The international development cooperation in child health arouses special interest in paediatric settings. In the last 10 years or so, new evidence has been presented on factors associated with morbidity and mortality in the first years of life in the least developed countries. This greater knowledge on the causes of health problems and possible responses in the form of interventions with impact leads to the need to disseminate this information among concerned professional paediatricians. Serious efforts are needed to get a deeper insight into matters related to global child health and encourage paediatricians to be aware and participate in these processes. This article aims to provide a social paediatric approach towards international cooperation and child health-related matters.
La cooperación internacional al desarrollo en salud infantil despierta un especial interés en el ámbito pediátrico. En los últimos decenios se han ido revelando nuevas evidencias en torno al análisis de los factores vinculados a la morbimortalidad en las primeras etapas de la vida en los países menos adelantados. Este mayor conocimiento del origen de los problemas de salud y las posibles respuestas en forma de intervenciones con impacto determina la necesidad de su divulgación entre los profesionales de Pediatría interesados. Se hacen necesarios mayores esfuerzos para profundizar en materias relacionadas con salud global infantil y favorecer el que los pediatras conozcan y participen en estos procesos. Este artículo pretende ofrecer un acercamiento pediátrico social hacia los elementos relacionados con cooperación internacional y salud infantil.
The Asociación Española de Pediatría (AEP: Spanish Association of Paediatrics) has not failed to respond to the growing interest in international cooperation among paediatricians in Spain. In 2011, with a view to channelling these concerns, it set up a working group which has raised awareness of the culture of cooperation and solidarity with developing countries in child health.1
Paediatrics must take a broad view and facilitate access to the best and most up-to-date methods for diagnosing and treating illness, as well as preventing them, promoting health and fostering adequate growth and development. This should be extended to all children without exception.
Paediatricians occupy a privileged position in that remarkable process of transformation by which children, after almost two decades, turn into adults, and they must take on areas of responsibility and professional commitment, together with other professionals and authorities, that extend to a setting beyond the geographical limits of their own country.
In this article we will try to address the subject and reflect on some of its defining features.
From international health to global healthSince the mid-1990s the field of international health has been renamed “global health”.2 This term implies the study and practice of health issues that transcend borders, in rich and poor regions.
Countries with greater resources help those that have fewer or none, although in many cases there are unexploited resources in the receiving countries and doubts continue to arise about conditioning factors or dependencies created by certain forms of cooperation, which have proved contentious.
International cooperation in development is based not only on the ethical principle of solidarity, but also on responsibility and on the need to recognise human rights beyond frontiers, cultures, races and religions.1,3
The field of global health must involve a rights-based approach. The Convention on the Rights of the Child (1989) establishes the right to survival and development among its governing principles.4 Paediatrics, and those who practise it, must act as guarantors of the contents of the Convention, by encouraging knowledge of and compliance with them.
Major efforts have been made in recent decades to improve global child health. In some cases, paradoxically, initiatives designed to solve problems by cost-effective means have provided answers applicable to countries that are not poor. This is true, for example, of oral rehydration salts, and of “kangaroo care”, initiated in Colombia in response to lack of resources. Attention should be drawn to the systematic work of the WHO Growth Assessment and Surveillance Unit, led by Mercedes de Onís, which resulted in the publication, in 2006, of the first international growth and development standards for all children under five years, valid all over the world.5
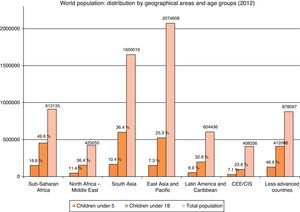
Childhood and adolescence: arguments for cooperation in healthAnalysing the distribution of world population by geographical region and paediatric age group (<18 years), and particularly those under 5, for the year 2012 (Fig. 1), we can see that out of a total of 7041 million people, 2124 million – approximately 31% – were aged under 18 and 652 under 5 (a little over 9%).6
One in every three inhabitants of the planet is under 18 and almost one in ten has not yet reached the age of 5. But as Fig. 1 shows, the distribution is not uniform, and in Sub-Saharan Africa practically one in two members of the population is of paediatric age.
Recognising the best evidence on the major problems affecting child health and some of the alternatives for treating them has been an essential task. The successive publications in the so-called “Lancet Series” have reconsidered many of the elements that define the reality of child health in a global health context, particularly in the most deprived countries.
In 2003, for example, the “Child Survival” series, in five parts, drew attention to under-five mortality in the world.7–11 It highlighted the death of more than 10 million children under the age of five per year, half of them in six countries (led by India, with over 2.4 million), the main causes being neonatal pneumonia, diarrhoea and malaria, although it pointed to various different epidemiological profiles depending on the specific features of countries (HIV/AIDS predominates in some cases, malaria or other causes in others, and in many of them underweight is identified as a comorbidity factor in varying proportions).7
Interventions were proposed, some described as “preventive” (exclusive breastfeeding up to six months of age, appropriate supplementary feeding, use of mosquito nets with insecticides, sanitation and clean drinking water, vitamin A, among others) and others as “therapeutic” (use of oral rehydration solutions, antibiotics for pneumonia, antimalarials, vitamin A, among others), that would reduce mortality. The authors stated that universal and exclusive breastfeeding for the first six months would alone prevent 1.3 million deaths a year.8 They pointed out the need to obtain epidemiological information, perform the best child survival interventions, implement mother-and-child health management strategies, identify factors related to differences due to inequity, and follow up successes.11
In 2005 the series entitled “Neonatal Survival” presented an analysis of factors associated with survival in the first month of life in four articles.12–15 With the gradual decrease in overall infant mortality, neonatal mortality constitutes the highest proportion and the niche where the greatest efforts should be focused. The deaths of over 4 million children per year in the neonatal period represents 38% of deaths in children under five years, with prematurity, severe infections and asphyxia as the main causes.12 Certain actions before conception (folic acid supplementation), before birth (tetanus vaccination, screening and treatment of syphilis …), during labour (antibiotics in preterm premature rupture of membranes, corticosteroids in preterm labour, surveillance and monitoring during delivery …) and after birth (neonatal resuscitation, breastfeeding …) can improve neonatal survival.
Undernutrition in under-fives is another challenge that has received special attention. In 2008 new evidence was presented in the series “Maternal and Child Undernutrition”,16–20 followed by a further revision in 2013 in “Child and Maternal Nutrition”.21–24
Many deaths of children under five are accompanied by acute malnutrition as a main cause or contributing cause. Chronic forms are also very important and may be associated with growth and development abnormalities, including motor and cognitive delays, as well as higher morbidity and mortality.25 Black et al.21 estimate that intrauterine growth delay, acute and chronic malnutrition, and also vitamin A and zinc deficiency, with non-exclusive or incomplete breastfeeding, were the cause of 3.1 million deaths in children under five in 2012, 45% of the total.
In general, successive improvements have reduced mortality in children under five, from 10 million in the year 2000 to just under 7 million currently, although neonatal mortality is falling more slowly.6
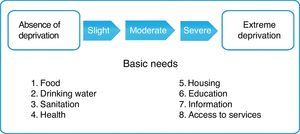
In this context we have to think of the child in his or her environment. Poverty pervades all aspects of health, education and society, establishing a vicious circle with disease, from which it is very difficult to escape. In children it can be expressed as a gradual succession of deprivations in basic needs, as shown in Fig. 2.26
The so-called “determinants approach”, promoted by the WHO, seeks to analyse and draw attention to the conditions in which many people are born, grow up, live, work and grow old.27
All this evidence must underpin scientific discourse and planning of cooperation in child health.
Challenges in global child healthThe Millennium Development Goals (MDG), formulated at the end of 2000, with the participation of almost 200 member states of the United Nations, set out a series of challenges for 2015.
Target 4 (to reduce the mortality rate in children under five years by two-thirds based on 1990 figures) is one of the most prominent of those affecting children. Experts point out that what has been achieved is insufficient. Major efforts have been made against pneumonia and diarrhoea, but tackling the problems related to nutrition could still save millions of lives. Recent successes in controlling measles may not be sustainable if funding is not maintained.26
Child health in these countries is directly associated with so-called “transitions”, demographic, epidemiological and nutritional, which are at different stages in each country. The “demographic transition” shows population changes in mortality and fertility (in general terms, a reduction in mortality in the first few moments of life, a reduction in the birth rate and an increase in life expectancy). The “epidemiological transition” shows population changes in the incidence of diseases and their causes (from a predominance of infections to prevalence of other, basically chronic conditions). The “nutritional transition” attempts to explain changes observed at the population level in relation to nutrition – in diet composition and availability of foods – as various phases of economic growth take place in societies. Thus, for example, a “double burden of malnutrition” (undernutrition with obesity) can be observed in some countries.28
Poverty in itself represents a challenge linked to child health. Although the percentage of people living in extreme poverty has been reduced from 43% in 1990 to 21% in 2010, if growth is weak and unevenly distributed there will still be 1.3 billion people in the world living in this situation by 2030.29
Child malnutrition, in its various forms, remains one of the most important challenges facing us.30
In the poorest countries, one of the comprehensive responses that has had the greatest impact on improving child health has been the Integrated Management of Childhood Illness (IMCI) strategy, launched in the mid-1990s. Its goal is to reduce morbidity and mortality in children under five by advocating a series of “key practices”, aimed at growth and development, disease prevention, household care and care seeking. It is not only applicable to health services, but also to the community and the home.26 It has undoubtedly made a notable contribution in various countries where it has been applied.
Framework for cooperation on child healthCooperation continues to pose serious technical and ethical problems.31
International cooperation for development involves a range of actors, among which we would highlight the following:
- -
Governments of countries with their own funds channelled through national agencies, with variable investment potential, related to economic capacity and willingness to intervene according to geostrategic interests. Notable examples are USAID (United States), JICA (Japan), GTZ (Germany), NORAD (Norway), ACDI (Canada), AFC (France) and AusAID (Australia). In the case of Spain there is AECID (the Spanish Agency for International Development Cooperation), which operates in over 50 countries, and other agencies of the autonomous communities of the Spanish State.
- -
Non-governmental organisations (NGOs) or charities, for which a more correct term would perhaps be the one used in other countries: non-profit organisations.
- -
Agencies of the United Nations system, which carry out humanitarian aid work or cooperate in development. Here we could mention UNICEF.
In the late 1970s Spain was regarded by the World Bank as a developing country, without a defined cooperation policy. In that period it was beginning to have a presence and participate in international organisations.32 In the last few decades it has decisively joined the group of actively participating countries.
The Spanish Master Plan for Cooperation for 2013–201633 lays down the guiding principles and highlights the need to continue facing up to challenges in the field of maternal and child health.
Humanitarian and emergency aid comprises a set of actions that are usually linked to needs arising unexpectedly in connection with natural disasters, famines, wars and conflicts and involving a different kind of approach, implementation and logistical strategy from cooperation for development in a general sense.
As regards areas of work, there are some particular interests that could be mentioned:
- 1.
Research
The 2013 World Health Report drew attention to the need to support research, including underpinning research that may lay the foundation for research for universal health coverage.34
Research can provide knowledge for addressing health problems in low-income countries. Bassatt et al.35 remind us that research aimed at preventing or treating the diseases most closely related to poverty is not subject to the same rules, even though in absolute terms such diseases may represent a disproportionate share of the total burden of disease.
Another result obtained from research, as already mentioned, was the 2006 growth and development standards,5 which confirm scientifically that it is possible for all the children in the world to grow up with smaller anthropometric and general development differences at the population level than had been thought, if they are offered the necessary care.
- 2.
Training and knowledge transfer
Training is essential in the area of child health. Acquiring appropriate competencies, abilities and skills leads to significant and long-lasting success.
Spanish universities are also contributing in terms of academic cooperation in the area of health, and this may help to enhance quality of life. However, the absence of a specific curriculum related to global health in faculties of Medicine or during specialist training in Paediatrics is a shortcoming that we must urgently remedy.36
- 3.
Care work
Perhaps the most common and visible form of cooperation in child health is engagement in care tasks.
Many of the concerns of Spanish paediatricians in relation to cooperation on the ground are channelled through their involvement in specific projects led by NGOs with more or less experience in countries in various continents, for short periods, and in some cases they take on greater responsibilities for longer periods. Occasionally the National Health System, through the corresponding organisations that provide health care facilities in some autonomous communities in Spain, helps some paediatricians to join other health services in low-income countries for a certain period, usually just a few months. Humanitarian aid in emergency or disaster situations represents another setting in which paediatricians can participate on an urgent basis.
Cooperation, international health and global health are relatively recent topics for Spanish paediatrics, but this is not the case in other countries. To give an example, nearly twenty years ago 25% of the training programmes for residents in the United States, Puerto Rico and the Caribbean already included optional subjects in global health.37
In a survey carried out by the AEP's International Cooperation Group with the participation of over 750 interested paediatricians, only 16% had received specific training and 28% had some experience on the ground.38
Some final thoughtsScientific knowledge of the real conditions in which the world child population finds itself in the health field and the factors that affect survival with dignity must be put to good use. A little over a decade ago there were already calls for knowledge to be translated into action for children's survival.11
Paediatricians must have basic training in global health and must know the specific problems affecting the child population in which they are going to intervene.
Ongoing care at all stages of life or of the prospective lifespan is needed: treating adolescents, pregnant women, newborns, infants in the neonatal period and subsequently in a range of settings – home, family, community, health services, both primary care and hospital – and establishing the appropriate referral systems.39
As paediatricians we must contextualise the space for international cooperation in child health, beyond the lack of an appropriate health care response to illness. In a situation of poverty, children will be particularly affected. We must analyse the determinants of child health and their direct and indirect influences; otherwise we will be demonstrating that we are unaware of the problem, its causes and the possible sustainable solutions, as we have pointed out on other occasions.40
We must remember that health inequity is an unnecessary, avoidable and unjust difference in health, in a broad sense, not only in terms of access to the health care system. We must incorporate determinants of health, without neglecting to promote support for health care establishments and trying to strengthen them, contributing to their effectiveness and sustainability.26
The safety and welfare of mothers has a decisive influence on the survival of children. The mother-child dyad must be addressed as a single whole.
Multi- and interdisciplinarity, combined with multi- and interprofessionalism, are essential, highlighting the decisive role of other professionals, including those who do not fall within the traditional definitions of “healthcare staff”.
Prevention and promotion of health must be a permanent guiding principle, because of their proven impact and contribution to the sustainability of success.
In addition, we must draw attention to the influence of malnutrition on the present and future burden of disease in children under two, women of reproductive age and pregnant women.21 And we must highlight the window of opportunity or “thousand days” (from conception until the child reaches the age of two) as a key period for intervention.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sobrino Toro M, Riaño Galan I, Bassat Q, Perez-Lescure Picarzo J, de Aranzabal Agudo M, Krauel Vidal X, et al. Salud infantil y cooperación internacional: una aproximación pediátrica. An Pediatr (Barc). 2015;82:367.