To compare the results of secondary alveoloplasty performed in one Hospital when osteosynthesis material was used and when the bone graft does not require this material, and relating them to factors such as gender and age.
Material and methodsA retrospective study was conducted from the years 2014 to 2019 in this Hospital on selected patients who met the inclusion criteria. Two periods of ages, period A: ages between 5−12 years (mixed secondary alveoloplasty) and period B: older than 12 years (late secondary alveoloplasty). Autologous bone from the iliac crest or parietal calotte was used for the bone graft. The patients were divided into 2 groups: group I: patients with alveoloplasties that required osteosynthesis material. Group II: patients who did not require osteosynthesis material. Parameters evaluated: the success criteria for alveoloplasty were assessed according to the clinical parameters described by Precious. Alveoloplasty was successful if they met all the criteria of Precious in the year of intervention. Postoperative complications in both groups were evaluated. The statistical analysis was performed using the Exact Fisher exact test for qualitative variables.
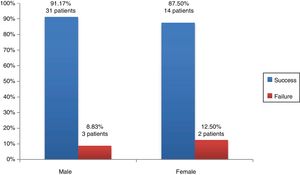
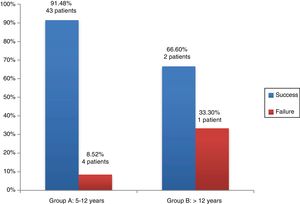
ResultsAlveoloplasty was successful in 89.4% of patients in group I, while it was 90.3% in group II. Alveoloplasty was successful in 87.5% of females compared to 91.17% of males. The intervention was a success in 91.48% of patients in group A, compared to 66.6% in group B. The osteosynthesis material in two patients of Group I was not degraded in the annual assessment. There were no significant differences in any of the comparisons.
ConclusionsThe use of osteosynthesis material does not alter the integration of the bone graft in patients that undergo alveoloplasty. Factors such as gender or age do not influence the results of the interventions.
Comparar los resultados de alveoloplastias secundarias realizadas en nuestro Hospital cuando utilizamos material de osteosíntesis y cuando el injerto óseo no precisa de dicho material relacionándolos con factores como el sexo y la edad.
Material y métodosRealizamos estudio retrospectivo de los años 2014–2019 en nuestro Hospital y seleccionamos los pacientes que cumplían los criterios de inclusión en nuestro estudio. Establecemos 2 grupos de edades, grupo A: edades entre 5-12 años (alveoloplastia secundaria mixta) y el grupo B: más de 12 años (alveoloplastia secundaria tardía). Para el injerto óseo se utilizó hueso autólogo procedente de cresta iliaca o calota parietal. Dividimos los pacientes en 2 grupos: grupo I: pacientes con alveoloplastias que precisaron de material de osteosíntesis. Grupo II: pacientes que no precisaron de material de osteosíntesis. Parámetros evaluados: los criterios de éxito de la alveoloplastia se valoraron según los parámetros clínicos descritos por Precious. La alveoloplastia era exitosa si cumplían todos los criterios de Precious al año de intervención. Evaluamos las complicaciones postoperatorias en ambos grupos. El análisis estadístico se realizó con el test exacto de Fisher para variables cualitativas.
ResultadosEl éxito de la alveoloplastia se produjo en el 89,4% de los pacientes del grupo I mientras que en el grupo II fue del 90,3%. La alveoloplastia fue exitosa en el 87,5% del sexo femenino frente al 91,17% de varones. En el 91,48% de los pacientes del grupo A la intervención fue un éxito frente al 66,6% del Grupo B. En 2 pacientes del grupo I el material de osteosíntesis no se degradó en la valoración anual. No existieron diferencias significativas en ninguna de las comparaciones.
ConclusionesLa utilización de material de osteosíntesis no altera la integración del injerto óseo en pacientes a los que se realiza alveoloplastia. Factores como el sexo o la edad no influyen tampoco en los resultados de las intervenciones.
Cleft lip and cleft palate is the most frequent congenital craniofacial malformation, with an incidence of 1 per 800 live births.1 Most of these patients present clefting of the alveolar bone. Repair of the bony defect must be included in the treatment plan of these patients to minimise the stigma associated with the cleft to a minimum.2
Multiple factors, genetic as well as environmental, are involved in the aetiology of cleft lip and palate. Its aetiology is generally multifactorial, although in some cases it is associated with specific syndromes or is part of a polymalformative syndrome.3
Alveoloplasty with alveolar bone grafting has become a standard treatment in the bone repair of patients with cleft lip and palate after surgical closure of the cleft, and current orthodontic and prosthetic management protocols are based on the presence of adequate bony structures before the eruption of the permanent canines in the alveolar cleft region.
The goals of alveoloplasty are the following4,5:
- •
Creating a stable and continuous maxillary dental arch that makes tooth eruption through the bone graft possible.
- •
Providing bony support to adjacent teeth, allowing their preservation and facilitating orthodontic intervention at the cleft site.
- •
Improving oral and nasal hygiene by closing the fistula and eliminating mucosal recesses.
- •
Reducing the need of prosthetics.
- •
Providing bony support to the apertura piriformis, thus improving facial symmetry through elevation of the nasal ala and improvement of the nasolabial angle.
One of the important factors in this approach is the graft source, and there is consensus that fresh autogenous bone is the best choice for secondary alveolar bone grafting, as it supplies living, immunocompatible bony cells that integrate fully with the maxilla and are essential for osteogenesis.6
The donor site must be selected based on the required volume of bone for the graft, the type of bone, the anatomical conformation, access to the site and potential sequelae or complications at the donor site.7
There are different potential choices of sites, such as the iliac crest, the parietal bone, the mandibular symphysis and the tibia, among others. However, the iliac crest and the cranium and the best choices because they achieve optimal outcomes and integrate better at the transplant site.8,9
In some instances, the characteristics and size of the graft require stabilization with internal fixation systems. There is no question that the development of rigid fixation systems has been one of the most important advances in modern maxillofacial surgery.10
There is ample evidence on the excellent qualities of titanium; however, the development and widespread popularity of the combination of polylactic and polyglycolic acids (resorbable materials) has led to increasing use of these materials in the field of paediatric maxillofacial surgery, in most instances displacing titanium.11
These resorbable materials dissolve into small fragments that are phagocyted by macrophages and foreign-body giant cells. The products that result from their degradation are metabolised into carbon dioxide and water and are eliminated through respiration. Complete degradation of these materials takes between 6 months and 4 years depending on their composition, although they lose their tensile strength months before.12
Objectives- 1
General objective: to compare the outcomes of secondary alveoloplasties performed in our hospital when internal fixation implants were used versus not required to support the bone graft.
- 2
Specific objectives: to analyse the association of factors such as age and sex with outcomes.
We conducted a retrospective study of patients managed at the Complejo Hospitalario Virgen de las Nieves in Granada, Spain, in the 2014–2019 period that met the inclusion criteria.
Inclusion criteria:
- •
Either sex.
- •
Presence of a residual alveolar cleft after closure of the lip and palate cleft.
- •
Presence of an unerupted permanent canine or incisor tooth in the alveolar cleft.
- •
No previous history of alveoloplasty.
- •
Surgeries performed by the same surgical team.
- •
Absence of additional malformations.
- •
Signed informed consent by one of the parents or legal guardians of the patient.
Exclusion criteria:
- •
Refusal of parents to consent to participation.
- •
Failure to meet any of the inclusion criteria.
We classified patients by age into 2 groups: group A, ages 5–12 years, the period of mixed dentition before eruption of the canine tooth (early secondary alveoloplasty), and group B, ages 12 years and greater, after the eruption of all permanent teeth (late secondary alveoloplasty).
The graft source was autologous bone from either the iliac crest or the parietal bone, selected indistinctively without applying any criteria related to the patient or the surgical technique.
The three-dimensional reconstruction of the alveolar defect with bone from the iliac crest or parietal bone was performed following the split block bone or tunnelling approach described by Khoury for bone reconstruction at the atrophic alveolar crest.
We divided patients into 2 groups based on the use of internal fixation implant materials:
- 1
Group I: patients that underwent alveoloplasty requiring resorbable or titanium implants.
- 2
Group II: patients that underwent alveoloplasty not requiring resorbable or titanium implants.
The decision whether to employ fixation systems was based solely on the purpose of achieving adequate stabilization of the bone graft, the need for which was assessed during the procedure itself by the surgical team based on clinical practice standards.
Analysed variables: the criteria used to assess the success of alveoloplasty were the clinical parameters proposed by Precious13:
- •
Closure of oronasal fistula
- •
Eruption of teeth through the graft
- •
Bony support of adjacent teeth
- •
Stability and continuity of maxillary dental arch.
- •
Alar base support
- •
Improved function of the cleft nose.
We considered that alveoloplasty had been successful if all the above criteria were met within 1 year from the operation. We used panoramic radiographs to assess alveoloplasty failure (graft loss, absence of tooth eruption through the graft, recurrence of oronasal fistula, detachment of fixation systems, etc).
We analysed postoperative complications such as infection, inflammation, removal of fixation systems, delayed degradation of fixation materials, nerve damage and foreign body reaction.
We collected data on the independent variables under study and entered them in a database built for the purpose. We used the Fisher exact test to compare qualitative variables using the software SPSS version 21 and considered p-values of less than 0.05 statistically significant.
ResultsThe initial sample included 53 patients, out of which 3 were excluded due to incomplete data collection in the review of health records.
Of the 50 patients included in the definitive sample, 34 were male and 16 female (Table 1).
The group aged 5−12 years included 47 patients, and the group aged more than 12 years included 3. The mean age of the sample was 9.1 ± 0.4 years.
When it came to the graft source, the bone was obtained from the iliac crest in 28 patients and from the parietal skull in 22 patients.
In 24% of cases (12 patients) the alveolar cleft was bilateral.
Fixation systems were used in 19 patients: titanium plates in 3 cases and resorbable fixation systems in 16 (LactoSorb). The titanium plates were used in 1 patient aged 14 years and 2 patients aged 12 years. Fixation systems were not implanted in the remaining 62% of patients.
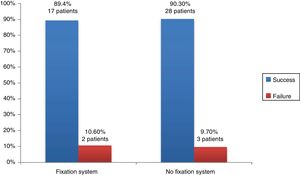
The alveoloplasty was successful in 17 patients in Group I whose procedure included implantation of fixation systems, while the alveolar graft failed in another 2: in one case due to reopening of the oronasal fistula and in another due to necrosis in the premaxilla.
In Group II (no use of fixation systems), the alveolar bone graft was successful in 28 patients and failed in 3 cases: in 2 cases due to reopening of the oronasal fistula, and in 1 case due to graft loss (Fig. 1).
The Fisher exact test did not reveal statistically significant differences in the outcome of alveoloplasty based on whether fixation systems were or not used (P = 1).
When it came to the association of sex with graft outcomes, as can be seen in Fig. 2, we found that alveoloplasty was successful in 31 male patients (91.17%) compared to 14 female patients (87.5%). We did not find statistically significant differences in surgical outcomes based on sex (P = .65).
As for the association of graft outcomes and the age groups established in our study, we found that the graft was successful in 43 patients (91.48%) in group A and in 2 patients (66.6%) in Group B (Fig. 3). We did not find statistically significant differences using the Fisher exact test (P = .26).
Concerning postsurgical complications, there were only 2 patients (in the group of patients with resorbable fixation systems) in whom fixation materials remained undegraded at the 1-year follow-up evaluation, which did not have any impact on the outcome of the graft.
DiscussionFollowing the publication of works by Bergland et al.,14 multiple other studies have provided evidence that secondary alveoloplasty is the method of choice for surgical correction of the residual alveolar cleft in patients with cleft lip and cleft palate. The goals of repair must be met without affecting mid-facial growth, due to which performance of alveoloplasty during the mixed dentition stage (before the eruption of the permanent canine tooth or the lateral incisor tooth, if present) is preferred, between ages 5 and 12 years.15 Secondary alveolar bone grafting offers substantial benefits to patients with alveolar cleft, since completion of the dental arch allows descent of the canine tooth, provides stability to the maxilla and supports the ala of the nose with a low risk of complications.16,17
The graft type and source has been subject to extensive study and debate in the literature in both human and animal models with very heterogeneous results. Recent studies on animals have demonstrated that the dynamics of cancellous bone grafts (iliac crest) differ from those of cortical bone grafts (parietal skull), with the latter showing earlier vascularization and a greater volume of maintained bone, as they form larger bone arches and exhibiting less resorbption.18 Rychlik and Wojcicki19 suggested that fresh autogenous cancellous bone is the best choice for bone grafts, as it supplies immunocompetent cells that integrate fully in the maxillary bone and essential to osteogenesis. Mayer and Molsted3 suggest that the iliac crest is the ideal donor site for alveolar bone grafting. In our study, either graft source was selected nonpreferentially and independently of patient characteristics and the surgical approach, and the distribution between both types was fairly even. Although this was not an objective in our study, we did observe that success rates were similar for either donor site and whether fixation systems were implanted or not. The work of Alonso et al.20 pave the way for advances in the application of tissue engineering with the combined use of an iliac crest graft and recombinant human bone morphogenetic protein (BMP) for bone reconstruction; although outcomes were not superior when this protein was added, it opens new possibilities in the field of maxillofacial surgery.
Tissue engineering is contributing to improving how bony defects are repaired in patients with cleft lip and cleft palate. Autogenous bone is currently the material of choice for procedures involving bone grafting in the cleft palate, as it provides a support on which bone cells can proliferate, inducing proliferation of undifferentiated cells and their differentiation into osteoblasts.
In our study, the decision to use fixation systems was based solely on the objective of achieving adequate stabilization of the bone graft. Different authors21 have published evidence on the usefulness of systems made of titanium or resorbable materials to achieve fixations that would allow successful grafting. The decision to use fixation systems is always based on multiple factors, but the main goal is to achieve adequate integration of the graft in the maxilla thanks to correct stabilization. The use of resorbable materials in cleft palate corrective surgeries is increasing progressively. The existing evidence demonstrates that this is a valid alternative to the use of titanium systems in most clinical situations.22 They are available in different proportions of polyglycolic and polylactic acid (LactoSorb and BioSorb) and preserve 70% of their initial strength for 6–8 weeks, and most degrade fully within one year. Ylikontiola et al.23 used resorbable plates for fixation in the repair of alveolar clefts with favourable outcomes: only one patient experienced intraoral exposure of the plate, which required its removal. Hoffman et al.24 used BioSorb plates in 22 patients and did not observe complications in wound healing, which they assessed based on clinical features and imaging tests. Suuronen et al.25 conducted a retrospective study that included more than 200 patients in whom resorbable fixation systems were used in a variety of maxillofacial interventions over a period of 7 years, and the authors concluded that resorbable plates may be used routinely in maxillofacial fixation. Thrivikraman et al.26 discussed novel biomaterials in their study, including resorbable materials, and recent advances in 3D technologies and bioprinting techniques applied to craniofacial reconstruction, remarking on the considerable potential of these biomaterials in the repair of bony defects. In their article, Ferretti and Reyneke27 explained that advances in the design of miniplates and microplates with very low profiles (1–1.5 mm) and very short, self-drilling screws are a significant breakthrough, as they achieve far superior stabilization compared to other products. One of the most controversial aspects in the use of resorbable fixation devices is stability, as cases have been published in the literature of patients that required additional surgeries to stabilise the maxilla. From a clinical perspective, it is evident that fixation is less strong compared to the use of titanium, but the frequency of cases requiring reoperation to stabilise the graft published in the literature is negligible.28 An optimal resorbable system must be able to support bony fragments during the healing period and be fully degraded once healing is complete, and its metabolites should not cause any local or systemic reactions. These characteristics offer unquestionable advantages, chief of which is not requiring removal.
In our study, we assessed the success of alveoloplasty based on the clinical parameters described by Precious, and we found high success rates at 1 year post-intervention, specifically of 89.4% in the group without fixation systems and 90.3% in the group with fixation systems. The success rates of alveoloplasty published in the literature range from 51% to 95%. In a study conducted between 2010 and 2015, Baldin et al.29 considered that the alveolar bone graft had integrated poorly in 51% of patients that had undergone surgical repair of a cleft palate. Goudy et al.7 determined that the success rate of alveoloplasty in their study was as high as 90%. The outcomes in our study were within similar ranges to those of the reviewed works in the previous literature.
Although in our study we only used panoramic radiographs, other radiological techniques can be used to assess the outcomes of alveolar bone grafting in case failure is suspected. The most commonly used scale is the one proposed by Whitherow et al.30; such scales are based on the use of plain radiographs, are accurate, and allow assessment of graft integration, although they have some limitations, such as distortion and superimposition of structures. Cone beam computed tomography is an effective method, both in the postoperative period, for assessment of the graft, and in the preoperative period, for calculation of the volume of bone needed to close the alveolar cleft.31
It is widely accepted that the ideal timing for secondary alveoloplasty is between 5 and 12 years of age, corresponding to the period of mixed dentition before eruption of the permanent canine tooth, when one-third or half of the root has formed, as the success rate is greater at this stage due to more predictable bone availability.32 In our study, we established 2 age groups, group A including ages 5–12 years (mixed dentition period) and group B including ages greater than 12 years. Alveoloplasty was successful in 91.48% of patients in group A and success dropped to 66.6% in group B, although the difference was not statistically significant. Other authors have established 2 age groups, for instance Tabrizi et al.,33 who established one group for ages 9–13 years and another for ages greater than 13 years; the success rate in the younger group was 92% compared to 20% in the older group, and the authors concluded that success is more frequent in the mixed dentition period and that bone availability is more predictable at this stage, which benefits both the donor site and the recipient site.
In our study, sex was not associated with differences in the success rate of secondary alveoloplasty, which was consistent with the findings of other studies.
We found few postoperative complications associated with the use of fixation systems in our study, as we only found undegraded fixation material in 2 patients at the 1-year followup, which did not have any impact on the success of alveolar bone repair. Previous studies also have not reported significant complications derived from the use of resorbable or titanium fixation systems.34
ConclusionsIn our study, the outcomes of secondary alveoloplasties for correction of cleft lip and palate did not change based on the use of fixation system to stabilize the maxillary prominences, so they can be used as needed without fear that they will interfere with the integration of the graft. Factors like sex or age were not correlated to surgical outcomes.
Advances in tissue engineering are paving the way for a very promising future in the field of maxillofacial surgery, combined with traditional approaches, as reflected by the growing number of publications in recent years, and may make it possible to avoid collection of bone grafts or greatly reduce their volume, which would decrease morbidity at the donor site.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Parrilla EMC, Sanfiel JR, Camarasa BG, Valadés RF. Alveoloplastias y utilización de material deosteosíntesis en la fisura labiopalatina. An Pediatr (Barc). 2020;93:170–176.