The SARS-CoV2 pandemic dimension has affected the Hospital Pediatrics Medicine assistance in our country. New challenges generated by COVID-19 require a series of proactive measures, based on existing scientific knowledge and standards of good practice, that allow the Pediatric Hospital services readiness and operability. Hospital Internal Pediatrics, as responsible of integral care of the hospitalized child, plays a leading role in the new hospital model emerging from this crisis. This review analyzes the impact of the current SARS-CoV2 epidemic on pediatric care, and perspective of new COVID-19 outbreaks in coexistence with other viral infections. Changes secondary to pandemic involved in Hospital pediatric units must be analyzed, and how to prepare for future epidemics, also the involvement of pediatric units in adult care and the possible opportunities for improvement. Assistance of patients with chronic complex conditions in epidemic circumstances, safety aspects, opportunities for teaching and ethical considerations are reviewed. The Spanish Society of Hospital Pediatrics Medicine offers with this article a series of resources for Internal pediatric Medicine practitioners responsible to face next challenges in pediatric hospitalization units.
La dimensión de la pandemia por SARS-CoV2 ha afectado a la organización asistencial de la Pediatría Hospitalaria de nuestro país. Los nuevos retos generados por la COVID-19 exigen una serie de medidas proactivas basadas en los conocimientos científicos existentes y las normas de buena práctica, que permitan la preparación y la mayor operatividad de los servicios pediátricos hospitalarios. La Pediatría Interna Hospitalaria, como responsable de la atención integral del niño hospitalizado, tiene un papel principal en el nuevo modelo de hospital surgido de esta epidemia. En la presente revisión se analiza la repercusión pediátrica que ha tenido la epidemia por SARS-CoV2 y la preparación ante futuros rebrotes, en posible coexistencia con otras infecciones virales. Se revisa también la implicación de las unidades pediátricas en la asistencia de adultos y la atención de pacientes crónicos complejos y se ofrecen recomendaciones sobre aspectos de seguridad, consideraciones éticas y docencia de los futuros pediatras durante la crisis. La Sociedad Española de Pediatría Hospitalaria (SEPHO) pretende con este documento ofrecer a los pediatras internistas hospitalarios una serie de reflexiones y recursos de utilidad en un escenario con muchas incertidumbres.
Mankind is facing a serious crisis due to the rapid spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has already caused 400 000 deaths,1 with millions of people currently infected and unpredictable economic and social consequences.
In Spain, the response to this health crisis has led to the implementation of extraordinary measures in care delivery.2 The magnitude of the pandemic has also affected the organization of inpatient paediatric care. In the wake of this pandemic, a substantial proportion of paediatric hospitalists have faced adjustments that would have seemed inconceivable only a few months before, such as the management of adult patients by paediatricians, the relocation of units and health care professionals, shut down of paediatric departments to expand adult care services, the centralization of paediatric care in a few departments of paediatrics… These decisions have been made in a rush due to the rapid spread of coronavirus disease 2019 (COVID-19) caused by the SARS-CoV-2 and to prevent the collapse of the health care system.
The pandemic has challenged many of the principles of paediatric inpatient care that seemed unquestionable until now. A proactive approach is replacing the former “reactive” approach to ensure readiness and improve the efficiency of inpatient paediatric services in a crisis situation. We must use the lessons learned in this pandemic to establish a series of recommendations susceptible of revision based on current scientific evidence and good clinical practice standards. With its integral approach to the care of hospitalised paediatric patients, the speciality of inpatient paediatrics will play a prominent role in the development of the new model of inpatient care that will emerge from the incipient changes spurred by this crisis.
With this document, the Sociedad Española de Pediatría Hospitalaria (Spanish Society of Inpatient Paediatrics, SEPHO) aims to offer paediatric hospitalists a series of useful reflections and resources to aid them in a scenario rife with uncertainty.
Impact of COVID-19 on inpatient paediatric care. Upcoming care delivery scenariosCoronavirus disease 2019 in children contributed slightly to the collapse of the health care system experienced in the early months of the pandemic.3 In the paediatric population, the hospitalization rate and the incidence of complications due to SARS-CoV-2 infection is lower compared to other infectious pathogens4 and to SARS-CoV-2 infection in other age groups.5 Nevertheless, paediatricians have faced a broad spectrum of presentations, including particularly severe forms of disease often found in patients with underlying conditions.6 An additional challenge due to the novelty of the disease is the scarcity of scientific evidence on the management of severe forms of disease in the paediatric population, which may have been influenced by the evidence on the management of adult patients.
In the early phase of the pandemic, care delivery in paediatric units may have been affected not only by paediatric caseloads, but also by the redistribution of resources due to the saturation of hospital services, the considerable spread of the virus among health providers and the curtailment of what may be considered non-essential care. This situation, if sustained, may carry a high opportunity cost as regards other health problems, especially if measures are not taken to minimise its medium- and long-term impact. As paediatricians, we must ready ourselves to face a new scenario that will be more of a marathon than a second sprint.7
Confinement and social distancing, key measures in the control of the spread of SARS-CoV-2 during the first wave,8 may have also had an impact on all other infectious diseases in the paediatric age group. These measures, along with the suspension of a large part of elective hospital-based services, have led to a striking decline in occupancy in many paediatric units. However, the suspension of all work- and school-related activities can hardly be sustained indefinitely,9 and activities will need to resume gradually under epidemiological surveillance.
Future inpatient care will be conditioned by the need to maintain social distancing measures inside hospitals, which may affect the structure of care delivery, teams and units. This crisis has created an opportunity to make changes to the classic model of inpatient care. Resources that were already available, such as hospital-at-home and telemedicine services, will grow in importance and become part of everyday clinical practice.
Forecasts to model the spread of COVID-19 will be crucial in anticipating what will be required for paediatric services to be prepared. Current models suggest that the initial wave may be followed by new epidemic peaks in the upcoming 24 months10 that will vary in intensity between geographic regions and possibly exhibit a seasonal pattern, which will unquestionably have an impact on health care demand and resources. We must develop an adaptive model of hospital-based care that can ensure continued management of all other conditions with the same quality of care that was available before this health crisis, along with measures for contention of new epidemic outbreaks of SARS-CoV-2.
Preparing for the concurrence of COVID-19 and seasonal epidemics of viral diseaseIn the period before the SARS-CoV-2 spread, there may have been a degree of complacence in the belief that the epidemic would not reach us, or that it would have a lesser impact, which may have contributed to the delay in implementing certain control measures.11 We would be making another mistake if we did not contemplate the probability of the coexistence of COVID-19 with seasonal epidemics by other viruses, such as respiratory syncytial virus (RSV) or the flu, and did not start right away the necessary preparations to confront such a scenario.12
But it is not enough to plan a series of measures exclusively aimed at the management of seasonal infectious diseases. It is also important to ensure the continuity of all other medical services, with an efficient use of resources and the establishment of a safe environment for patients, families and health care workers.13
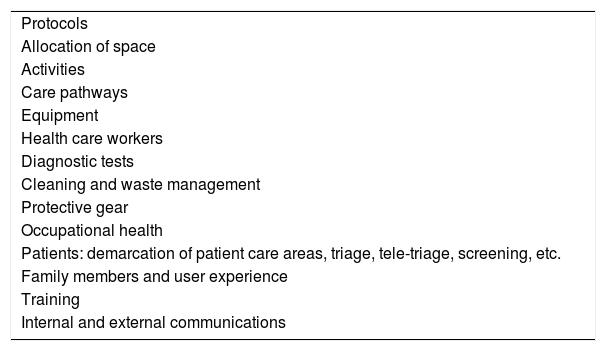
In light of this, it would be advisable to form, as was done at the beginning of the pandemic, hospital crisis committees composed by representatives responsible for the management of operations in different care areas.14Table 1 presents some of the aspects to be discussed in the meetings of the committee.
Qualitative aspects to be considered by crisis preparedness and response committees.
| Protocols |
| Allocation of space |
| Activities |
| Care pathways |
| Equipment |
| Health care workers |
| Diagnostic tests |
| Cleaning and waste management |
| Protective gear |
| Occupational health |
| Patients: demarcation of patient care areas, triage, tele-triage, screening, etc. |
| Family members and user experience |
| Training |
| Internal and external communications |
During the first wave of the pandemic there was no shortage of paediatric intensive care beds, contrary to what happened in adult care. But given the annual impact of RSV and flu on critical care units15,16 and the potential for new waves of COVID-19, we must ensure adequate availability of resources for all affected patients.
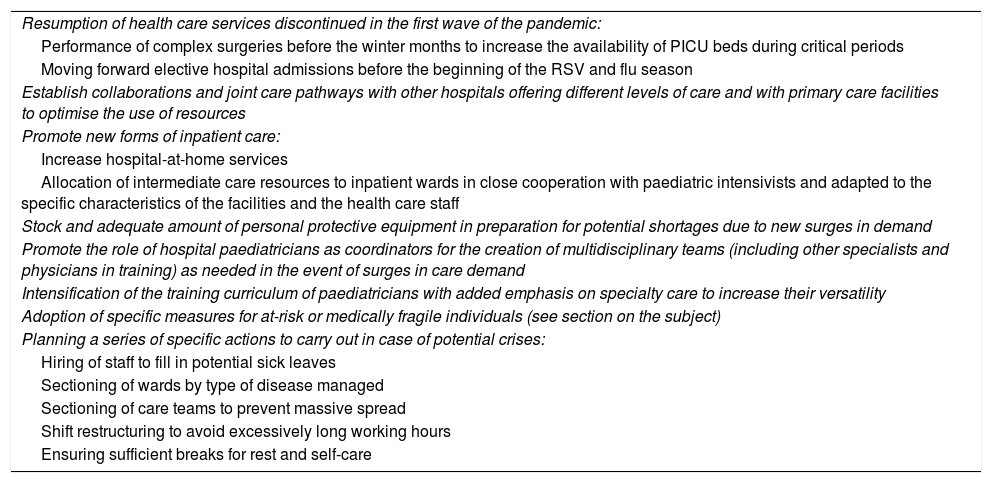
A successful management of all these issues requires the implantation of a series of preparedness measures affecting every aspect of hospital organization. Table 2 proposes some organizational strategies that may be useful in this context.17–19
Measures to guarantee the continuity of essential medical care for upcoming respiratory infection epidemic seasons in the context of SARS-CoV-2.
| Resumption of health care services discontinued in the first wave of the pandemic: |
| Performance of complex surgeries before the winter months to increase the availability of PICU beds during critical periods |
| Moving forward elective hospital admissions before the beginning of the RSV and flu season |
| Establish collaborations and joint care pathways with other hospitals offering different levels of care and with primary care facilities to optimise the use of resources |
| Promote new forms of inpatient care: |
| Increase hospital-at-home services |
| Allocation of intermediate care resources to inpatient wards in close cooperation with paediatric intensivists and adapted to the specific characteristics of the facilities and the health care staff |
| Stock and adequate amount of personal protective equipment in preparation for potential shortages due to new surges in demand |
| Promote the role of hospital paediatricians as coordinators for the creation of multidisciplinary teams (including other specialists and physicians in training) as needed in the event of surges in care demand |
| Intensification of the training curriculum of paediatricians with added emphasis on specialty care to increase their versatility |
| Adoption of specific measures for at-risk or medically fragile individuals (see section on the subject) |
| Planning a series of specific actions to carry out in case of potential crises: |
| Hiring of staff to fill in potential sick leaves |
| Sectioning of wards by type of disease managed |
| Sectioning of care teams to prevent massive spread |
| Shift restructuring to avoid excessively long working hours |
| Ensuring sufficient breaks for rest and self-care |
Due to the considerable number of adults affected by the first wave of the pandemic and the threat of a potential collapse of the health care system, many hospital paediatric teams have been sharing material and human resources and physical space to provide adult care.20 A few children’s hospitals and paediatric teams have taken responsibility for all paediatric admissions referred from other facilities so that paediatric care areas in referring hospitals can be devoted to adult care. In other instances, paediatric departments have managed adult patients, and paediatric care staff have been redeployed to support adult COVID-19 units.
We ought to evaluate carefully the unprecedented measures that had to be implemented on an urgent basis and determine which could be improved. We need to consider whether in the future, in a similar situation requiring the reallocation of paediatric care resources to adult care, the response would be agile, safe and efficient.21 In this hypothetical scenario, it is also important to guarantee continuity of care in the paediatric population, especially for at-risk patients with acute disease or complex medical conditions requiring specialised treatment, providers and equipment.22
Some of the potential measures to consider23 include the creation of multidisciplinary teams of paediatricians and professionals in adult care to anticipate patient needs, create treatment plans and follow-up cases. Depending on the circumstances, it may be appropriate to expand the admission criteria of paediatric units to include adult patients with COVID-19 aged up to 30 to 35 years without comorbidities or with chronic diseases with onset in childhood or adolescence. Another possibility would be to consider hospitalization of young adults with conditions commonly found in the paediatric population in paediatric care settings. Adults with COVID-19 are at higher risk of developing arrythmias, coronary artery disease and stroke, so older adults or adults with a previous history of these diseases should not be hospitalised in a paediatric setting. Intrahospital medical alert systems specific to the adult patient population must be set up along with the establishment of adult critical care rapid-response teams.
Patient and provider safety during epidemicsThe number of health care workers that have been infected during this pandemic has exposed potential gaps in epidemic preparedness and reinforced the importance of protective measures. Preparation for similar situations in future years requires the development of measures to guarantee the safety of patients and health care workers during care delivery.
Two interdependent types of factors are at play in safety: institutional factors and personal factors. The hospital must provide the organizational structure and resources necessary to facilitate the work of the health care staff, and have in place an outbreak protocol that can be quickly implemented when necessary.24,25 The protocol must address the following aspects:
- •
Setting up exclusive wards for confirmed or suspected cases with rooms allowing the application of required isolation measures (including negative pressure as needed).
- •
If this is not possible, section off spaces and establish separate care teams in the ward to be dedicated exclusively to suspected/confirmed cases, on one hand, and to all other cases on the other.
- •
Maintain an adequate supply of personal protective equipment (PPE).
- •
Train health care staff on personal protection (for instance, the correct use of PPE).
- •
Allow organizational changes and internal mobility of staff.
- •
Facilitate the implementation of social distancing measures within the staff.
- •
Perform enough tests in the health care staff to ensure early detection of infection.
- •
Provide psychological support to staff as needed.
Health care workers play a key role in their own safety and the safety of the patient. It is important to raise awareness of importance of personal protection measures to minimise transmission in and out of hospital.26 Some of the recommendations are:
- •
Maintaining a safe distance from the rest of the staff (>1.5–2 m).
- •
Replacing the usual face-to-face staff meetings (case conferences, shift-change handoffs, huddles…) with online meetings.
- •
Frequent handwashing.
- •
In case of droplet transmission, refraining from touching the face (mouth, nose and eyes).
- •
Training in the use (correct placement and removal) of PPE.
- •
At-home quarantine from the moment of detection of early manifestations for the period established by the specific recommendations for the infection in question.
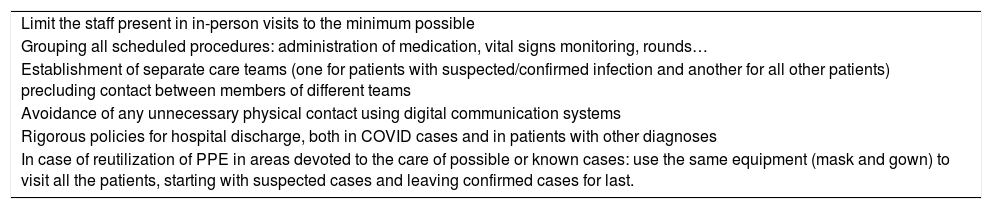
This pandemic has uncovered numerous barriers that increase the risk of hospital-acquired infection.27 One of the main barriers worldwide is the insufficient availability of PPE. This situation has led to an evaluation of the use of this protective gear28 and to the development of recommendations for personal protection and the rational use of PPE (Table 3).
Personal protection measures and rational use of personal protective equipment.
| Limit the staff present in in-person visits to the minimum possible |
| Grouping all scheduled procedures: administration of medication, vital signs monitoring, rounds… |
| Establishment of separate care teams (one for patients with suspected/confirmed infection and another for all other patients) precluding contact between members of different teams |
| Avoidance of any unnecessary physical contact using digital communication systems |
| Rigorous policies for hospital discharge, both in COVID cases and in patients with other diagnoses |
| In case of reutilization of PPE in areas devoted to the care of possible or known cases: use the same equipment (mask and gown) to visit all the patients, starting with suspected cases and leaving confirmed cases for last. |
We must also reflect on safety in relation to the treatment of SARS-CoV-2. The pressing need to find an adequate treatment for COVID-19 has led to the use of drugs of unproven efficacy in this disease or based on the results of preclinical studies.29 These drugs are not free of risk of potentially serious adverse effects, a risk that is currently accepted on account of the exceptional circumstances. The field of paediatrics is even more affected due to the scarcity of paediatric trials. Thus, paediatricians must also act with extreme caution and adhere to the current recommendations of experts and working groups of scientific societies.
The dramatic characteristics of this crisis (an infection that is novel and unknown in many ways, the saturation of health care facilities, the overwhelming workload of professionals…) and its impact on patient and provider safety call for the implementation of an integral risk management model in which every involved party prioritises safety. Mistakes made in the current crisis will provide important lessons for future epidemics.
Care of medically fragile patients in the COVID-19 eraThe significant increase in the number of children with complex chronic disease in recent years demands that hospitals have specific care protocols to manage this group of patients, including in exceptional situations like the current COVID-19 pandemic.
In infections by other coronaviruses, complex chronic disease constitutes a risk factor for a poor outcome in children,30 as occurs with other viral infections.31 Due to their vulnerability, paediatric guidelines for the management of COVID-19 provided specific recommendations for patients with serious underlying disease.32
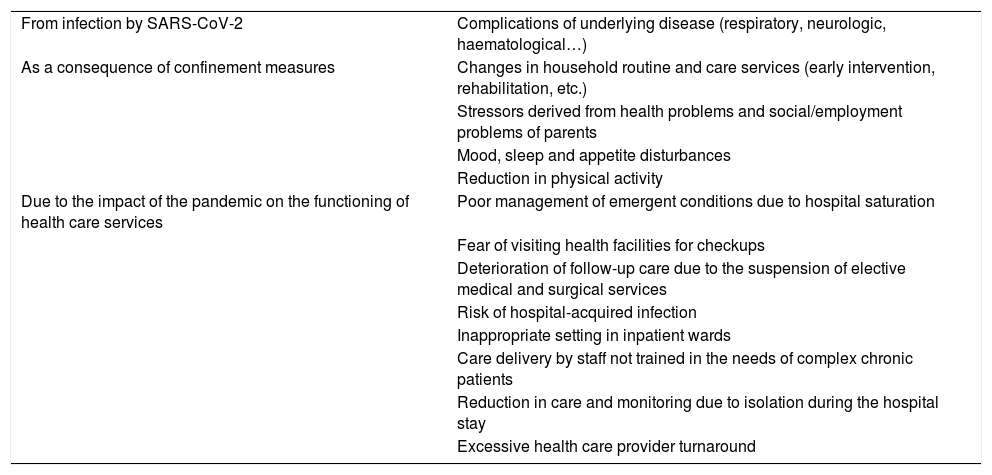
In addition to the infection by SARS-CoV-2, medically fragile patients may be affected by the impact of the pandemic crisis on society and the health care system (Table 4). A study conducted in Italy reported severe decompensations of underlying diseases and even deaths due to delays in seeking care out of fear of coronavirus.33
Main threats from the COVID-19 pandemic to patients with complex chronic disease.
| From infection by SARS-CoV-2 | Complications of underlying disease (respiratory, neurologic, haematological…) |
| As a consequence of confinement measures | Changes in household routine and care services (early intervention, rehabilitation, etc.) |
| Stressors derived from health problems and social/employment problems of parents | |
| Mood, sleep and appetite disturbances | |
| Reduction in physical activity | |
| Due to the impact of the pandemic on the functioning of health care services | Poor management of emergent conditions due to hospital saturation |
| Fear of visiting health facilities for checkups | |
| Deterioration of follow-up care due to the suspension of elective medical and surgical services | |
| Risk of hospital-acquired infection | |
| Inappropriate setting in inpatient wards | |
| Care delivery by staff not trained in the needs of complex chronic patients | |
| Reduction in care and monitoring due to isolation during the hospital stay | |
| Excessive health care provider turnaround |
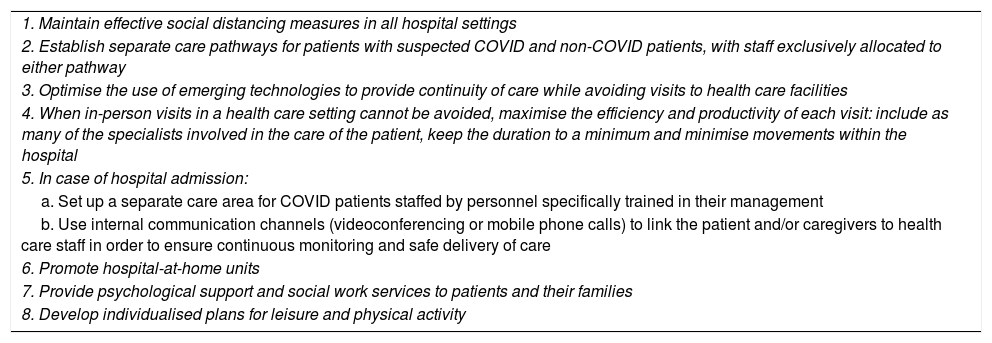
From a preventive standpoint, the experience gained in complex chronic disease units could be used to develop a series of recommendations to improve the care of these patients in the context of SARS-CoV-2 (Table 5).
Recommendations for the management of paediatric patients with complex chronic disease in the context of the SARS-CoV-2 pandemic.
| 1. Maintain effective social distancing measures in all hospital settings |
| 2. Establish separate care pathways for patients with suspected COVID and non-COVID patients, with staff exclusively allocated to either pathway |
| 3. Optimise the use of emerging technologies to provide continuity of care while avoiding visits to health care facilities |
| 4. When in-person visits in a health care setting cannot be avoided, maximise the efficiency and productivity of each visit: include as many of the specialists involved in the care of the patient, keep the duration to a minimum and minimise movements within the hospital |
| 5. In case of hospital admission: |
| a. Set up a separate care area for COVID patients staffed by personnel specifically trained in their management |
| b. Use internal communication channels (videoconferencing or mobile phone calls) to link the patient and/or caregivers to health care staff in order to ensure continuous monitoring and safe delivery of care |
| 6. Promote hospital-at-home units |
| 7. Provide psychological support and social work services to patients and their families |
| 8. Develop individualised plans for leisure and physical activity |
One of the challenges faced by hospital-based paediatrics in the current pandemic is finding the balance between caring for patients, restructuring services and continuing the education of medical students and residents-in-training.34 These two collectives are considered potential vectors of infection due to their rotation through different departments, which has led to the cancellation of many scheduled rotations.
Residents in paediatrics have contributed greatly to the management of paediatric patients and even adult patients in the current health crisis. However, the bedside education of residents in their early years of training may have been affected by the scarcity of PPE, in some cases limiting the chances to directly assess patients, a task that would have been performed by more seasoned professionals.
In this situation, we propose a few alternative educational approaches that could be useful for less experienced students and residents in the current or a future pandemic:
- •
Promotion of safe use by residents of information technology and electronic resources in the inpatient care and follow-up of patients.
- •
Practical workshops with mannikins to train in the performance of procedures while implementing all the required protective measures in cases of suspected infection.
- •
Drills to simulate transport of patients infected by SARS-CoV-2 from inpatient wards to intensive care units.
- •
Resources to promote professional conduct, leadership, teamwork and resilience.
- •
Round-table reviews of the literature on COVID-19.
Paediatric hospitalists must approach this situation as an educational opportunity for the purpose of preparing the next generation of professionals to manage future crises.35
Ethical considerations in the COVID-19 pandemicThe pandemic has generated very significant ethical dilemmas. The guidance for managing ethical issues in infectious disease outbreaks published in 2016 by the World Health Organization36 established the obligations of governments to respond to infectious disease outbreaks. Countries have obligations not only to persons within their own borders but also to the broader international community. An emphasis on geopolitical concerns rather than international cooperation may have contributed to the rapid global spread of SARS-CoV-2.
The medical code of ethics requires that physicians never abandon any patients needing their care, even in the event of disasters or epidemics.37 Naturally, paediatricians are driven to care for their patients, and they are only released from this duty in case their lives are at risk.38
As regards the uncertainty of some aspects of the treatment of COVID-19, the criteria for initiating treatment without an established indication are, besides the immediate impossibility of carrying out clinical trials, are evidence of safety from animal models, adequate risk-benefit analyses by research ethics committees and informed consent by patients or their legal guardians.
One of the aspects that raises the most concerning dilemmas in adult medicine is the allocation of care to individuals in a situation in which resources are scarce.39 The general guideline developed by the Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias(Spanish Association of Intensive and Critical Medicine and Cardiac Intensive Care)40 recommends prioritization based on saving the most life years and establishment of clear criteria for admission and discharge in the intensive care unit. The document called for the application of eligibility criteria and taking into account factors such as age, the presence of comorbidities, the severity of disease, organ compromise and reversibility. These issues are also relevant in the field of paediatrics. There is no guarantee that we will not be facing this situation at some point.
When confronted with challenging situations, it is important that we learn and then not forget. Mankind has always been subject to pandemics, and it will continue to be.
ConclusionThe management of this and other epidemic diseases in paediatric inpatient wards must be coordinated with the management of other health problems, especially in high-risk or complex patients. Some of the changes in paediatric clinical practice triggered by this pandemic will become permanent and be integrated in future models of paediatric inpatient care.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Alcalá Minagorre PJ, Villalobos Pinto E, Ramos Fernández JM, Rodríguez-Fernández R, Vázquez Ronco M, Escosa-García L et al. Cambios a partir de la COVID-19. Una perspectiva desde la pediatría interna hospitalaria. An Pediatr (Barc). 2020;93:343.