In the paediatric population, coronavirus disease (COVID-19) is usually asymptomatic or mild, but there are also severe and fatal cases.
MethodsWe analysed data on COVID-19 cases from the national and state-level databases of the Federal Ministry of Health of Mexico and the Department of Health of Mexico City to determine the clinical characteristics and risk factors for mortality in children. We used Cox proportional hazards regression analysis to calculate the risk of death.
ResultsThe national and Mexico City databases had recorded a total of 18,465 (2.8%) and 5,733 (4.2%) confirmed cases of COVID-19, respectively, in individuals aged less than 18 years as of September 2020. The median age at diagnosis was 12 years (range: 0–17). The differences between cases in the national vs Mexico City databases were: 12.5% vs 8.2% of patients were hospitalised; 6% vs 3.5% had pneumonia; 2.4% vs 1.9% were admitted to the intensive care unit (ICU), and 1.3% vs 0.7% died. The independent risk factors significantly associated with a higher probability of death were pneumonia, hypertension, obesity, immunosuppression and intubation.
ConclusionIn Mexico, 2.8% of all confirmed cases of COVID-19 occurred in individuals under 18 years, with a median age of 12 years and a mortality of 1.3%. The identified predictors of mortality were pneumonia, admission to the ICU, obesity, hypertension, immunosuppression, diabetes, chronic lung disease and renal disease.
En la población pediátrica, el COVID-19 suele ser asintomático o leve, pero puede haber casos graves y mortales.
MétodosSe analizaron datos de los casos de COVID-19 registrados en las bases de datos nacional y regional de la Secretaría de Salud Federal de México y la Secretaría de Salud de Ciudad de México para establecer las características clínicas y los factores de riesgo de mortalidad en la población pediátrica. El riesgo de defunción se calculó mediante el método de regresión de riesgos proporcionales de Cox.
ResultadosLas bases de datos nacional y de Ciudad de México, respectivamente, registraban un total de 18.465 (2,8%) y de 5.733 (4,2%) de casos confirmados de COVID-19 en menores de 18 años en septiembre de 2020. La edad mediana al diagnóstico fue de 12 años (rango: 0-17). Las diferencias encontradas en los casos registrados a nivel nacional en comparación con los registrados en la Ciudad de México fueron: 12,5 vs. 8,2% de pacientes hospitalizados; 6 vs. 3,5% con diagnóstico de neumonía; 2,4 vs. 1,9% ingresados en la unidad de cuidados intensivos (UCI) y 1,3 vs. 0,7% fallecidos. Los factores de riesgo independientes asociados a una probabilidad mayor de defunción fueron el diagnóstico de neumonía, la hipertensión, la obesidad, la inmunosupresión y la intubación.
ConclusionesEn México, el 2,8% del total de casos confirmados COVID-19 se dan en pacientes menores de 18 años, con una mediana de edad de 12 años y una mortalidad del 1,3%. Los factores de riesgo de mortalidad identificados fueron el diagnóstico de neumonía, el ingreso en la UCI, la obesidad, la hipertensión, la inmunosupresión, la diabetes, la enfermedad pulmonar crónica y la enfermedad renal.
Since the first cases of coronavirus disease 2019 (COVID-19) were notified in China in the early months of 2020, adults were reported to be most affected, with 98% of the cases detected in patients aged more than 20 years and only 2% in minors under 19 years.1,2 One of the first paediatric case series of infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in China described cases in 341 children. The median age was 7 years (4-14) and 66% had been infected by a family member with COVID-19, with a median incubation period of 9 days; 99.3% had mild to moderate disease, and only 0.6% and 0.3% developed severe or critical disease, respectively. The presenting symptoms were fever (77.9%), cough (32.4%) and, less frequently, diarrhoea (4.4%), nausea and vomiting (2.9%), abnormal tear production (4.4%) and nasal discharge, sore throat, dizziness, headache, myalgia and fatigue (2.2%). Overall, outcomes were favourable, with improvement in 16 days and no deaths.3 As the pandemic started to spread to other countries and continents, the number of reported cases in children grew, including some of severe disease and with fatal outcomes. A case series in France that included 27 children with COVID-19 described respiratory involvement in 89%, mechanical ventilation in 9, administration of catecholamines in 4, erithropheresis in 4, renal replacement therapy in 1, and extracorporeal membrane oxygenation in 1. Five children died, including 3 with no comorbidity. These reports highlight the broad clinical spectrum of COVID-19 in children and the possibility of cases of severe disease and death in this population.4
A systematic review of COVID-19 in children that included large case series from China, Italy, Spain, and the United States in addition to small case series and case reports found that children constitute a minority (< 2%) of the patients with symptomatic COVID-19 and amount to 5% to 21% of all asymptomatic cases, and that a large proportion of children with COVID-19 exhibit symptoms of common viral upper respiratory infections. The reported frequency of severe disease ranges from 1% to 6%, including patients with multisystem inflammatory syndrome in children (MIS-C), and a low mortality, with most deaths occurring in children with comorbidities. The clinical manifestations are very similar to those of infection by other viruses, and laboratory testing is needed to diagnose SARS-CoV-2 infection. The morbidity and mortality associated with SARS-CoV-2 infection seem to be lower compared to respiratory syncytial virus (RSV) or influenza.5
The aim of our study was to analyse the clinical characteristics and risk factors for mortality in patients aged less than 18 years with confirmed infection by SARS-CoV-2 based on information obtained from the databases of the Federal Ministry of Health of Mexico and the regional Department of Health of Mexico City.
MethodsWe conducted a study of the data available on the official open access databases of the Mexican government. We retrieved nationwide data on COVID-19 cases on September 12th, 2020 from the website of the Federal Ministry of Health of Mexico (https://coronavirus.gob.mx/datos/) and local data on COVID-19 cases in Mexico City on September 13th, 2020 from the website of the local Department of Health (https://covid19.cdmx.gob.mx). We applied the following criteria to include cases from either database: confirmed SARS-CoV-2 infection, child (male or female) aged less than 18 years. We excluded duplicate cases, records missing data on mortality, date of onset, date of diagnosis, date of end of episode of care, diagnosis not confirmed by SARS-CoV-2 polymerase chain reaction (PCR) test. The records obtained from the 2 databases were treated as 2 separate cohorts (Mexico [country] and Mexico City). Death was the terminal event (failure). We defined the duration of follow-up as the time (in days) elapsed from the onset of COVID-19 symptoms to failure (death) or censoring (recovery, last medical visit, or end of episode of care). In the statistical analysis, we generated survival curves using the Kaplan-Meier method. The survival curves were compared by means of the log-rank and generalised Wilcoxon tests. The risk of death was estimated by means of hazard ratios, given by the exponent of the coefficients obtained in the proportional hazards regression analysis, both crude and adjusted for different covariates. P-values were calculated with the corresponding 95% confidence intervals. We present the most relevant predictive multivariate models. We used correlation matrices to assess multicollinearity in the variables included in the model. We tested the proportional hazards assumption by means log–log plots. The statistical analyses were performed with the software SPSS for Windows, version 26.
ResultsFrom the first case reported in Mexico on February 28th, 2020 through September 13th, 2020, the Federal Ministry of Health of Mexico has reported 658 299 confirmed cases in individuals of any age nationwide, of who 18 465 (2.8%) were aged less than 18 years. In the same period, the Department of health of Mexico City reported 135 742 confirmed cases in individuals of any age statewide, of who 5733 (4.2%) were aged less than 18 years
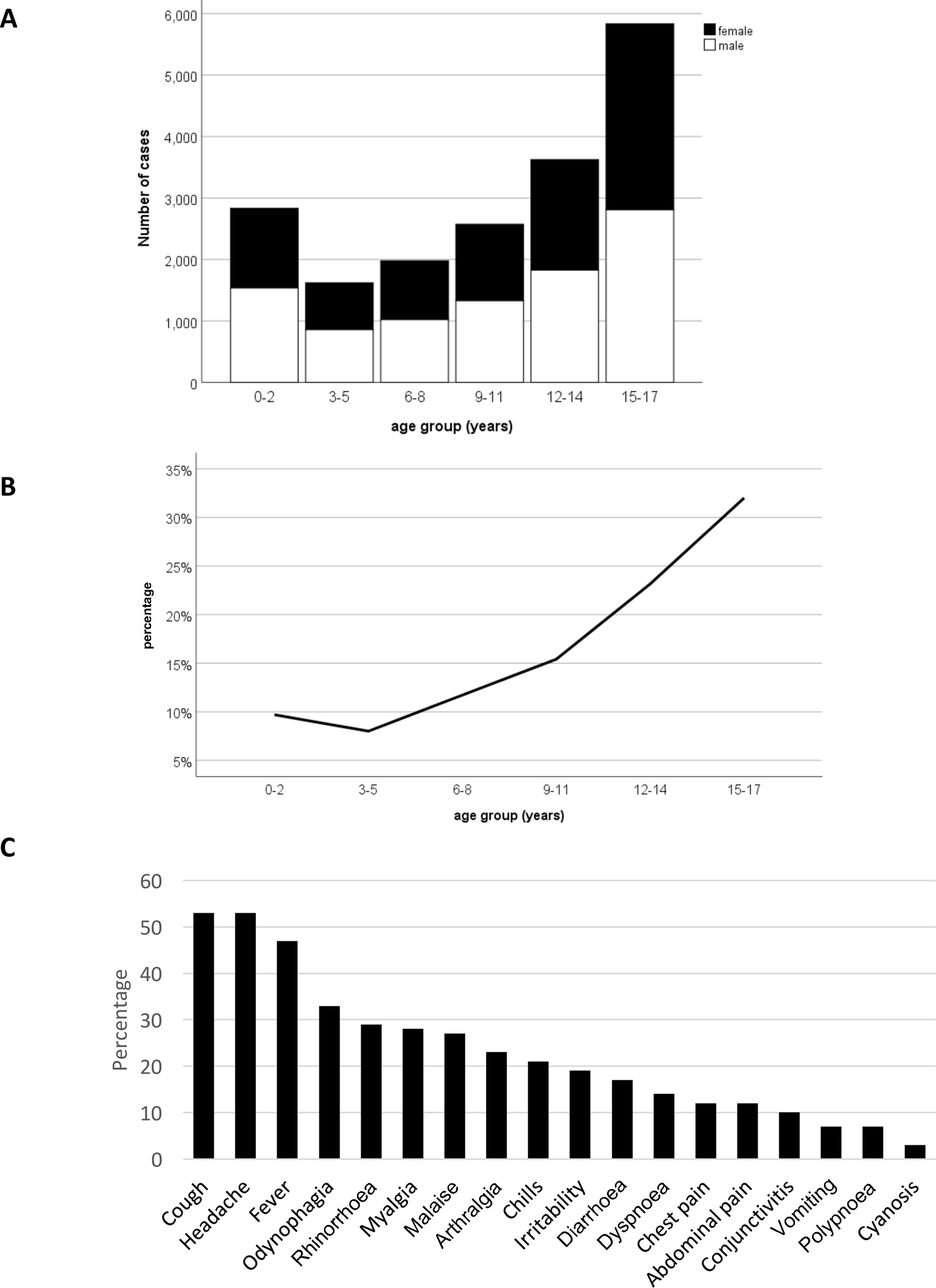
At the national level, older children were most affected, with 5835 cases (31.6%) in the 15-to-17 years age group, 3625 (19.6 %) in the 12-to-14 years group, 2574 (13.9%) in the 9-to-11 years group, 1979 (10.7%) in the 6-to-8 years group, 1621 (8.8%) in the 3-to-5 years group and 2831 (15.3%) in the 0-to-2 years group. The proportion of children with a known history of contact with a COVID-19 case was also higher in older children, with exposure documented in 33% of patients in the 15-to-17 years group, 23% in the 12-to-14 years group, 15% in the 9-to-11 years group, 12% in the 6-to-8 years group, 8% in the 3-to-5 years group and 10% in the 0-to-2 years group (Fig. 1B).
Some characteristics were similar in both cohorts: the median age in both was 12 years (range, 0-17), 49.2% and 48.9% of patients were female and 50.8% and 51.1% of patients were male, respectively. On the other hand, there were also some differences between the paediatric cases registered in the 2 databases: at the national level, 12.5% of patients with confirmed COVID-19 were admitted to hospital, compared to 8.1% in Mexico City, while 87.5% of patients nationwide and 91.9% in Mexico City were managed at the outpatient level; a higher proportion of patients had pneumonia at the national level (6% vs 3.5% in Mexico City), as was admission to the intensive care unit (ICU) (2.4% in Mexico vs 1.9% in Mexico City); intubation (1.7% nationwide compared to 1.2% in Mexico City) and pregnancy in adolescent female patients (1.3% nationwide vs 0.5% in Mexico City). A higher proportion of patients in Mexico City had a history of contact an infected person (69.1% vs 58.8% at the national level).
Of the cases reported by the Federal Ministry of Health, 26% were in residents of Mexico City and 73.8% in other states (Table 1). In addition, the Department of Health of Mexico City reported that 13.3% of the cases were detected by an influenza surveillance unit, as well as 40 deaths (0.7%), 54 (0.8%) cases of severe disease, 1515 (26.4%) cases followed up at home, 2231 (38.9%) patients whose symptoms improved and 1517 (26.5%) that remained in follow-up while receiving treatment. The initial diagnosis was flu-like syndrome in 5143 patients (89.7%), and only 1205 (21%) had been vaccinated against influenza in the past year; 416 patients (7.3%) received antibiotherapy and 84 (1.5%) antiviral treatment (Table 1). The mortality due to COVID-19 in children under 18 years was 1.3% in all of Mexico and 0.7% in Mexico City (Table 1).
Demographic and clinical characteristics of confirmed positive cases of COVID19 in patients aged less 18 years in Mexico and Mexico City, March-September 13th, 2020.
| Variable | MEXICO | MEXICO CITY | |
|---|---|---|---|
| N = 18 465 | N = 5733 | ||
| n (%) | n (%) | ||
| Age (years) | Median (range) | 12 (0-17) | 12 (0-17) |
| Sex | Female | 9088 (49.2%) | 2805 (48.9%) |
| Male | 9377 (50.8%) | 2928 (51.1%) | |
| Type of patient | Hospitalized | 2304 (12.5%) | 462 (8.1%) |
| Outpatient | 16161 (87.5%) | 5271 (91.9%) | |
| State of origin | Mexico City | 4831 (26.2%) | – |
| Other | 13634 (73.8%) | – | |
| State of care delivery | Mexico City | 5619 (30.4%) | – |
| Other | 12846 (69.6%) | – | |
| Diagnosis of pneumonia | Yes | 1107 (6.0%) | 198 (3.5%) |
| Admission to intensive care unit | Yes | 449 (2.4%) | 111 (1.9%) |
| Intubation | Yes | 320 (1.7%) | 66 (1.2%) |
| Pregnancy (out of 9088 and 2805 women) | Yes | 115 (1.3%) | 14 (0.5%) |
| History of contact with an infected person | Yes | 10857 (58.8%) | 3959 (69.1%) |
| Detection by an Influenza monitoring unit | Yes | – | 763 (13.3%) |
| No | – | 4970 (86.7%) | |
| Outcome | Death | 244 (1.3%) | 40 (0.7%) |
| Severe | – | 54 (0.9%) | |
| In treatment | – | 1517 (26.5%) | |
| Follow-up at home | – | 1515 (26.4%) | |
| Improvement | – | 2231 (38.9%) | |
| Other | – | 376 (6.6%) | |
| Initial diagnosis of flu-like syndrome | Yes | – | 5143 (89.7%) |
| Influenza vaccination in past year | Yes | – | 1205 (21.0%) |
| Antibiotic treatment | Yes | – | 416 (7.3%) |
| Antiviral treatment | Yes | – | 84 (1.5%) |
- Data not available or not aplicable.
The symptoms associated with COVID-19 in children younger than 18 years old documented in the Mexico City database were cough (53%), headache (53%), fever (47%), odynophagia (33%), rhinorrhoea (29%), myalgia (28%), general malaise (27%), arthralgias (23%), chills (21%), irritability (19%), diarrhoea (17%), dyspnoea (14%), chest pain (12%), abdominal pain (12%), conjunctivitis (10%), vomiting (7%), polypnoea (7%) and cyanosis (3%) (Fig. 1C).
Some of the characteristics of deceased patients were different in Mexico compared to Mexico City: median age of 3 vs 8 years, 53% vs 67.5% female, 28.7% vs 37.5% admitted to the ICU, 5.3% vs 7.5% with diabetes, 0.4% vs 2.5% with chronic pulmonary disease, 3% vs none with asthma, 20% vs 15% immunosuppressed, 4.1% vs 7.5% with hypertension, 3.7% vs none with heart disease, 8.2% vs 15% obese, 3.3% vs 10% with chronic renal failure, 1.6% vs none that smoked, respectively. Other characteristics of deceased children were similar in the Mexico and Mexico City cohorts: most were in the 0 to 2 years age group (48% vs 37.5%), were hospitalised (93% vs 90%) and had pneumonia (68.4% vs 67.5%) and approximately half were intubated (50.4% vs 57.5%). The symptoms and clinical characteristics described in deceased paediatric patients in Mexico were: fever (75%), cough (62.5%), odynophagia (25%), dyspnoea (55%), irritability (32.5%), diarrhoea (15%), chest pain (25%), chills (20%), headache (40%), myalgia (22.5%), arthralgia (30%), malaise (52.5%), rhinorrhoea (27.5%), polypnoea (17.5%), vomiting (7.5%), abdominal pain (17.5%), conjunctivitis (5%), cyanosis (7.5%), diagnosis of flu-like syndrome at the admission (45%), diagnosis of severe respiratory tract infection (55%), vaccination against influenza in the last year (5%), antibiotic treatment (30%) and antiviral treatment (5%) (Table 2).
Demographic and clinical characteristics of the deceased children younger than 18 years old in confirmed positive cases of COVID19 in Mexico and Mexico City. March-September 13th, 2020.
| Variable | MEXICO | MEXICO CITY | |
|---|---|---|---|
| N = 244 | N = 40 | ||
| n (%) | n (%) | ||
| Age (years) | Median (range) | 3 (0-17) | 8 (0-17) |
| Group of age | 0-2 years | 119 (48.8%) | 15 (37.5%) |
| 3-5 years | 18 (7.4%) | 1 (2.5%) | |
| 6-8 years | 14 (5.7%) | 5 (12.5%) | |
| 9-11 years | 24 (9.8%) | 5 (12.5%) | |
| 12-14 years | 25 (10.2%) | 7 (17.5%) | |
| 15-17 years | 44 (18%) | 7 (17.5%) | |
| Sex | Female | 114 (46.7%) | 13 (32.5%) |
| Male | 130 (53.3%) | 27 (67.5%) | |
| Type of patient | Hospitalized | 228 (93.4%) | 36 (90%) |
| Outpatient | 16 (6.6%) | 4 (10%) | |
| State of origin | Mexico City | 20 (8.2%) | – |
| Other | 224 (91.8%) | – | |
| State of care delivery | Mexico City | 40 (16.4%) | – |
| Other | 204 (83.6%) | – | |
| Diagnosis of pneumonia | 167 (68.4%) | 27 (67.5%) | |
| Admission to intensive care unit | 70 (28.7%) | 15 (37.5%) | |
| Intubation | 123 (50.4%) | 23 (57.5%) | |
| Diabetes | 13 (5.3%) | 3 (7.5%) | |
| Chronic pulmonary disease | 1 (0.4%) | 1 (2.5%) | |
| Asthma | 3 (1.2%) | 0 | |
| Immunosupression | 25 (10.2%) | 6 (15%) | |
| Hypertension | 10 (4.1%) | 3 (7.5%) | |
| Cardiopathy | 9 (3.7%) | 0 | |
| Obesity | 20 (8.2%) | 6 (15%) | |
| Chronic kidney failure | 8 (3.3%) | 4 (10%) | |
| Smoking | 4 (1.6%) | 0 | |
| History of contact with an infected individual | – | 7 (17.5%) | |
| Fever | – | 30 (75%) | |
| Cough | – | 25 (62.5%) | |
| Odynophagia | – | 10 (25%) | |
| Dyspnoea | – | 22 (55%) | |
| Irritability | – | 13 (32.5%) | |
| Diarrhoea | – | 6 (15%) | |
| Chest pain | – | 10 (25%) | |
| Chills | – | 8 (20%) | |
| Headache | – | 16 (40%) | |
| Myalgia | – | 9 (22.5%) | |
| Arthralgia | – | 12 (30%) | |
| Malaise | – | 21 (52.5%) | |
| Rhinorrhoea | – | 11 (27.5%) | |
| Polypnoea | – | 7 (17.5%) | |
| Vomiting | – | 3 (7.5%) | |
| Abdominal pain | – | 7 (17.5%) | |
| Conjunctivitis | – | 2 (5%) | |
| Cyanosis | – | 3 (7.5%) | |
| Diagnosis of FLS at the admission | – | 18 (45%) | |
| Diagnosis of severe RTI | – | 22 (55%) | |
| Influenza vaccination in the past year | – | 2 (5%) | |
| Antibiotic treatment | – | 12 (30%) | |
| Antiviral treatment | – | 2 (5%) |
FLS, flu-like syndrome; RTI, respiratory tract infection.
Table 3 presents the risk factors most strongly associated with mortality in all of Mexico and in Mexico City in the crude Cox regression analysis. We ought to mention that the Mexico City database includes more variables, mainly related to symptoms, than the national database. However, we found a statistically significant association with an increased risk of mortality for the following variables: intubation (hazard ratio, Mexico [HRM], 68.5; hazard ratio, Mexico City [HRMC], 129.8), diagnosis of pneumonia (HRM, 36.1; HRMC, 59.0), admission to the ICU (HRM, 17.0; HRMC, 30.7), chronic pulmonary disease (HRM: 4.7; HRMC, 43.0), chronic renal disease (HRM, 6.8; HRMC, 22.8), diabetes (HRM, 8.0; HRMC, 15.6), obesity (HRM, 1.9; HRMC, 4.0), hypertension (HRM, 6.6; HRMC, 17.1) and immunosuppression (HRM, 5.7; HRMC, 8.1). Conversely, age was inversely associated with mortality (HRM, 0.88; HRMC, 0.90), and the risk of death decreased by 10% to 12% with each additional year of age. Known contact with an infected person was also associated with a lower risk for death (HRM, 0.14; HRMC, 0.09). The proportion of patients with a history of exposure to SARS-CoV-2 increased with age (data not shown). The results for the association between male sex and mortality were at the threshold of significance only in the Mexico City cohort (HRMC, 1.9, 95% confidence interval [CI], 1.03-3.9; P = .04). Vaccination against influenza in the previous year (HRMC, 0.20) and the months elapsed since the administration of the influenza vaccine (in the past year) (HRMC, 0.76) were also associated with a decreased risk of death in the Mexico City cohort.
Risk factors associated with the probability of death in patients under 18 years with confirmed COVID 19 in Mexico and Mexico City, March-September 13th, 2020. Unadjusted analysis.
| Variable | cHR | 95% CI | P |
|---|---|---|---|
| MEXICO (N = 18 465) | |||
| Male sex | 1.11 | 0.86-1.42 | .44 |
| Age (years) | 0.88 | 0.87-0.90 | < .0001 |
| Admission to intensive care unit | 17.0 | 12.8-22.4 | < .0001 |
| Intubation | 68.5 | 53.2-88.0 | < .0001 |
| Pneumonia | 36.1 | 27.6-47.3 | < .0001 |
| Diabetes | 8.0 | 4.6-13.9 | < .0001 |
| Chronic obstructive pulmonary disease | 4.7 | 0.7-33.3 | .12 |
| Immunosuppression | 5.7 | 3.8-8.7 | < .0001 |
| Hypertension | 6.6 | 3.5-12.5 | < .0001 |
| Obesity | 1.9 | 1.2-3.1 | .004 |
| Chronic kidney disease | 6.8 | 3.4-13.8 | < .0001 |
| Contact with positive case | 0.14 | 0.10-0.19 | < .0001 |
| State of origin (Mexico City vs other) | 0.25 | 0.16-0.40 | < .0001 |
| State of care delivery (Mexico City vs other) | 0.45 | 0.32-0.63 | < .0001 |
| MEXICO CITY (N = 5733) | |||
| Male sex | 1.9 | 1.03-3.9 | .04 |
| Age (years) | 0.90 | 0.85-0.95 | < .0001 |
| Admission to intensive care unit | 30.7 | 16.2-58.2 | < .0001 |
| Intubation | 129.8 | 69.3-243.0 | < .0001 |
| Pneumonia | 59.0 | 30.4-114.4 | < .0001 |
| Fever | 3.3 | 1.6-6.7 | .001 |
| Dyspnoea | 7.7 | 4.1-14.3 | < .0001 |
| Irritability | 2.04 | 1.05-4.0 | .04 |
| Chest pain | 2.4 | 1.2-4.9 | .02 |
| Headache | 0.58 | 0.31-1.09 | .09 |
| Malaise | 2.9 | 1.6-5.4 | .001 |
| Polypnoea | 2.9 | 1.3-6.6 | .01 |
| Cyanosis | 2.8 | 0.86-9.0 | .09 |
| Sudden onset | 2.5 | 1.3-4.6 | .005 |
| Diabetes | 15.6 | 4.8-50.6 | < .0001 |
| Chronic obstructive pulmonary disease | 43.0 | 5.9-314.2 | < .0001 |
| Immunosuppression | 8.1 | 3.4-19.4 | < .0001 |
| Hypertension | 17.1 | 5.3-55.5 | < .0001 |
| Obesity | 4.0 | 1.7-9.6 | .002 |
| Chronic kidney disease | 22.8 | 8.1-64.1 | < .0001 |
| Antibiotic treatment | 5.4 | 2.7-10.6 | < .0001 |
| Antiviral treatment | 3.5 | 0.9-14.6 | .08 |
| Contact with positive case | 0.09 | 0.04-0.21 | < .0001 |
| Influenza vaccination in the past year | 0.20 | 0.05-0.81 | .02 |
| Time (months) from influenza vaccination | 0.76 | 0.59-0.97 | .03 |
CI, confidence interval; cHR, crude hazard ratio.
Table 4 presents the results of multivariate models obtained by Cox proportional hazard regression analysis. When it came to the nationwide cohort model, diagnosis of pneumonia (HRM, 8.6), hypertension (HRM, 3.4), obesity (HRM, 1.7), immunosuppression (HRM, 1.4), and intubation (HRM, 10.3) were independent predictors significantly associated with a higher probability of death. On the other hand, in the same cohort, the years of age (HRM, 0.97), history of contact with an infected individual (HRM, 0.28), and state of origin (Mexico City vs other) (HRM, 0.60) were independent predictors significantly associated with a lower probability of death. We also fitted 2 multivariate models for the Mexico City cohort. In both models, male sex (HRMC, 2.3 [model 1] and 3.4 [model 2]), diagnosis of pneumonia (HRMC, 26.9 [model 1] and 8.8 [model 2]), obesity (HRMC, 2.5 [model 1] and 2.7 [model 2]) and chronic kidney disease (HRMC, 7.1 [model 1] and 2.8 [model 2]), were independent predictors consistently associated with a higher probability of death. Age in years (HRMC, 0.96), admission to the ICU (HRMC, 4.1), hypertension (HRMC, 4.1), diabetes (HRMC, 4.7), intubation (HRMC, 20.1), the history of contact with infected person (HRMC, 0.18), general malaise (HRMC, 1.8), and chronic obstructive pulmonary disease (HRMC, 34.6) were other independent predictors associated with a higher or lower probability of death in one of the two models.
Multivariate models to estimate the probability for death in patients under 18 years with confirmed COVID in Mexico and in Mexico City. September 13th, 2020.
| MEXICO (N = 18 465) | Multivariate model | ||
|---|---|---|---|
| Variable | aHR | 95% CI | P |
| Age (years) | 0.97 | 0.95-1.0 | .02 |
| Pneumonia | 8.6 | 6.1-12.1 | < .0001 |
| Hypertension | 3.4 | 1.8-6.6 | < .0001 |
| Obesity | 1.7 | 1.1-2.8 | .02 |
| Immunosuppression | 1.4 | 1.0-2.2 | .09 |
| Intubation | 10.3 | 7.5-14.1 | < .0001 |
| Contact with positive case | 0.28 | 0.19-0.39 | < .0001 |
| State of origin (Mexico City vs other) | 0.60 | 0.38-0.96 | .03 |
| MEXICO CITY (N = 5733) | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Variable | aHR | 95% CI | P | aHR | 95% CI | P |
| Male sex | 2.3 | 1.2-4.5 | .02 | 3.4 | 1.7-7.0 | .001 |
| Age (years) | 0.96 | 0.91-1.01 | .10 | – | – | – |
| Admission to intensive care unit | 4.1 | 1.9-8.6 | < .0001 | – | – | – |
| Pneumonia | 26.9 | 12.5-57.9 | < .0001 | 8.8 | 3.8-20.6 | < .0001 |
| Hypertension | 4.1 | 0.9-18.0 | .07 | – | – | – |
| Diabetes | 4.7 | 1.0-22.1 | .05 | – | – | – |
| Obesity | 2.5 | 1.0-6.4 | .06 | 2.7 | 1.1-6.7 | .03 |
| Chronic kidney disease | 7.1 | 2.3-21.5 | .001 | 2.8 | 0.9-8.5 | .07 |
| Intubation | – | – | – | 20.1 | 8.8-46.1 | < .0001 |
| Contact with positive case | – | – | – | 0.18 | 0.08-0.42 | < .0001 |
| Malaise | – | – | – | 1.8 | 0.94-3.6 | .08 |
| Chronic obstructive pulmonary disease | – | – | – | 34.6 | 4.3-276.0 | .001 |
aHR, adjusted hazard ratio; CI, confidence interval.
One of the epidemiological characteristics of the COVID-19 pandemic is the lower severity of disease in children compared adults. Globally, the proportion of severe cases and deaths that are reported in children is small in comparison to adults, particularly compared with those older than 60 years of age.6 This contrasts with other viral respiratory infections, such as influenza and RSV infection, which are associated with frequent hospital admission and a high mortality in children worldwide.7,8 This is not to say that children are free of risk of severe SARS-CoV-2 infection. Multisystemic inflammatory syndrome in children (MIS-C) temporarily associated with SARS-CoV-2 may be best-known form of severe disease in the paediatric population,9,10 but children may also experience complicated respiratory infections requiring mechanical ventilation and admission to the ICU.11 Since death is a rare outcome in children, the evidence on the risk factors associated with mortality in children is more limited compared to adults.12
In this study, we found that 2.8% of cases of COVID-19 occurred in patients aged less than 18 years, with a higher frequency in older children that was consistent with the increasing proportion of known contact with a case with increasing age. The mortality was 1.3%, and it is worth noting that while older children were more likely to have the disease, almost half of deaths occurred in children under 2 years.
In our analysis of paediatric COVID-19 cases reported in Mexico, we found that younger age, male sex, certain underlying conditions (hypertension, obesity, immunosuppression, chronic kidney disease, diabetes, and chronic pulmonary disease) and severe respiratory illness (pneumonia, admission to ICU, need of intubation) were associated with an increase in mortality.
The risk factors for severe COVID-19 in paediatric patients have yet to be clearly established.13 A recent review summarized the published data on the risk factors for severe COVID-19 in children.12 The authors found that young age and underlying conditions were frequently reported in severe and fatal cases, but could not reach any definite conclusions regarding the role of specific comorbidities, partly due to the low frequency of death in children. Most of the underlying conditions associated with fatal COVID-19 in children identified in our study were well-known risk factors for severe respiratory infection in children,14,15 but there were also others, such as a history of hypertension, that have emerged as significant risk factors in adults with COVID-19 and had not been previously associated with acute respiratory infections in children. It is worth noting that the prevalence of hypertension in the child and adolescent population has been increasing in recent years, with a global prevalence of 4% in individuals under 19 years.16 Obesity, another condition whose prevalence in the paediatric population is on the rise, also emerged as a predictor of fatal outcome. While malnutrition has long been associated with severe respiratory infection, obesity has also been reported as a risk factor for severe illness in patients with viral respiratory infections, including COVID-19.17,18 In Mexico, obesity is a major public health problem; with a reported prevalence of 17.5% in children aged 5 to 11 years and of 14.6% in children and adolescents aged 12 to 19 years in 2018.19 Therefore, strategies aimed at reducing the impact of SARS-CoV-2 call for a broad range of intervention, focusing not only on the acute effects of infection, but on the overall health of the population.
Certain known risk factors for severity of influenza and RSV infections, such as congenital heart disease and preterm birth, have not been found to be associated with severe COVID-19 in children. A study of the characteristics of 77 children with severe COVID-19 requiring hospital admission in New York found a history of preterm birth in 9% and congenital heart disease in 6%11; the frequency of congenital heart disease was greater in this group compared to the general population, while the frequency of prematurity did not differ from the reported prevalence in the United States for the 2016-2018 period (9.57%-9.85%).20 A systematic review that analysed the characteristics of children with severe COVID-19 found that 75% of those that required mechanical ventilation had documented comorbidities, and cardiac diseases, including congenital heart defects and cardiomyopathy, were the most frequent type of comorbidity, present in 21% of children who required mechanical ventilation.21 These reports suggest that, similar to what occurs with other respiratory viruses, children with congenital heart disease might be at higher risk for severe COVID-19. Future studies in children should include a clear assessment of comorbidities, with particular emphasis on congenital heart diseases.
In general, results from the entire country of Mexico were similar to those of the Mexico City database. However, mortality was higher in Mexico overall (1.3%) compared to Mexico City (0.7%), and the strength of the association between different predictors and mortality varied between cohorts. The frequency of pneumonia, admission to the ICU and death were also lower in Mexico City. It is important to consider that although national guidelines on SARS-CoV-2 testing, patient management and transmission control measures are applicable to all states in Mexico, there are regional differences in their implementation. In addition, Mexico City has a substantially larger amount of health care resources compared to all other states in Mexico. For instance, in 2014 the number of hospital beds per 1000 inhabitants was 2.4 for Mexico City compared to 1 for the country overall.22 Thus, differences in the implementation of SARS-CoV-2 control policies or in access to health care may explain, at least in part, the observed differences between the 2 datasets. Supporting this hypothesis, an analysis of the global impact of COVID-19 in children evinced that paediatric mortality was higher in low- and middle-income countries compared with high-income countries.23 These findings underscore the need to take into account regional differences when assessing the impact of COVID-19 in different areas or countries.
It is also important to be aware of the fact that while mortality and severe disease may be infrequent in children, children may become infected, remain asymptomatic and transmit the virus to relatives that may develop more severe forms of disease, and therefore vaccination should also be contemplated in the paediatric age group.
One of the limitations of the study is that we did not collect the data prospectively or directly, but used retrospective data from open access databases obtained primarily through epidemiological surveillance programmes, so that the collection of data regarding underlying conditions was not tailored specifically to assess the paediatric population. Some of its strengths are that we retrieved information from 2 different databases, the large number of cases analysed, the uniform criteria applied in the case definition of COVID-19, and the inclusion of data covering the entire country. We also ought to highlight that the findings in both cohorts (nationwide and Mexico City cohorts) were consistent.
In conclusion, we identified predictors of mortality due to COVID-19 in Mexican children. Obesity was consistently associated with an increased probability of death, and hypertension, immunosuppression, diabetes, chronic lung disease and chronic renal disease were also underlying conditions associated with an increase in mortality. Further research is required to establish the impact of other comorbidities, such as congenital heart disease, in relation to the risk of severe COVID-19 in children.
Ethical considerationsThe study was exempt from approval, as it consisted in the analysis of secondary data from 2 open access databases retrieved from the official websites of the Federal Ministry of Health of Mexico and the Department of Health of Mexico City, neither of which include any personal identifiable information.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Wong-Chew RM, Noyola DE, Villa AR. Características clínicas y factores de riesgo de mortalidad en menores de 18 años con COVID-19 en México y Ciudad de México. An Pediatr (Barc). 2022;97:119–128.