A male adolescent aged 17 years with no relevant medical history visited the emergency department and the primary care center five times in the same year due to pain in his right calf. He received a diagnosis of muscle pain and a prescription for nonsteroidal anti-inflammatory drugs (NSAIDs) without undergoing any imaging tests.
A year after the onset of symptoms, he returned to his assigned primary care center due to persistent pain, which was now constant and occasionally nocturnal, which responded well to NSAIDs. He reported playing soccer but denied any trauma associated with the activity.
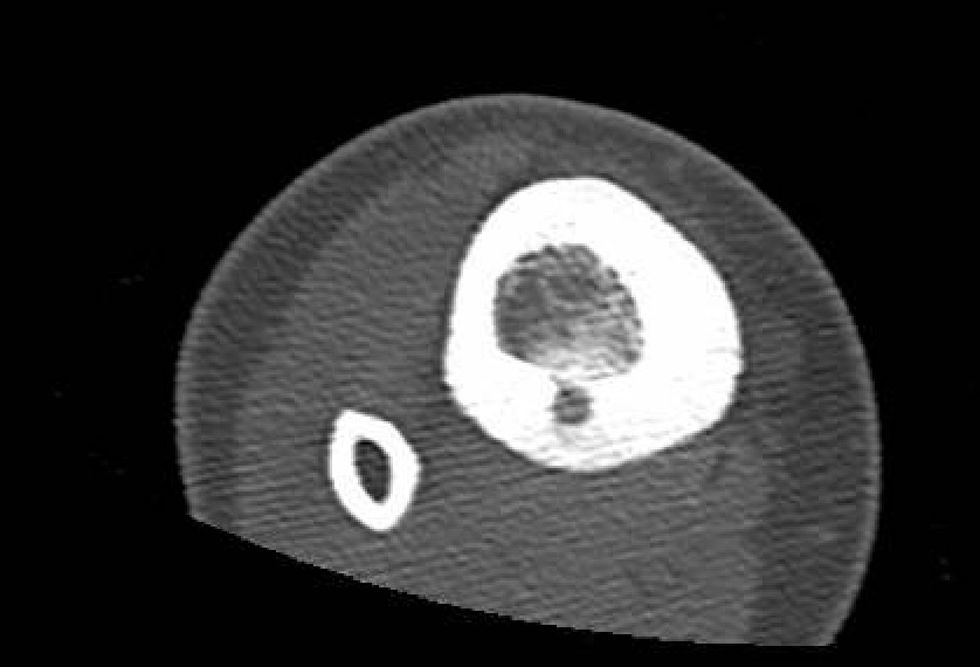
An X-ray was ordered (Fig. 1), which revealed a punctiform cortical lesion in the right tibia with a perilesional osteosclerotic reaction. Computed tomography and magnetic resonance imaging (Figs. 2 and 3) revealed an oval lytic lesion measuring 5 × 8 mm in the posteroinferior cortex of the tibia with reactive sclerosis, consistent with osteoid osteoma. In light of this suspected diagnosis, he was referred to traumatology and is awaiting treatment with radiofrequency ablation.1
The differential diagnosis included subacute osteomyelitis (Brodie abscess), which was ruled out due to the absence of fever, a history of infection and abnormal laboratory results. However, its clinical presentation can overlap that of osteoid osteoma, and in some cases histological analysis of the bone is the only way to definitively differentiate them. Stress fracture is another condition that needs to be ruled out.
The mean diagnostic delay for this disease is usually 2 years, despite its characteristic clinical presentation, such as persistent night pain that responds to NSAIDs or acetylsalicylic acid. In this case, although the diagnosis was made within 15 months (an average delay for this type of lesion), we ought to highlight the significant impact on the patient’s quality of life and the many visits he made during this time.2,3
The authors have no conflicts of interest to declare.