A boy aged 18 months with a history of recurrent respiratory infections presented with fever and cough of 3 days’ duration, hypoxaemia (SpO2, 85%), and a murmur in the lower right hemithorax. Blood tests revealed leukocytosis, neutrophilia and elevation of C-reactive protein. The viral panel detected metapneumovirus. There was opacification of the right lung in the chest X-ray. The hypoxaemia persisted despite oxygen therapy, and a thoracic point-of-care ultrasound (POCUS) scan confirmed the abnormalities in the right lung(Fig. 1, panel A).
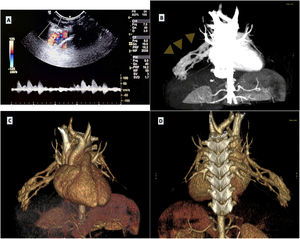
Complex pulmonary arteriovenous malformation (AVM) in the right middle lobe in a boy aged 18 months. (A) Thoracic POCUS with a stronger Doppler signal along the right thoracic wall at the level where a murmur was heard on auscultation. (B) CT angiogram showing the pulmonary AVM (arrowheads). (C and D) 3D reconstruction of CT scan provides both anterior and posterior views of the intricate pulmonary AVM, illustrating its complexity.
A CT angiogram revealed a arteriovenous malformation (AVM) in the right middle lobe (Fig. 1, panel B-D). The family history was suggestive of hereditary haemorrhagic telangiectasia (HHT), and abdominal and brain imaging showed no vascular anomalies. Embolization with a nitinol vascular plug improved oxygen levels. Genetic testing is underway.
The diagnosis of pulmonary AVMs in children can be suggested by persistent hypoxaemia.1 Their symptoms include dyspnoea, haemoptysis, cough, chest pain, finger clubbing and cyanosis. Patients with HHT may display early signs like epistaxis and telangiectases.1 Pulmonary AVMs can lead to respiratory infections, embolisms and haemoptysis, which can be managed with tranexamic acid.2 Early detection is crucial.
The approach to diagnosis includes non-invasive methods like transthoracic contrast echocardiography and pulse oximetry.1,3 POCUS can be useful for diagnosis when AVM is already suspected.3 Additional steps may involve chest CT scans, pulmonary angiography and genetic testing to identify HHT-related mutations (endoglin and ALK-1 genes on chromosomes 9 and 12).1 Treatment for pulmonary AVMs involves embolization to block abnormal vessels and reduce complications.1