 2 independent bilingual pain researchers, with a bilingual translator resolving discrepancies. Then, the Spanish version was back-translated to English by 2 native bilingual speakers. Lastly, a professional bilingual translator compared the Spanish version of the CPASS with the original version published by Pagé et al.10 The Spanish version of the CPASS can be found in Supplementary Document II.
ProcedureAt hospital admission, all children who were going to undergo surgery and their parents were invited to participate in the study. In a 45-minute interview, an independent researcher informed them in detail about the study. Those interested in participating completed an informed consent form. The assent of children (<12 years) as well as the consent of the parents/guardians and adolescents (through signing the informed consent) was a prerequisite for participation in the study. Parents and children were then asked to fill out paper questionnaires. It is important to note that both the patient and the parent/guardian had to fill out the entire questionnaire (child version for the patient, parent version for the parents) to be included in the study. Thus, if either the patient or the parent did not complete any questionnaire or item, both patient and parent were excluded from the study. Subsequently, the nursing team measured the height and weight of the participants, and the researchers performed the anamnesis.
Statistical analysisThe software packages SPSS, version 21 (IBM SPSS Statistics) and Mplus, version 7.11 were used to conduct all the statistical analyses. We set the level of statistical significance at 5% (P < .05).
Construct validityWe assessed construct validity in 2 steps. First, we conducted an exploratory factor analysis (EFA) to identify the optimal factor structure. Subsequently, we confirmed the theoretical factor structure through confirmatory factor analysis (CFA).
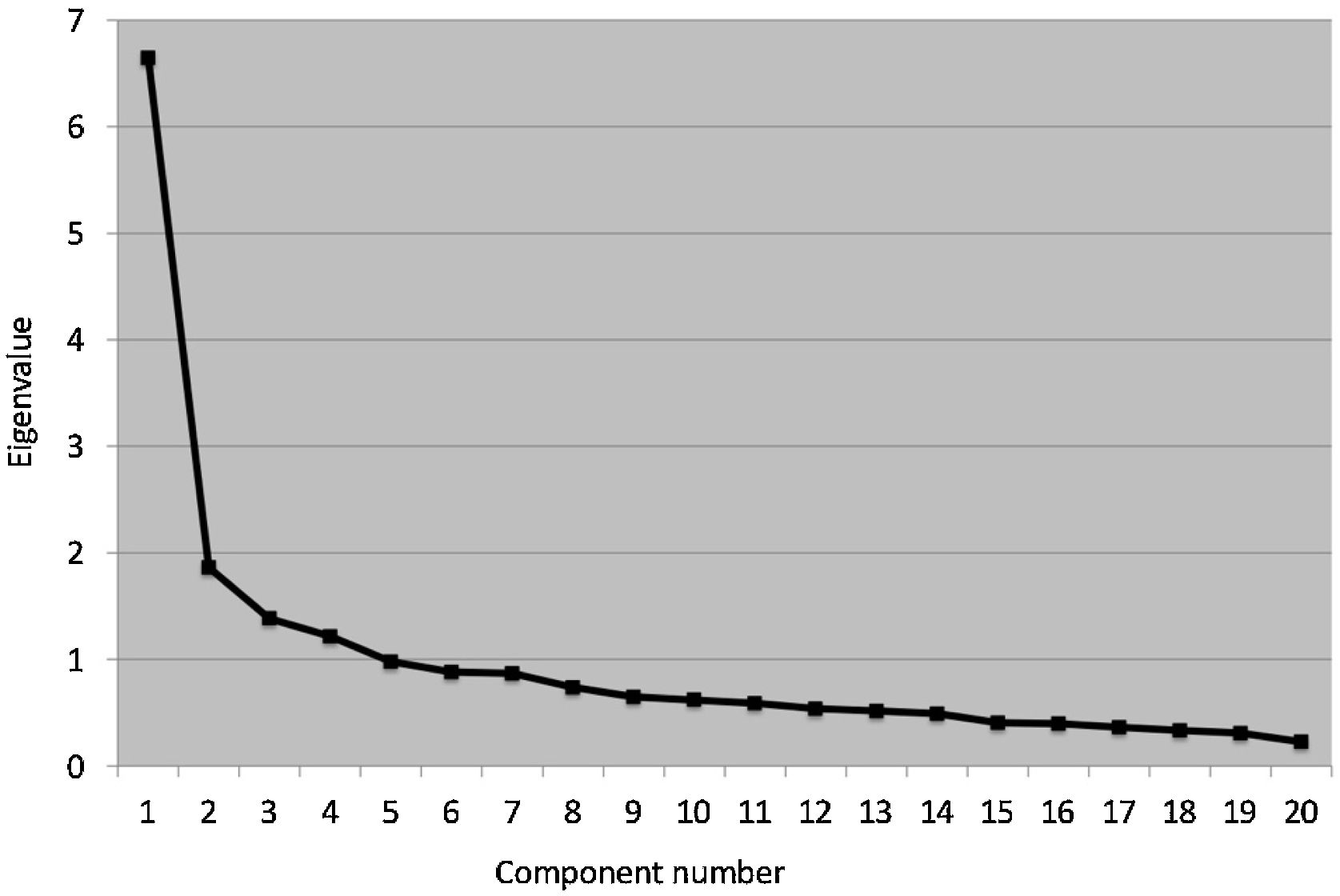
In EFA, to determine the suitability of the Pearson correlation matrix for factor analysis, we used the Barlett test of sphericity and the Kaiser-Meyer-Olkin (KMO) test.23 The optimal number of factors was established based on the Kaiser eigenvalue criterion (eigenvalue ≥ 1) and the scree plot.24 We used the principal axis method with oblique rotation for factor extraction. Items had to have a factor loading of 0.4 or greater to be included.
The CFA was performed with the robust maximum likelihood estimation method. We used the following measures to assess goodness of fit in both analyses (EFA and CFA): χ2 test, comparative fit index (CFI), Tucker Lewis index (TLI), standardised root mean residual (RMSR) and root mean square error of approximation (RMSEA). The model was considered to have a good fit if it met the criteria proposed by Hu and Bentler25 (TLI and CFI ≥ 0.95, SRMR and RMSEA ≤ 0.08). We also calculated modification indices to identify local areas of misspecification that could not be detected by the overall fit measures previously mentioned.26
Internal consistency, floor and ceiling effectsThe internal consistency of the Spanish version of the CPASS was assessed by means of the Cronbach α, with values greater than 0.70 considered acceptable.27 We defined the presence of a floor or ceiling effect as at least 15% of the patients having the lowest or highest possible score, respectively.28
Convergent validityThe convergent validity of the CPASS was analysed through the assessment of its association with the rest of the variables, including both objective aspects in the health history (medical visits and previous surgeries in the past year) and subjective aspects (perception of the child and parents/guardians) related to pain (FPS-R, PPPM, and PROMIS Pediatric Pain Interference scale), pain catastrophising (PCS-C) and HRQoL (PedsQL). We used the Pearson correlation coefficient to assess the strength of these correlations: strong (>0.60), moderate (0.30−0.60), and weak (<0.30).28
ResultsBetween January and March of 2021, 190 potential participants were invited to participate in the study (Supplementary Document III, flow chart of sample selection). A total of 160 children and adolescents were included in the study, of who 49.37% were female (81 male, 79 female), with a mean age of 14.5 years (standard deviation [SD], 2.3). Table 1 presents the anthropometric and sociodemographic characteristics of the children and the parents/guardians that participated in the study.
Exploratory factor analysisBefore performing the exploratory factor analysis, we calculated the Cronbach α coefficient for the whole scale (α = .88) and the adjusted item-total correlations (average item-total correlation, 0.51). No items were removed, given that all contributed substantially to the scale. The KMO test showed that the data were suitable for factor analysis (KMO = .87), and the Bartlett test rejected the identity matrix null hypothesis: χ2 (190) = 1168.40 (P < .001). Based on these results, it was justified to proceed with the EFA. Applying the Kaiser criteria, we kept 4 factors, which accounted for 57.61% of the variance (Fig. 1). However, the preliminary EFA revealed the presence of 2 problematic items. Specifically, item 18 had a factor loading of less than 0.40, and item 19 had a significant and similar factor loading in 2 factors other than the factor initially expected based on the theoretical model (0.41 for the fear construct; 0.40 for the escape/avoidance construct). For these reasons, we decided to eliminate both items from the model. The resulting final 4-factor model (18 items) fit the data well. Table 2 presents the goodness-of-fit indices of the model and the factor loadings of each item.
Final solution of the exploratory factor analysis.
| Goodness of fit | ||||
|---|---|---|---|---|
| χ2 = 111.90, P = .040; CFI = 0.97; TLI = 0.95; SRMR = 0.03; RMSEA = 0.04; 95% CI 0.01–0.06 | ||||
| Item | Fear | Physiological Anxiety | Cognitive | Escape/Avoidance |
| 1. Pienso que si mi dolor es demasiado intenso, nunca mejorará. | 0.63* | – | – | – |
| I think that if my pain hurts too much, it will never get better. | ||||
| 2. Cuando tengo dolor, tengo miedo de que algo horrible pase. | 0.61* | – | – | – |
| When I feel pain, I am afraid that something terrible will happen. | ||||
| 3. Cuando tengo mucho dolor, descanso tan pronto como puedo. | – | – | – | 0.49* |
| I rest right away when my pain hurts too much. | ||||
| 4. Mi cuerpo empieza a temblar cuando hago alguna actividad que empeora mi dolor. | – | 0.69* | – | – |
| My body starts to shake when I am doing an activity that makes my pain worse. | ||||
| 5. No puedo pensar con claridad cuando tengo dolor. | – | – | 0.69* | – |
| I can’t think straight or think clearly when I feel pain. | ||||
| 6. Paro cualquier actividad cuando empiezo a sentir dolor. | – | – | – | 0.70* |
| I will stop any activity when I start feeling pain. | ||||
| 7. Cuando tengo dolor, mi corazón late más rápido. | – | 0.65* | – | – |
| When I feel pain, my heart beats faster. | ||||
| 8. Tan pronto como el dolor empieza, pido a mis padres que me den medicación. | – | – | – | 0.54* |
| As soon as pain begins, I ask my parents for medication. | ||||
| 9. Cuando tengo dolor, pienso que podría estar muy enfermo. | 0.62* | – | – | – |
| When I feel pain I think I might be really sick. | ||||
| 10. Cuando tengo dolor me es muy difícil pensar en cualquier otra cosa. | – | – | 0.51* | – |
| When I feel pain, it is hard for me to think about anything else. | ||||
| 11. Cuando tengo dolor, no hago algunas actividades importantes. | – | – | – | 0.45* |
| I don’t do important activities when I hurt. | ||||
| 12. Cuando tengo dolor, me siento mareado y/o débil. | – | 0.52* | – | – |
| When I feel pain, I feel dizzy or faint. | ||||
| 13. Tener dolor me asusta mucho. | 0.53* | – | – | – |
| Feeling pain is very scary. | ||||
| 14. Cuando tengo dolor, pienso en él todo el rato. | – | – | 0.66* | – |
| When I feel pain, I think about it all the time. | ||||
| 15. Cuando tengo dolor, siento ganas de vomitar. | – | 0.59* | – | – |
| When I feel pain, I feel like I am going to throw up. | ||||
| 16. Cuando me duele mucho, pienso que no seré capaz de volver a moverme. | 0.63* | – | – | – |
| When my pain hurts too much I think I might not be able to move again. | ||||
| 17. Encuentro difícil concentrarme y prestar atención cuando tengo dolor. | – | – | 0.47* | – |
| I find it hard to concentrate and pay attention when I feel pain. | ||||
| 18. Me resulta difícil relajar mi cuerpo después de sentir dolor. | – | – | – | – |
| I find it hard to relax my body after I feel pain. | ||||
| 19. Me preocupo cuando tengo dolor. | – | – | – | – |
| I worry when I feel pain. | ||||
| 20. Intento no hacer aquellas actividades que me hacen sentir dolor. | – | – | – | 0.55* |
| I try not to do activities that make me feel pain. | ||||
CFI, comparative fit index; CI, confidence interval; RMSEA, root mean square error of approximation; RMSR, standardised root mean square residual; TLI, Tucker-Lewis index.
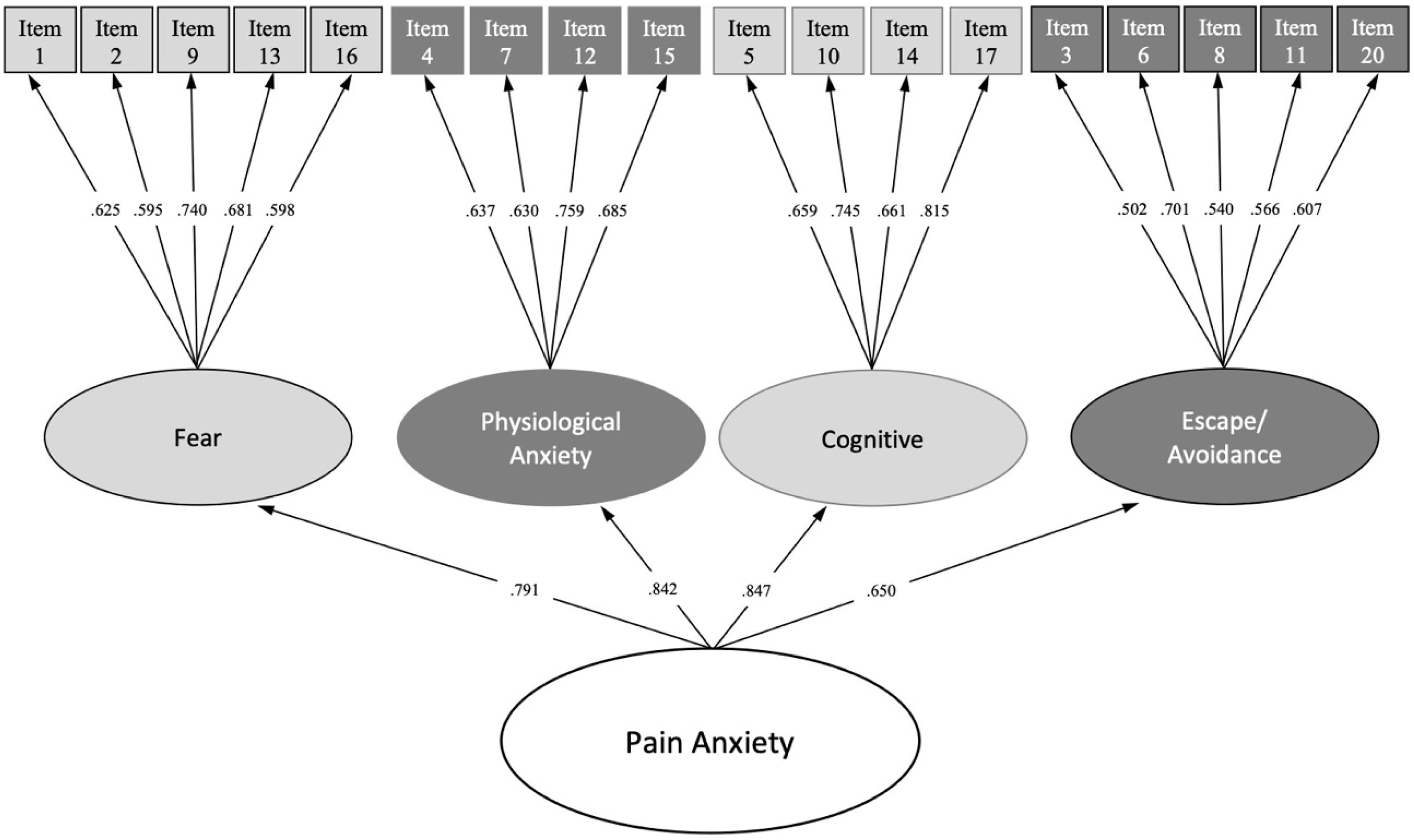
We performed a CFA of the original version and of the scale with the deleted items (see Table 3). The final 18-item version (without items 18 and 19) of the CPASS was the best fit, with all items fitting in the expected hypothetical construct and showing optimal factor loadings (>0.50). In addition, because there was a moderate-high correlation between the 4 CPASS factors (fear, physiological anxiety, cognitive, and escape/avoidance: r = 0.46–0.72; P < .001), we added a higher-order factor for a single unifying construct named pain anxiety. The higher-order 18-item 4-factor solution was a good fit for the data; thus, it was established in the final model: χ2 (131) = 150.56, P = .116; CFI = 0.97; TLI = 0.97; RMSEA = 0.03, 95% CI 0.001–0.05; SRMR = 0.06. Fig. 2 shows the standardised factor loadings of this final higher-order 18-item 4-factor solution.
Model fit in the confirmatory analysis of the CPASS.
| Model | χ2 (df) | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|
| 20-item | 207.50 (164) | 0.94 | 0.93 | 0.04 (0.02−0.06) | 0.06 |
| 19-item (without item 18) | 180.47 (146) | 0.95 | 0.94 | 0.04 (0.02−0.057) | 0.06 |
| 18-item (without items 18 and 19) | 144.66 (129) | 0.98 | 0.97 | 0.03 (0.001−0.05) | 0.05 |
CFI, comparative fit index; df, degrees of freedom; RMSEA, root mean square error of approximation; RMSR, standardised root mean square residual; TLI, Tucker-Lewis index.
The final Spanish version of the CPASS consisted of 18 items distributed across 4 dimensions (fear: 1, 2, 9, 13, and 16; physiological anxiety: 4, 7, 12, and 15; cognitive: 5, 10, 14, and 17; and escape/avoidance: 3, 6, 8, 11, and 20). All items had a direct and affirmative wording and were rated on a 5-point Likert scale (0–5), so the total score ranged from 0 to 90 points. Higher scores are indicative of higher levels of pain anxiety.
The internal consistency of the scale was acceptable (Cronbach α, 0.88), and its 4 dimensions had an internal consistency of 0.72 or greater (Table 4). No child obtained the highest possible score on the scale, and only 1.2% of the children obtained the lowest possible score. Thus, we did not identify floor or ceiling effects in the final Spanish version of the CPASS.
Internal consistency of the CPASS.
| CPASS | Mean ± SD | Adjusted item-to-total score correlation | Cronbach α if item was removed | Skewness | Kurtosis | Cronbach α (95% CI) | Composite reliability | AVE | |
|---|---|---|---|---|---|---|---|---|---|
| Subconstruct | Item | ||||||||
| Fear | 0.78 (0.73–0.83) | 0.78 | 0.43 | ||||||
| Item 1 | 0.90 ± 1.00 | 0.45 | 0.87 | 1.10 | 0.91 | ||||
| Item 2 | 1.43 ± 1.16 | 0.44 | 0.87 | 0.47 | −0.62 | ||||
| Item 9 | 1.10 ± 1.21 | 0.62 | 0.87 | 0.95 | 0.05 | ||||
| Item 13 | 1.40 ± 1.44 | 0.56 | 0.87 | 0.69 | −0.89 | ||||
| Item 16 | 0.62 ± 1.20 | 0.43 | 0.87 | 2.07 | 3.66 | ||||
| Physiological anxiety | 0.77 (0.71–0.83) | 0.77 | 0.47 | ||||||
| Item 4 | 0.99 ± 1.23 | 0.49 | 0.87 | 1.19 | 0.46 | ||||
| Item 7 | 1.59 ± 1.27 | 0.51 | 0.87 | 0.52 | −0.56 | ||||
| Item 12 | 1.67 ± 1.42 | 0.62 | 0.87 | 0.39 | −1.03 | ||||
| Item 15 | 0.99 ± 1.29 | 0.52 | 0.87 | 1.19 | 0.58 | ||||
| Cognitive | 0.81 (0.76–0.86) | 0.80 | 0.52 | ||||||
| Item 5 | 1.81 ± 1.28 | 0.49 | 0.87 | 0.20 | −1.00 | ||||
| Item 10 | 1.79 ± 1.33 | 0.61 | 0.87 | 0.14 | −1.18 | ||||
| Item 14 | 1.74 ± 1.38 | 0.53 | 0.87 | 0.38 | −0.98 | ||||
| Item 17 | 1.83 ± 1.21 | 0.70 | 0.87 | 0.14 | −0.99 | ||||
| Escape/avoidance | 0.72 (0.64–0.78) | 0.72 | 0.35 | ||||||
| Item 3 | 2.15 ± 1.31 | 0.34 | 0.88 | −0.07 | −1.03 | ||||
| Item 6 | 2.04 ± 1.33 | 0.47 | 0.87 | 0.03 | −1.10 | ||||
| Item 8 | 1.69 ± 1.41 | 0.35 | 0.88 | 0.49 | −0.69 | ||||
| Item 11 | 1.86 ± 1.18 | 0.47 | 0.87 | 0.28 | −0.75 | ||||
| Item 20 | 2.31 ± 1.34 | 0.44 | 0.87 | −0.28 | −1.14 | ||||
AVE, average variance extracted; CI, confidence interval; SD, standard deviation.
Table 5 presents the correlations of the Spanish version of the CPASS with all the other measures. The total score of the CPASS was strongly correlated to pain catastrophising (r = 0.69), with a particularly strong correlation to the cognitive dimension (r = 0.70). In addition, we found an inverse and significant correlation of moderate magnitude between the CPASS and the self-reported HRQoL of paediatric patients (PedsQL) (r = −0.41), which was of low magnitude in the parent report (r = −0.22). Thus, patients who exhibited greater pain anxiety also exhibited more pain catastrophising and a poorer quality of life.
Convergent validity of the Spanish version of the Child Pain Anxiety Symptoms Scale.
| Spanish version of the Child Pain Anxiety Symptoms Scale (CPASS) | |||||
|---|---|---|---|---|---|
| Total Score | Fear | Physiological Anxiety | Cognitive | Escape/Avoidance | |
| Medical visits in the past year | −0.05 | −0.01 | −0.07 | −0.10 | 0.01 |
| Previous Surgeries | 0.10 | 0.10 | 0.07 | 0.12 | 0.03 |
| FPS-R | 0.18* | 0.22** | 0.13 | 0.09 | 0.12 |
| PPPM | 0.14 | 0.21* | 0.11 | 0.10 | 0.02 |
| PROMIS Pediatric Pain Interference | 0.31** | 0.33** | 0.18* | 0.28** | 0.18* |
| Pain Catastrophizing Scale for Children | 0.69** | 0.51** | 0.56** | 0.70** | 0.43** |
| PedsQLTM | |||||
| Child Response | −0.41** | −0.32** | −0.35** | −0.31** | −0.33** |
| Parent/Guardian Response | −0.22** | −0.15 | −0.17* | −0.22** | −0.15 |
FPS-R, Faces Pain Scale-Revised; PPPM, Parents Postoperative Pain Measure; PedsQL, Pediatrics Quality of Life Inventory.
With respect to pain-related variables, the CPASS was only moderately associated with patient self-reports of pain intensity (r = 0.18) and pain interference in daily life (r = 0.31). In particular, the fear dimension of the CPASS was most strongly correlated to pain-related variables (r, 0.21 to 0.33). In other words, children with higher CPASS scores, especially those with high scores on the fear dimension, reported greater disruption of their life attributed to pain in addition to more intense pain.
Last of all, we did not find any correlation between the CPASS score and the number of previous visits or surgeries.
DiscussionThe objective of this study was to translate the CPASS into Spanish and evaluate its psychometric properties. The results showed that the Spanish CPASS is a valid and reliable scale that can be used in children and adolescents.
First, the results of the EFA indicated problems with 2 items. Specifically, item 18 (“I find it hard to relax my body after I feel pain”) had a low factor loading, so we excluded it from the final model. A possible reason is that although the construct was explained to the patients, they may not have understood it correctly or clearly identified this sensation. Children may have had problems identifying this sensation because their anxiety may have made it difficult to relax, especially when in pain,29 and because they may express pain anxiety in the form of fearful or avoidant behaviours, as described in previous studies.10,16 As for item 19 (“I worry when I feel pain”), we found that it loaded similarly in 2 dimensions (fear and escape/avoidance) instead of on the cognitive dimension, as reported in the psychometric studies of the original scale10 and the Catalan version.16 Based on the findings of previous studies10,16 and our own, it seems that children tend to construe worry as akin to fear rather than as a cognitive response, probably because they respond to fear with avoidant behaviour, as previously described in the literatury.30,31 Although the difference between both factors was small (fear = 0.41, escape/avoidance = 0.40), we also chose to discard this item from the final model. The CFA corroborated that the 18-item, 4-factor model was the one that offered the best fit. The 4-factor model is the most widespread in the literature in both paediatric and adult populations, and it is also the one that has shown improvement in assessing pain-related anxiety.10,11,16,32,33
The internal consistency of the Spanish CPASS was acceptable (Cronbach α, 0.88), in agreement with the findings of previous studies that analysed the psychometric properties of the scale in other populations (original version10: Cronbach α, 0.90; Catalan version16: Cronbach α, 0.87; and study in a sample of surgical patients11: Cronbach α, 0.91). When it came to the 4 dimensions of the Spanish CPASS, we found adequate values (internal consistency ≥ 0.72). Previous versions also exhibited an acceptable internal consistency for the dimensions, except for the physiological anxiety and escape/avoidance constructs, for which the obtained Cronbach α values were near but inferior to 0.70 (physiological anxiety, α = 0.6810,11,16; escape/avoidance, α = 0.67).11,16 These slight differences could be explained by the better fit of the model with the elimination of items 18 and 19. Nevertheless, the data provide strong evidence that the Spanish CPASS is a reliable instrument that can be used in the paediatric and adolescent populations. The Spanish CPASS also showed an adequate discriminatory capacity since no floor or ceiling effects were identified.
In the convergent validity analysis, the CPASS is strongly correlated to pain catastrophising. Specifically, in our study, the cognitive dimension was strongly correlated to pain-related catastrophising. The relationship between pain-related anxiety and catastrophising can be explained as anticipatory cognitions and psychological feedback constructs.7,10 On the other hand, pain-related anxiety was moderately associated with HRQoL and with the pain interference reported by children. Pain-related anxiety probably amplifies the impact of pain5 because it produces discomfort in children, reducing their quality of life6 and limiting their activities.11,34 Similarly, based on the observed weak correlation between anxiety and pain intensity, the impact of pain could increase or produce high levels of anxiety related to pain.10 As expected, however, anxiety had a greater impact on pain-related behaviours than on pain intensity. This is probably explained by the fact that anxiety, as an emotion/sensation closely related to fear and restlessness, promotes avoidant behaviours (eg, limiting the level of activity).6,35,36 Our results corroborate the relationship between fear and anxiety, given that the fear dimension was the one with the strongest correlation to pain-related variables. Lastly, we did not find an association between pain-related anxiety and the number of visits or of previous surgeries. In the sample under study, 65% of the participants had not undergone a previous surgery, a very high percentage, which would indicate that the development of anxiety related to pain would not be just an innate personality trait and could be mediated by the learning process of pain or by parental influences (for example, parental anxiety can be transmitted to children).37,38
Limitations and future researchThere are limitations to this study. Firstly, although we assessed the psychometric properties of the scale, we were not able to assess changes over time and the ability of the scale to predict scores (responsiveness). It would be interesting to assess these aspects in future studies. Secondly, the sample size did not reach the 200 subjects/observations established as the minimum necessary to evaluate the psychometric properties of an instrument, but other authors consider that a sample of at least 100 subjects may suffice if the model fits reasonably well.39,40 Nevertheless, it is important to note that the sample size could have affected the results obtained in this study. Thirdly, the heterogeneity of the sample could also affect the results, as the age range of participants varied widely (8–18 years), and they had a broad range of clinical conditions (in terms of the type of disease, comorbidities, etc). Nevertheless, our results corroborate the external validity of the scale and suggest that the Spanish version of the CPASS is suitable for application regardless of the heterogeneity of the sample. Last of all, we did not assess how anxiety changed over time; future studies could examine how anxiety changes over time, with or without pain, and its association to other changes in pain-related domains in the patients.
ConclusionIn conclusion, the Spanish CPASS was a valid and reliable tool to assess pain anxiety in a clinical sample of children and adolescents.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors have no conflicts of interest to declare.
Author contributionsCB conceived and designed the study, designed the data collection instruments, collected data, carried out the analyses and drafted and revised the manuscript.
MC and LDUV conceived and designed the study, coordinated and supervised data collection, and critically reviewed and revised the manuscript, contributing important intellectual content.
GF critically reviewed and revised the manuscript, contributing important intellectual content.
We express our deep gratitude to all the patients and families that participated in the study for their involvement and interest. We would like to make special mention of and thank all the nursing staff of the department of surgery of the Hospital 12 de Octubre and the supervisor and staff of the day hospital, for their involvement and enormous collaborative effort.