Pseudoangiomatous stromal hyperplasia of the breast (PASH) is a benign lesion of the mammary stroma that is relatively common in women of child-bearing age. Its presentation is variable, ranging from an incidental microscopic finding to the quick and massive enlargement of one or both breasts.1
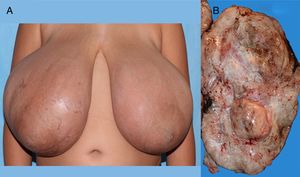
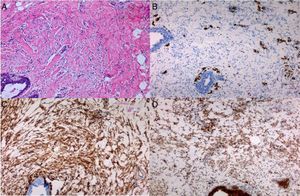
We present the case of a girl aged 10 years and 7 months with bilateral breast enlargement that started 5 months prior that was painful, accompanied by cutaneous eczema and cracks, without nipple inversion or secretions and without mammary lymphadenopathy. The patient experienced thelarche at age 9 years and 8 months, and menarche at 10 years and 6 months. There was no history of breast disease in the family. Her height was 147.4cm (+1.19 SD), her weight 59.3kg (+3.7 SD), and she had features corresponding to Tanner stage V. Each breast weighed approximately 2.5kg, the distance from the suprasternal notch to the right nipple was 43.5cm, and the distance from the notch to the left nipple was 41cm (Fig. 1A). The complete blood count, chemistry panel and hormone panel (thyroid function tests, oestrogen, progesterone and prolactin levels) were normal. An ultrasound examination of the breast revealed breast tissue of normal appearance housing multiple solid oval shapes with well-defined borders and homogeneous echogenicity, suggestive of fibroadenomas in both breasts, the biggest of which was in the left breast (33.6×60mm). A magnetic resonance imaging (MRI) scan of the breasts revealed multiple hypointense nodules in T1 images that were hyperintense in T2 images, occupying nearly the entire volume of the breast. Two biopsy samples of tissue were obtained that measured 2×2×1.2cm. Their cytological examination revealed marked sclerosis of the breast parenchyma, with isolated ducts and lobules lined by a mildly hyperplastic epithelium. The mammary stroma featured a pattern of interconnected slit-like spaces lined with spindle cells lacking atypia and mitotic figures (Fig. 2A). Immunohistochemical staining showed that the cells were negative for endothelial and lymphatic markers (CD31, WT1, D240), with a diffuse pattern of cells positive for CD34, BCL2 and SMA (Fig. 2B–D). These findings led to the diagnosis of PASH. The patient underwent surgery, with full resection of the lesion, removing masses that weighed 4200g (right breast) and 3200g (left breast), with maximum diameters of 35×25×10cm and 25×20×10cm, respectively. On gross examination, the resected tissue exhibited a fascicular architecture and multinodular hyperplasia (Fig. 1B). The histological examination revealed the same features as the cytological examination, confirming the diagnosis.
Pseudoangiomatous stromal hyperplasia of the breast was first described by Vuitch et al.2 It is a histological diagnosis and is characterised by the presence of a network of channels or slit-like spaces lined by spindle or ovoid cells without atypia resembling endothelial cells on a hypocellular and markedly hyalinised stroma.1 On immunohistochemical staining, the cells lining these vessel-resembling slits are negative for CD31, factor viii, cytokeratin and S100 (positive in endothelial cells), and positive for CD34, SMA and BCL2 (myofibroblast markers).3 In some cases, the tissue tests positive for oestrogen and progesterone receptors, which supports the currently dominant pathophysiological hypothesis: myofibroblasts proliferate due to an abnormal response to these hormones, which would explain the presence of this disease in premenopausal women, women that use oral contraceptives or postmenopausal women under hormone replacement therapy.4
This is a benign lesion, in most cases an incidental finding in the evaluation of a different breast problem. It may also present as a solitary palpable mass, with well-defined borders, similar to a fibroadenoma,4 as multiple nodules, or as a large diffuse mass. Approximately 14% of cases present with irregular borders and excessively rapid growth, which requires ruling out a malignancy. Talu et al.5 found areas of PASH in 37 of 412 biopsy breast tissue samples, associated with fibrosis in 46% of cases.
An ultrasound examination of the breast is the imaging test of choice in adolescents. In MRI scans of the breast, PASH appears as multiple masses that are hypointense in T1 images and hyperintense in T2 images, with irregular or microlobulated borders.6 However, the findings of imaging tests are nonspecific, and examination of biopsy samples is necessary to make a definitive diagnosis. The differential diagnosis must include fibroadenoma, based on the clinical and radiological features, and low-grade angiosarcoma (with infiltration and positive for vascular markers such as CD31 and factor viii) and phyllodes tumour, based on the histological features.1
Surgery is the first-line treatment if the patient is symptomatic or the lesion is growing rapidly. In localised forms, if the clinical manifestations, radiological features and histology suggest a benign course, a conservative approach with followup of the patient is recommended. Surgery options range from lumpectomy with broad margins (if the lesion is nodular) to mastectomy followed by reconstruction surgery.1
Massive bilateral PASH is a rare disorder during puberty. Ultrasound examination is the preferred imaging technique for assessment, and the diagnosis is based on histological features. Surgery is the recommended treatment.
Please cite this article as: Márquez Rivera M, Corredor Andrés B, Azorín Cuadrillero D, Muñoz Calvo MT, Argente J. Hiperplasia estromal pseudoangiomatosa mamaria bilateral. An Pediatr (Barc). 2018;89:309–311.