Blake's pouch cyst is defined as a midline cystic malformation consisting of an posterior outpouching of the inferior medullary velum into the cisterna magna.1 It is attributed to the lack of fenestration of Blake’s Pouch, an embryological expansion of the posterior membranous area continuous with the fourth ventricle, which would normally give rise to the foramen of Magendie.2 Failed fenestration results in the lack of communication between the fourth ventricle and the subarachnoid space, which in turn can cause hydrocephalus.2 The differential diagnosis includes arachnoid cyst, mega cisterna magna and Dandy-Walker variant.2
Fenestration of the cyst is one the approaches proposed to treat the main complication of Blake’s pouch cyst, hydrocephalus. In children aged less than 1 year, fenestration is often unsuccessful and the patient requires placement of a ventriculoperitoneal shunt.1,3 Endoscopic third ventriculostomy is the treatment of choice.3
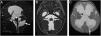
We present the case of a male infant aged 6 months assessed for macrocephaly of 2 month’s duration, born at 38 weeks of gestation and with no history of gestational or perinatal complications. The physical examination revealed that the infant was not able to support his head or roll, milestones that the mother reported he had achieved before the onset of the condition with hypoactivity and vomiting. She also denied any convulsive seizures since birth. Magnetic resonance imaging (MRI) allowed visualization of Blake’s pouch cyst associated with signs of intracranial hypertension (Fig. 1). We referred the patient for placement of a ventriculoperitoneal shunt.
Preoperative MRI in a male infant aged 6 months with severe tetraventricular hydrocephalus. (A) Sagittal image evincing patency of the cerebral aqueduct (white arrowhead) between the enlarged fourth ventricle and Blake’s pouch cyst (black star). Thin posterior cyst wall (white arrow) inferior to the slightly elevated and compressed lobules of the posterior vermis. Concavity of the floor of the third ventricle as a consequence of the cerebrospinal fluid outflow from the ventricles into the cisterns (black arrow). (B) Axial MRI evincing patency of the foramina of Luschka (white arrows). (C) Axial image showing hydrocephalus associated with periventricular interstitial oedema (white arrow) indicative of increased intracranial pressure at the level of the perforated septum pellucidum (black arrow).
Authors state that no economic support has been associated with the present study.
Conflicts of InterestAuthors declare no conflict of interest regarding the present study.