To describe the clinical and epidemiological features, management, and follow-up of child abuse suspicions diagnosed in the Paediatric Emergency Unit.
MethodsA single-centre, observational and retrospective study was conducted between 2008 and 2017. Clinical, epidemiological and follow-up data were collected in those patients younger than 16 that were reported as child abuse suspicions. A descriptive and analytic study was performed, as well as a bivariate and multivariate analysis.
ResultsA total of 404 out of 570,648 emergency patients (0.07%) were diagnosed with potential abuse. Physical abuse was the most frequent kind of abuse (40.3%). The median age was 4.3 years (IQR 1.6–10.2), and 55% were girls, with sexual abuse being more common in them (OR 3.71; 95% CI: 2.23–6.17), and physical abuse more frequent in boys (OR 1.72; 95% CI: 1.15–2.57). A total of 89 patients (22%) required admission. Age and type of abuse were independently associated with risk of admission. More than half (56%) of the cases required additional follow-up, with sexual (OR 3.98; 95% CI: 1.93–7.03) and emotional abuse (OR 4.93; 95% CI: 1.82–13.35) requiring more mental health follow-up, and physical abuse requiring more social services follow-up (OR 4.39; 95% CI: 1.61–11.98).
ConclusionsIn our study, child abuse is more frequent in pre-school children. Age and type of abuse are associated with the need of admission. The kind of follow-up is determined by the type of abuse.
Describir las características clínico-epidemiológicas, el manejo y el seguimiento de las sospechas de maltrato infantil diagnosticadas en Urgencias Pediátricas.
MétodosEstudio observacional, unicéntrico, y retrospectivo realizado entre 2008 y 2017. Se recogieron datos clínicos, epidemiológicos y de seguimiento de los menores de 16 años diagnosticados de sospecha de maltrato. Se realizó un análisis descriptivo y analítico, bivariante y multivariante.
ResultadosSe consideró potencial maltrato en 404 pacientes de 570.648 urgencias atendidas (0,07%). El maltrato físico fue el más frecuente (40,3%). La mediana de edad fue 4,3 años (RIC 1,6-10,2). El 55% fueron niñas, siendo en ellas más frecuente el abuso sexual (OR 3,71; IC95%: 2,23-6,17), y el maltrato físico más común en varones (OR 1,72; IC95%: 1,15-2,57). Un total de 89 pacientes (22%) precisaron ingreso. La edad y el tipo de maltrato se relacionaron de forma independiente con el riesgo de hospitalización. El 56,4% precisó seguimiento adicional; el análisis multivariable mostró mayor seguimiento por Salud Mental en los casos de abuso sexual (OR 3,98; IC95%: 1,93-7,03) y maltrato emocional (OR 4,93; IC95%: 1,82-13,35), y por servicios sociales en los maltratos físicos (OR: 4,39; IC95%: 1,61-11,98).
ConclusionesEn el presente estudio, el maltrato infantil es más frecuente en preescolares. La edad y el tipo de maltrato predicen la necesidad de hospitalización. El tipo de seguimiento está condicionado por el tipo de maltrato padecido.
Child abuse continues to be an underdiagnosed health problem that has gained considerable prominence in recent years.1 It is defined by the Centre International de l’Enfance (International Children's Centre) of Paris as any action, omission or neglect, not accidental, that deprives a child of his or her rights and wellbeing, threatening or interfering with his or her normal physical, psychological or social development, committed by individuals, institutions or society itself.2
The management of this problem is complex, and paediatric emergency services play a key role as a frequent entry point to health care for affected patients. The diagnosis and management of child abuse poses a significant challenge, as it is necessary to identify which situations require immediate intervention to guarantee the protection of the minor, managing the associated physical, psychological and social problems in cooperation with other professionals and implementing a protocol3 to prevent potential physical and psychiatric sequelae and a negative impact on development in these patients in the short and the long term.4,5
The magnitude of this problem in Spain has been reflected in official statistics published by the World Health Organization (WHO) and the Spanish Ministry of Health,6,7 and its epidemiology has been described in various studies, such as those by Sabaté Rotés et al.8 or Trenchs Sainz de la Maza et al.9 However, the time frame of these studies is narrow, and there are no studies describing the management of these patients in emergency care services beyond immediate intervention or hospital admission.10,11 Since child abuse requires a multidisciplinary approach, and given the number of detected cases and the key role played by emergency services, we considered it essential to gain knowledge of the outcomes in these patients, the follow-up services that are offered and whether the clinical and epidemiological characteristics at the time of initial care are associated with the approach to management and with physical and psychosocial outcomes.
The aim of our study was to describe the epidemiology of suspected cases of child abuse in our region, and to analyse their management in the emergency department and the subsequent follow-up in relation to their clinical and epidemiological characteristics.
Materials and methodsWe conducted a single-centre retrospective, observational and analytical study in children aged less than 16 years identified as possible subjects of child abuse that were managed at the Paediatric Emergency Department (PED) of a tertiary care hospital in the Autonomous Community of Madrid between January 2008 and December 2017. The study was approved by the Clinical Research Ethics Committee of the hospital. The diagnosis of child abuse was established by the filing of a child abuse report form with the government of the Autonomous Community of Madrid according to the criteria established by the Observatorio de la Infancia (Observatory on Childhood).12 We collected clinical and epidemiological data from the health records of the patients and the report forms, as well as follow-up data from primary care, the social work team and the different specialists involved in the subsequent follow-up. The epidemiological data we collected included patient age and sex, the reason for visiting the PED, who accompanied the patient, the reason for suspecting abuse and the relationship with the suspected perpetrator, with data for the last 3 variables collected if it was recorded in the emergency department discharge summary. We categorised abuse following the guidelines proposed by the Working Group on Child abuse of the Observatorio de la Infancia,12 differentiating between physical abuse, emotional abuse, neglect and sexual abuse, and allowed the recording of more than one type of abuse identified simultaneously in the included cases.
We collected data on patient destination after discharge, the reason for hospital admission and department of admission, and the need for the child to be taken into the custody of the autonomous community government; whether reports were filed with various legal authorities, and data on the subsequent follow-up (social, medical, legal and psychological/psychiatric). We defined social follow-up as referral from the PED or the hospital social work department to the Department of Social Services of the Autonomous Community of Madrid or to Child Protective Services, medical follow-up as the scheduling of successive outpatient visits related to the abuse, and psychological/psychiatric follow-up as documentation of involvement of the Mental Health Clinic in the follow-up records of the emergency department, social work department or primary care. We defined legal follow-up as evidence, obtained either through the direct referral from the emergency department, primary care or inpatient services to the judiciary, juvenile prosecution or forensic specialists or of subsequent contact through the hospital social work department with these parties, that any of these institutions were involved in the management of the suspected abuse at any time following the patient's initial visit to the emergency department.
We performed the statistical analysis with the software SPSS version 20. In the descriptive analysis, we summarised the quantitative variables with asymmetrical distributions as medians and interquartile ranges (IQRs), and qualitative variables as absolute frequencies and percentages. For the bivariate analysis, we used the Pearson chi square test to compare proportions. We used logistic regression for the multivariate analysis. We defined statistical significance as a p-value of less than 0.05.
ResultsIn the total 570,648 emergency visits managed during the period under study, 404 corresponded to cases of suspected child abuse (7 per 100,000 visits, 95% CI, 0.06–0.08%). The most frequent type of abuse was physical abuse (40.6%), followed by neglect (35.1%), sexual abuse (25.5%) and emotional abuse (7.4%). The median age of these patients was 4.3 years (IQR, 1.6–10.2) and abuse was most frequent in the group of children aged 1–5 years (38.9%). Table 1 presents data on the age and sex of the patients and the type of abuse.
Type of abuse by sex and age. Data presented as absolute frequencies and percentages.
| Total (N=404) | Type of abuse (N=404) | ||||
|---|---|---|---|---|---|
| Physical 164 (40.6%) | Neglect 142 (35.1%) | Sexual 103 (25.5%) | Emotional 30 (7.4%) | ||
| Sex | |||||
| Male | 182 (45%) | 86 (47.2%) | 73 (40.1%) | 22 (12%) | 11 (6%) |
| Female | 222 (55%) | 78 (35.1%) | 69 (31%) | 81 (36.5%) | 19 (8.5%) |
| Age | |||||
| <1 year | 79 (19.6%) | 43 (54.4%) | 35 (44.3%) | 1 (1.2%) | 4 (5.1%) |
| 1–5 years | 157 (38.9%) | 55 (35%) | 62 (39.5%) | 50 (31.8%) | 4 (2.5%) |
| 6–10 years | 63 (15.6%) | 21 (33.3%) | 17 (27%) | 18 (28.5%) | 12 (19%) |
| 11–16 years | 105 (25.9%) | 45 (42.8%) | 28 (26.6%) | 34 (32.3%) | 10 (9.5%) |
Sexual abuse was suspected more frequently in girls (OR, 3.71; 95% CI, 2.23–6.17) while physical abuse was more frequent in boys (OR, 1.72; 95% CI, 1.15–2.57). Of all the emergency visits where abuse was suspected, 57.2% had been made for reasons other than the abuse. The abuse was suspected during the history taking in 68.3% of cases, during the physical examination in 20.3%, and after performance of diagnostic tests in 8.4%. In 59.3%, the suspected perpetrator was one of the parents.
Eighty-nine patients (22.0%) required hospital admission, 18.8% of them for the purpose of protecting the child and the remaining 81.2% for observation or treatment. Of the total of admissions, 82.9% were to a hospital ward or the neonatal intermediate care unit, and 17.1% to the intensive care unit (ICU), and the most frequent reason for admission to the ICU was acute intoxication. None of the patients died. The group at highest risk of admission corresponded to infants aged less than 1 year (OR, 2.01; 95% CI, 1.10–3.66). The multivariate analysis found an independent association of age (OR, 0.928; 95% CI, 0.876–0.983) and the type of abuse with the risk of hospitalisation in the logistic regression model: sexual abuse was associated with a lower risk of admission (OR, 0.26; 95% CI, 0.08–0.72) and neglect with a higher risk (OR, 1.86; 95% CI, 1.07–3.22). The suspicion of abuse on the grounds of diagnostic tests was also associated with a higher risk of admission (OR, 6.49; 95% CI, 2.98–14.17). Of all the patients in whom abuse was suspected, 7.4% became wards of the Autonomous Community of Madrid and 4.4% were taken to an emergency shelter.
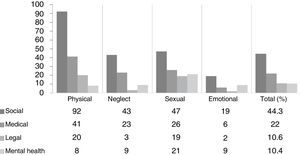
In all cases in which a report was filed, the social work department contacted primary care services. Furthermore, 56.4% of the patients required some type of additional follow-up, most frequently by social services (44.3%), followed by medical follow-up (22.3%), legal follow-up (10.6%) and psychological/psychiatric follow-up (10.4%). Fig. 1 represents the type of follow-up for each type of abuse. The subset of patients with the highest proportion of patients in follow-up was the group aged 11–16 years (75.2%), followed by children aged 6–10 years (63.5%). After correcting for potential confounders (age and sex), the multivariate analysis showed that follow-up by mental health services was more frequent in cases of sexual abuse (OR, 2.61; 95% CI, 1.36–5.02) and of emotional abuse (OR, 4.93; 95% CI, 1.82–13.35), while follow-up by social services was more frequent in cases of physical abuse (OR, 1.94; 95% CI, 1.29–2.91) and less frequent in cases of neglect (OR, 0.46; 95% CI, 0.30–0.72).
DiscussionWith this work, we aimed to get an overview of the epidemiology, management and follow-up of cases of suspected child abuse detected in the paediatric emergency department. The incidence of child abuse and the distribution of affected patients by sex and age were similar to those reported in previous studies conducted in Spain.8,9 In this study, the most frequent type of abuse was physical abuse, followed by neglect and sexual abuse, while in other studies neglect is not as prevalent. This could be related to the high level of suspicion for this subtype in our hospital, as our emergency care team has a designated point person for child abuse that is informed of all the suspected cases and in charge of coordinating the care and follow-up of these patients and to educate the rest of the staff on the subject. As observed in previous studies, emotional abuse was clearly the least reported type, but the data probably does not reflect its real incidence, as in many cases it is harder to detect and this is also the type that is the least likely to lead to emergency visits. The association between sex and type of abuse was consistent with the pattern described in the previous literature.
In more than half of the cases, the reason for the emergency visit was not the abuse, and in most instances abuse was suspected during the history taking, which highlights the vital importance of taking a careful history and of keeping a high level of suspicion of child abuse. Furthermore, in more than half of the cases the suspected perpetrator was a parent, which suggests that most instances of abuse occur in the household.8,10 Given the key role played by emergency departments in the detection and subsequent reporting of child abuse, it seems necessary to continue striving to provide adequate training and to raise awareness in all health professionals involved in emergency care, implementing strategies aimed at ensuring the safety of minors and preventing the potential deleterious consequences of abuse.2,3
The morbidity resulting from abuse is greater in the first years of life, as the medical literature has established that newborns and children aged less than 2 years are more likely to require hospital admission10 and intensive care.11 However, this phenomenon is not exclusive to injury due to child abuse, as studies on unintentional injuries13 and poisonings14 have reported similar age distributions. In our study, we found that the probability of hospital admission was highest in infants aged less than 1 year and decreased with increasing age, and that this pattern varied based on the type of abuse. The fact that our findings differed in this latter aspect from those of Trenchs Sainz de la Maza10 (whose study found the highest proportion of admissions in cases of physical abuse) and that the proportion of overall admissions in our hospital was slightly higher (22%) compared to the study just mentioned and other previous studies15 could be explained by the higher frequency of detection of neglect in our study—including cases of poisoning, which are generally associated with a higher proportion of hospital admission14—and to the fact that cases of sexual abuse require observation and treatment less frequently and instead usually lead to discharge with referral to other governmental institutions for legal reasons.
To date, there were no studies conducted in Spain that analysed the referral and follow-up of these patients from the emergency department. In this regard, we found that more than half of the patients in whom abuse was suspected in our hospital were subject to some type of follow-up in addition to primary care services, most frequently through social services, especially in cases of physical abuse. The filing of child abuse report forms12 and the coordination of care with social services are useful to ensure follow-up at the primary care level and, if needed, by other institutions. Among the latter, and in addition to social services, mental health clinics are very important, especially in cases of sexual or emotional abuse, which frequently require psychological support. Given the need to individualise care, the role of emergency clinicians is essential, as they are responsible for initiating and ensuring this follow-up when needed, adapting it to the type of abuse and the characteristics of the patient. Additional prospective studies are required in our region that investigate this follow-up over longer periods of time to establish whether these patients experience a higher incidence of social or mental health problems in the future.16
There are limitations to this study, including its retrospective design, which made the collection of follow-up data more difficult, and that it was conducted in a single centre. Furthermore, the cases included in the study were classified as “suspected abuse”, but the difficulties involved in the diagnosis and management of child abuse make it impossible to confirm or refute that abuse actually existed. The latter is an intrinsic limitation on the literature on this subject, and we do not believe that it would have an impact on the initial approach taken at the level of emergency services or on the validity of our data. Another limitation, this time involving the collection of legal follow-up data, was that we did not have access to data from the legal system, which may have led us to underestimate the proportion of cases with legal involvement, as some children may not have been referred to legal institutions directly from emergency services, primary care, inpatient services or social services.
Based on our findings, we conclude that in our region suspected child abuse is most frequent in the pre-school age, that age and the type of abuse are determinants of the need of hospital admission, that these patients frequently require a close follow-up, preferably by social services, and that the type of follow-up should be based on the type of abuse inflicted and individualised to meet the specific needs of these patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Solís-García G, Marañón R, Medina Muñoz M, de Lucas Volle S, García-Morín M, Rivas García A. Maltrato infantil en Urgencias: epidemiología, manejo y seguimiento. An Pediatr (Barc). 2019;91:37–41.
Previous presentations: This study was presented as a long oral communication at the XXIII Annual Meeting of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine), 2018.