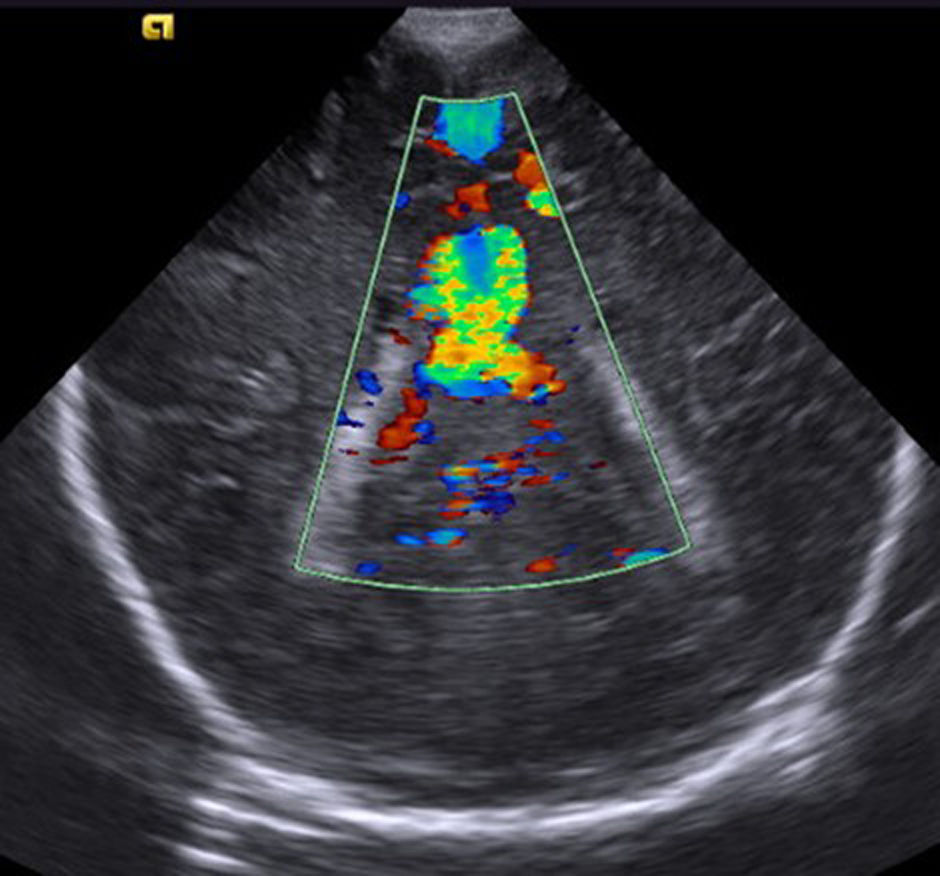
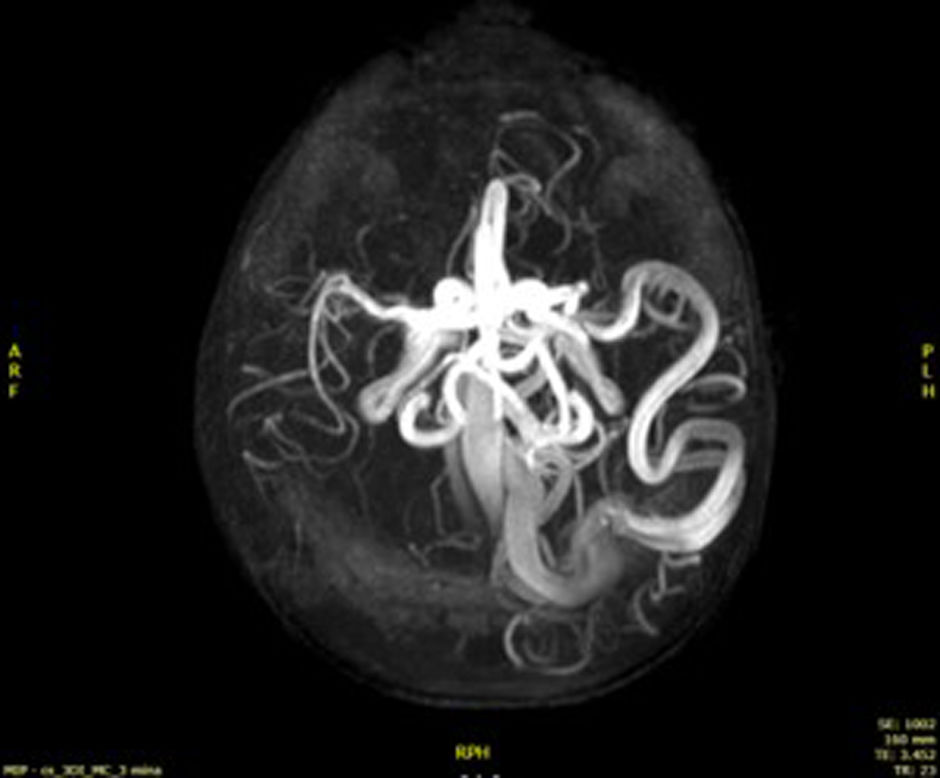
A male term newborn was transferred to a level IV neonatal intensive care unit due to severe pulmonary hypertension. Structural heart disease and infection were ruled out. The neonate required inotropic support, mechanical ventilation and nitric oxide. A cranial ultrasound examination revealed a hyperemic pattern and an anechoic area suggestive of an arteriovenous malformation (AVM) [Fig. 1]. A magnetic resonance angiogram of the brain confirmed a high-flow pial fistula draining to an enlarged cortical vein (Fig. 2). He underwent a partially successful percutaneous embolism followed by open surgery with removal of the entire fistula, but with hemodynamic instability due to brain hemorrhage and seizures, with subsequent clinical stabilization. The patient developed right hemiparesis but walks independently, has no seizures, and has two cutaneous vascular malformations (Fig. 3).
Targeted exome sequencing detected a pathogenic variant in the RASA1 gene, confirming the diagnosis of capillary malformation-arteriovenous malformation (CM-AVM) syndrome. The mother also tested positive and has two angiomatous maculae, but no other malformations.
Capillary malformation-arteriovenous malformation syndrome is a recently described autosomal dominant disorder that affects vascular development.1 It presents with cutaneous malformations and can cause AVMs in various organs, including the brain. These may be asymptomatic or lead to seizures or death if they rupture.2 Genetic diagnosis enables monitoring of potential AVMs in affected individuals and family members.3
Previous meeting: These data have been presented as a printed poster at the 10th Congress of the European Academy of Paediatric Societies; October 17–20, 2024; Vienna.