To identify clinical characteristics that may lead to the early identification of patients hospitalised for moderate-to-severe bronchiolitis with urine results associated with the syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Patients and methodsA prospective observational study was conducted, spanning the bronchiolitis epidemic season (October 2012–March 2013), including all children who were hospitalised with a diagnosis of moderate-to-severe bronchiolitis. The following criteria were used to establish a diagnosis of SIADH: urine sodium level of 40mmol/L or greater, urine osmolarity above 500mosm/kg, and urine density of 1020g/L or greater. Demographic characteristics, ventilation mode and clinical outcome were also analysed. A comparison was made between patients that met urine SIADH criteria and those that did not.
ResultsA total of 126 children were included, 23 (18.6%) with urine SIADH criteria. Patients in this group had a higher incidence of pneumonia and/or atelectasis on chest X-ray (21.7% vs. 1.9%, p=.002), worse response to bronchodilator treatment with nebulised adrenaline (69.5% vs. 28,1%, p=.016), more need for respiratory assistance (high flow oxygen therapy (17.4% vs. 7.7%, p=.016)), or non-invasive mechanical ventilation (13% vs. 5.8%, p=.034), and more admissions to the PICU (26.1% vs. 6.8%, p=.007).
ConclusionsPatients older than 1 month with acute moderate bronchiolitis and urine SIADH criteria present poorer progress and greater need for non-invasive mechanical ventilation, PICU admission, and a higher incidence of pneumonia on chest X-ray. For this reason, urine samples should be collected from these patients for early diagnosis of SIADH, and thus early treatment of fluid and electrolyte abnormalities.
Identificar precozmente y analizar las características de pacientes que precisan ingreso por bronquiolitis moderada o grave que cumplen criterios urinarios de SIADH.
Pacientes y métodosEstudio prospectivo observacional, realizado entre octubre de 2012-marzo de 2013 en urgencias pediátricas. Se incluyen menores de 12 meses con bronquiolitis moderada o grave que requieren ingreso. Se consideran criterios urinarios de SIADH: sodio urinario≥40mmol/l, osmolaridad urinaria>500mOsm/kg y densidad urinaria>1.020g/l. Se recogen variables epidemiológicas y clínicas y se comparan 2 grupos definidos por cumplir o no criterios urinarios de SIADH.
ResultadosSe incluyen 126 pacientes con bronquiolitis moderada, 23 (18,6%) cumplen criterios urinarios de SIADH, ninguno grave ni menor de un mes. Los pacientes con criterios urinarios de SIADH tienen mayor incidencia de neumonía y/o atelectasia en la radiografía de tórax (21,7% vs. 1,9%; p=0,002), peor respuesta al tratamiento con adrenalina (69,5% vs. 28,1%; p=0,016), mayor asistencia respiratoria: oxigenoterapia de alto flujo (17,4% vs. 7,7%; p=0,016) y ventilación mecánica no invasiva (13% vs. 5,8%; p=0,034). Requieren más días oxigenoterapia (p=0,02) y tratamiento broncodilatador (p=0,04) y mayor ingreso en cuidados intensivos pediátricos (26,1% vs. 6,8%; p=0,007).
ConclusionesLos pacientes mayores de 1 mes con bronquiolitis moderada y con criterios urinarios de SIADH tienen peor evolución respiratoria, mayor necesidad de soporte respiratorio, ingreso en UCIP y más alteraciones radiográficas. Por ello recomendamos realizar determinaciones de orina a estos pacientes para detectar precozmente el desarrollo de SIADH y cuidar el manejo hidroelectrolítico, previniendo el desarrollo de complicaciones potencialmente graves.
Bronchiolitis is a disease of viral aetiology that is characterised by small and medium-calibre airway obstructions. Diagnosis is based on clinical criteria.1 It is defined as the first episode of respiratory distress, with wheezing in infants under the age of 12 months within the context of upper airway infection during epidemic seasons.2
Incidence of this disease is seasonal, and varies according to country. It affects up to 35.7% of the population during the epidemic season in Spain, with a frequency of hospital admissions of between 1% and 3.5%. Hospitalisation rates are even higher in patients with risk factors.3–5
Fluid and electrolyte imbalance is an added difficulty when treating children with bronchiolitis. This imbalance is not always detected in the early stages, and diagnosis is sometimes delayed until severe complications typical of hyponatraemia develop, such as seizures or apnoea.5–8
The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is characterised by the sustained release of antidiuretic hormone in the absence of usual stimuli (hyperosmolarity, hypotension and hypovolaemia).6
Studies analysing plasma ADH in children have found elevated levels in bronchiolitis, pneumonia, pneumothorax and asthma crises.7–9
The theory that is proposed within the context of bronchiolitis is that, due to pulmonary hyperinflation and hypoxia, the intrathoracic osmoreceptors that activate ADH secretion centrally receive false volume depletion signals. ADH acts in the renal collecting tubule, where the incorporation of aquaporins in the tubule's wall stimulates water absorption, forming very concentrated, high density urine with high concentrations of sodium. The ultimate result of these physiopathological changes is a reduction in plasma osmolality and dilutional hyponatraemia.7–9 Hyponatraemia is not diagnostic, since there are studies in which there are no differences in sodium plasma concentrations between the groups with high levels of ADH and normal levels of ADH.8
Therefore, the analysis of urine samples obtained by non-invasive methods can be useful in selecting patients with SIADH.
Most of the patients admitted due to bronchiolitis do not need venous cannulation, except for those in a severe condition or who reject feeding. Among these, blood tests do not always show osmolality and natraemia. Therefore, we propose a non-invasive method of detecting SIADH.
The objective of this study is to optimise management of SIADH during hospital admission by early identification, without implementing invasive techniques, of patients who meet urinary criteria for SIADH, and to compare their characteristics with those of all infants admitted to the emergency unit due to moderate or severe bronchiolitis, since they could potentially develop SIADH.
Material and methodsThis is a unicentric, prospective, observational and analytical study, performed during an epidemic bronchiolitis season, from October 2012 to March 2013, in the paediatric emergency unit of a tertiary hospital in Madrid.
Patients included in the study were infants under the age of 12 months diagnosed by the attending emergency specialist with moderate or severe bronchiolitis (defined as the first rhinorrhoea, cough, effort of breathing with intercostal recession and/or hypoxia) that required hospitalisation for therapeutic support.2,10
Those patients who, due to their underlying disease or chronic treatment, could have confusing results in their urinary analysis were excluded, as well as those with adrenal insufficiency, nephropathy, heart failure, hypothyroidism, encephalopathy and those undergoing diuretic treatments.
Patients who had symptoms of dehydration were also excluded from the study; they were considered as such if they had scores over 111 in the Gorelick scale.
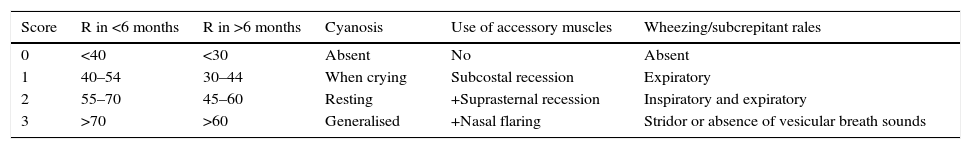
The severity assessment for bronchiolitis was performed by the attending specialist, using the Bierman–Pierson scale.12
In this study, moderate bronchiolitis is defined as a score of between 6 and 10 on the Bierman–Pierson scale after clearing the upper airway of secretions by administering saline solution. It is considered severe when the score is above 10 (Table 1).
Bierman–Pierson scale.
| Score | R in <6 months | R in >6 months | Cyanosis | Use of accessory muscles | Wheezing/subcrepitant rales |
|---|---|---|---|---|---|
| 0 | <40 | <30 | Absent | No | Absent |
| 1 | 40–54 | 30–44 | When crying | Subcostal recession | Expiratory |
| 2 | 55–70 | 45–60 | Resting | +Suprasternal recession | Inspiratory and expiratory |
| 3 | >70 | >60 | Generalised | +Nasal flaring | Stridor or absence of vesicular breath sounds |
RR: respiratory rate (measured in breaths per minute).
Mild bronchiolitis: 1–5 points, moderate bronchiolitis: 6–10 points, severe bronchiolitis: more than 10 points.
Prior to admission, we performed a quick test in all patients to detect the presence of the respiratory syncytial virus (RSV) by means of an immunochromatography of nasopharyngeal secretions (Monolabtest®) obtained by nasal cleansing and aspiration, according to the usual admission protocol for patients with bronchiolitis during epidemic seasons.
During their stay in the emergency unit and subsequent admission to the ward, patients were treated according to the protocol and clinical pathway developed by the hospital for bronchiolitis cases, which includes aerosol therapy with salbutamol or adrenaline, oxygen therapy and/or respiratory support, if needed.
The parents of patients with a Bierman–Pierson score of 6 or over at admission were invited to participate in the study and were asked to sign an informed consent form. Immediately following this, a urine collection bag was placed to collect a sample using a non-invasive method.
The urine of all patients meeting inclusion criteria was tested for sodium (mmol/l), osmolality (mmol/l) and density. We consider as urinary criteria for SIADH the presence of the alterations described in the literature: urinary sodium (NaU) over or equal to 40mmol/l, urinary osmolality (Osm u) over 500mOsm/kg and urinary density over 1.020g/l.13,14
Epidemiologic and demographic data were analysed, such as gender, personal risk history for severe bronchiolitis (chronic pulmonary disease, congenital cardiopathy and prematurity), age (children under the age of 1 and 3 months),3–5 causative agent for bronchiolitis, type of feeding (artificial or breastfeeding) in infants under the age of 6 months, time of onset of the respiratory distress in hours prior to arrival at the emergency unit, transcutaneous oxygen saturation, acuteness according to the Bierman–Pierson scale at the time of arrival and admission into the emergency room, findings in the chest X-ray (only when performed, at the discretion of the clinician), response and days of treatment with a bronchodilator (improvement with bronchodilator treatment is defined as a 2-point reduction in the Bierman–Pierson score, within 30min after administration) and the need for oxygen therapy (maximum support needed) and its duration.
Two groups of patients were compared: one group that met the foregoing urinary criteria and another group that did not have these changes.
For the analysis of the quantitative variables, we used the Mann–Whitney test, whereas for qualitative variables we used Pearson's chi-square test, statistical significance was set at p<0.05 in both cases.
The study was approved by the hospital's Ethics and Clinical Research Committee (ECRC).
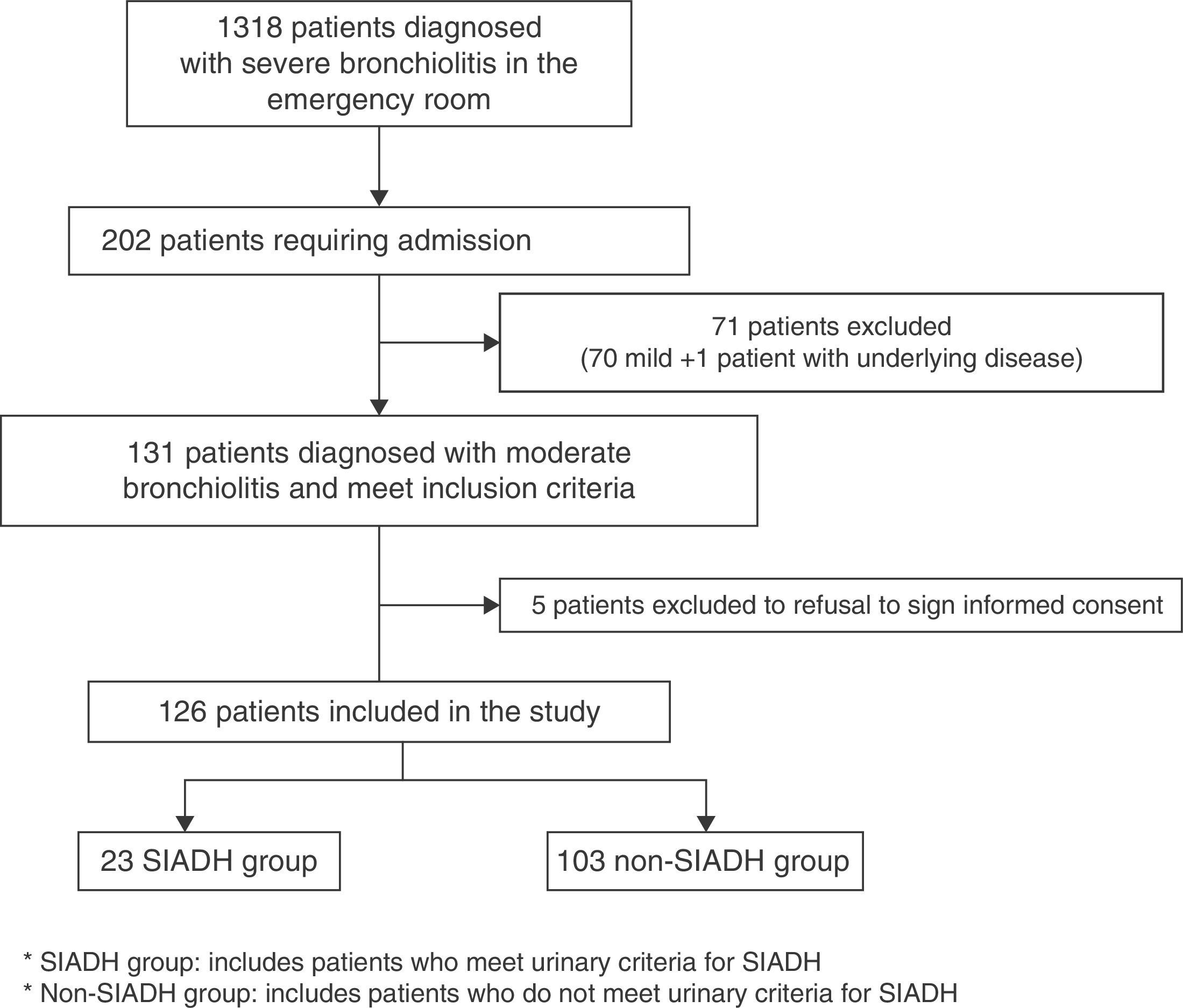
ResultsDuring the bronchiolitis epidemic season, 1318 children diagnosed with bronchiolitis were seen in the paediatric emergency unit, of whom 202 were hospitalised. Of those, 131 were moderate cases, according to the Bierman–Pierson scale. Informed consent was not obtained in 5 cases. The study included 126 patients, of whom 23 (18.6%) met urinary criteria for SIADH. The study did not include any patients with severe bronchiolitis since none had symptoms of severe bronchiolitis at the moment of admission (Fig. 1).
The average age of the patients that met urinary criteria for SIADH was 240 days (p25–p75: 180–330); this was higher (p<0.001) than the age of those who did not meet these criteria (average 70, p25–p75: 45–150). Of the 12 patients aged under 1 month included in the study, none met the urinary criteria for SIADH.
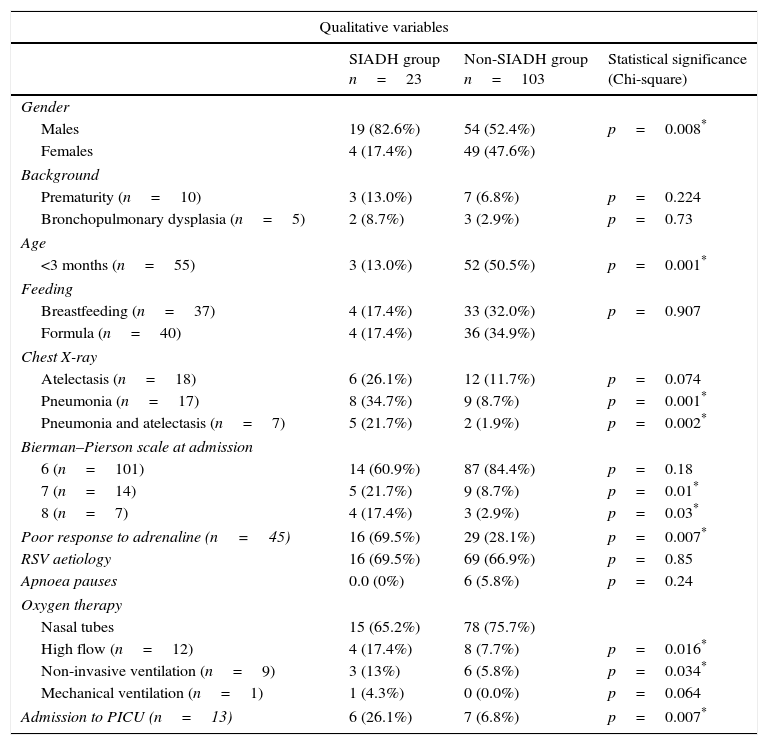
The results of the qualitative and quantitative variables are shown in Table 2. The feeding of 77 infants under the age of 6 months was analysed, but no differences between breastfeeding and artificial feeding were found.
Comparison of clinical and epidemiologic characteristics of patients with moderate bronchiolitis according to the existence of urinary criteria for SIADH.
| Qualitative variables | |||
|---|---|---|---|
| SIADH group n=23 | Non-SIADH group n=103 | Statistical significance (Chi-square) | |
| Gender | |||
| Males | 19 (82.6%) | 54 (52.4%) | p=0.008* |
| Females | 4 (17.4%) | 49 (47.6%) | |
| Background | |||
| Prematurity (n=10) | 3 (13.0%) | 7 (6.8%) | p=0.224 |
| Bronchopulmonary dysplasia (n=5) | 2 (8.7%) | 3 (2.9%) | p=0.73 |
| Age | |||
| <3 months (n=55) | 3 (13.0%) | 52 (50.5%) | p=0.001* |
| Feeding | |||
| Breastfeeding (n=37) | 4 (17.4%) | 33 (32.0%) | p=0.907 |
| Formula (n=40) | 4 (17.4%) | 36 (34.9%) | |
| Chest X-ray | |||
| Atelectasis (n=18) | 6 (26.1%) | 12 (11.7%) | p=0.074 |
| Pneumonia (n=17) | 8 (34.7%) | 9 (8.7%) | p=0.001* |
| Pneumonia and atelectasis (n=7) | 5 (21.7%) | 2 (1.9%) | p=0.002* |
| Bierman–Pierson scale at admission | |||
| 6 (n=101) | 14 (60.9%) | 87 (84.4%) | p=0.18 |
| 7 (n=14) | 5 (21.7%) | 9 (8.7%) | p=0.01* |
| 8 (n=7) | 4 (17.4%) | 3 (2.9%) | p=0.03* |
| Poor response to adrenaline (n=45) | 16 (69.5%) | 29 (28.1%) | p=0.007* |
| RSV aetiology | 16 (69.5%) | 69 (66.9%) | p=0.85 |
| Apnoea pauses | 0.0 (0%) | 6 (5.8%) | p=0.24 |
| Oxygen therapy | |||
| Nasal tubes | 15 (65.2%) | 78 (75.7%) | |
| High flow (n=12) | 4 (17.4%) | 8 (7.7%) | p=0.016* |
| Non-invasive ventilation (n=9) | 3 (13%) | 6 (5.8%) | p=0.034* |
| Mechanical ventilation (n=1) | 1 (4.3%) | 0 (0.0%) | p=0.064 |
| Admission to PICU (n=13) | 6 (26.1%) | 7 (6.8%) | p=0.007* |
| Quantitative variables | |||
|---|---|---|---|
| SIADH group n=23 Mean (IQR) | Non-SIADH group n=103 Mean (IQR) | Statistical significance (Mann–Whitney) | |
| Hours of evolution of respiratory distress | 48 (24–84) | 24 (24–72) | p=0.20 |
| Days of oxygen therapy | 6 (4–9) | 4 (3–7) | p=0.02* |
| Days of bronchodilator treatment | 6.5 (5–11) | 6 (4–8) | p=0.04* |
| Admission days | 6 (5–11) | 4 (4–8) | p=0.06 |
| Oxygen saturation (%) | 96 (92–97) | 93 (90–96) | p=0.93 |
Non-SIADH group: includes patients who do not meet the urinary criteria of inadequate secretion of antidiuretic hormone; SIADH group: includes patients who meet the urinary criteria of inadequate secretion of antidiuretic hormone; IQR: interquartile range.
A chest X-ray was performed in 33 patients, of whom 13 did not have complications, 17 had pneumonia (10 associated with atelectasis) and 3 had atelectasis with no alveolar involvement. Four patients were diagnosed with pneumonia in the emergency room, and 13 were diagnosed during admission.
DiscussionAccording to the literature, SIADH is found in up to 33% of patients with severe bronchiolotis, mainly caused by RSV.5,10,15–18 This, however, is the first study in which urinary criteria is evaluated and used as a screening method.
We found a correlation between greater severity, poorer outcome and more severe complications and patients meeting urinary criteria for SIADH, together with more days of oxygen therapy and bronchodilator treatment, greater need for respiratory support (high flow oxygen therapy and non-invasive mechanical ventilation), worse response to bronchodilator treatment and greater need for admission to the PICU. In our series, only 1 patient needed mechanical ventilation, so we cannot extrapolate conclusions about this treatment. This is consistent with previous publications in which a more symptomatic condition, an increase in the partial pressure of CO2, hypoxaemia and pulmonary hyperinflation are associated with higher levels of ADH secretion.5,8,19,20
Our study shows that patients with pneumonia, whether associated with atelectasis or not, have a higher incidence of urinary criteria for SIADH (54%) and a poorer outcome. These data are also consistent with those reported in previous studies, in which SIADH is found with or without hyponatraemia in up to 45% of pneumonia cases.8,21
Among the qualitative variables analysed, there is an age difference between the group that met ADH urinary criteria and the group that did not. We found a higher percentage of males in the group that met urinary criteria for SIADH, although in our sample there is also a higher number of males than females, globally. The fact that we did not find any patients with urinary criteria under the age of 1 month, regardless of other factors analysed, could be due to the immaturity of the renal tubule in the newborn, which prevents adequate concentration of urine.22 Therefore, we could not perform a comparative analysis, and we consider that in this age group urinary measurements in patients with bronchiolitis would be of little use.
The main limitations of our study derive from the fact that it is unicentric, comprises only 1 epidemic period, and no ADH plasma levels were measured. The chest X-ray was performed at different times, so the early or late development of radiographical alterations could have influenced the presence of urinary criteria at the time of admission. Likewise, we did not find any severe bronchiolitis during this period, so it has not been possible to analyse and compare these data with moderate forms and with what is described as severe forms in literature.
According to the results we have obtained and the data described in previous studies, we can conclude that in patients over 1 month of age, with moderate bronchiolitis and a score of over 6 on the Bierman–Pierson scale, particularly those with radiographical findings of pneumonia, as well as those requiring high flow oxygen therapy or admission to the PICU, urine tests should be performed in the emergency room to detect those who meet the urinary criteria for SIADH, and thus monitor the fluid–electrolyte balance in order to prevent the development of potentially acute complications.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Toledo del Castillo B, González Ruiz de León E, Rivas García A, Vázquez López P, Miguez Navarro MC, Marañón Pardillo R. Asociación entre bronquiolitis moderada-grave y síndrome de secreción inadecuada de hormona antidiurética en urgencias. An Pediatr (Barc). 2016;84:24–29.