Distal intestinal obstruction syndrome (DIOS) refers to a phenomenon of bowel obstruction in children with cystic fibrosis (CF) with manifestations that are very similar to those of meconium ileus in infants.1 It is characterised by an accumulation of viscid faecal material combined with thick mucosal secretions that adheres to the crypts of the terminal ileum and the caecum and is difficult to remove.2 It may develop in 8.3–16% of patients with CF, presenting as acute intestinal obstruction or subacutely (pseudo-obstructive episodes), and it recurs in 50–76% of cases.1–3 The patient may present with a mass in the right iliac fossa (detection of faecal matter by radiography) along with obstruction of varying degrees (vomiting of bilious or faecal material, abdominal pain and distension). It is essential to differentiate DIOS from constipation, appendicitis, intussusception, adhesion-related disorders, Crohn's disease and fibrosing colonopathy.1–4 The insufficient secretion of chloride and water, a slow intestinal transit, impaired ileal secretion and fat malabsorption are predisposing factors. There is no evidence of a link between DIOS and excessive pancreatic enzyme supplementation.4 Some of the risk factors for DIOS are: severe genotypes (DF508, W1282X), pancreatic insufficiency, dehydration, history of meconium ileus, lung transplant and a previous episode of DIOS.1–3 The management of DIOS is usually conservative by means of antegrade or retrograde lavage with laxative or surfactant enemas (phosphate, N-acetylcysteine, polyethylene glycol [PEG], or meglumine diatrizoate [MD, Gastrografin®, Schering, Berlin]).1–3 In this article, we present the cases of three patients with CF that suffered several episodes of DIOS.
Case 1Male patient aged 11 years with CF DF508, afebrile, presenting with abdominal pain and distension, constipation and bilious vomiting of 48 hours’ duration. Abdominal radiography showed abundant faecal material in the right iliac fossa, while the ultrasound findings were normal. Treatment with N-acetylcysteine via enema was initiated due to suspected DIOS, leading to partial relief of symptoms and the production of a small volume of soft stools. At 24h, a barium enema with Gastrografin® was performed under radiographic control, and the episode resolved.
Case 2Female patient aged 6 years with CF DF508 presenting with constipation, bilious vomiting and abdominal pain of two days’ duration. Treatment with phosphate enemas was initiated for suspected DIOS, followed by an N-acetylcysteine enema that was repeated at 24h, resulting in the production of soft stools and the resolution of symptoms.
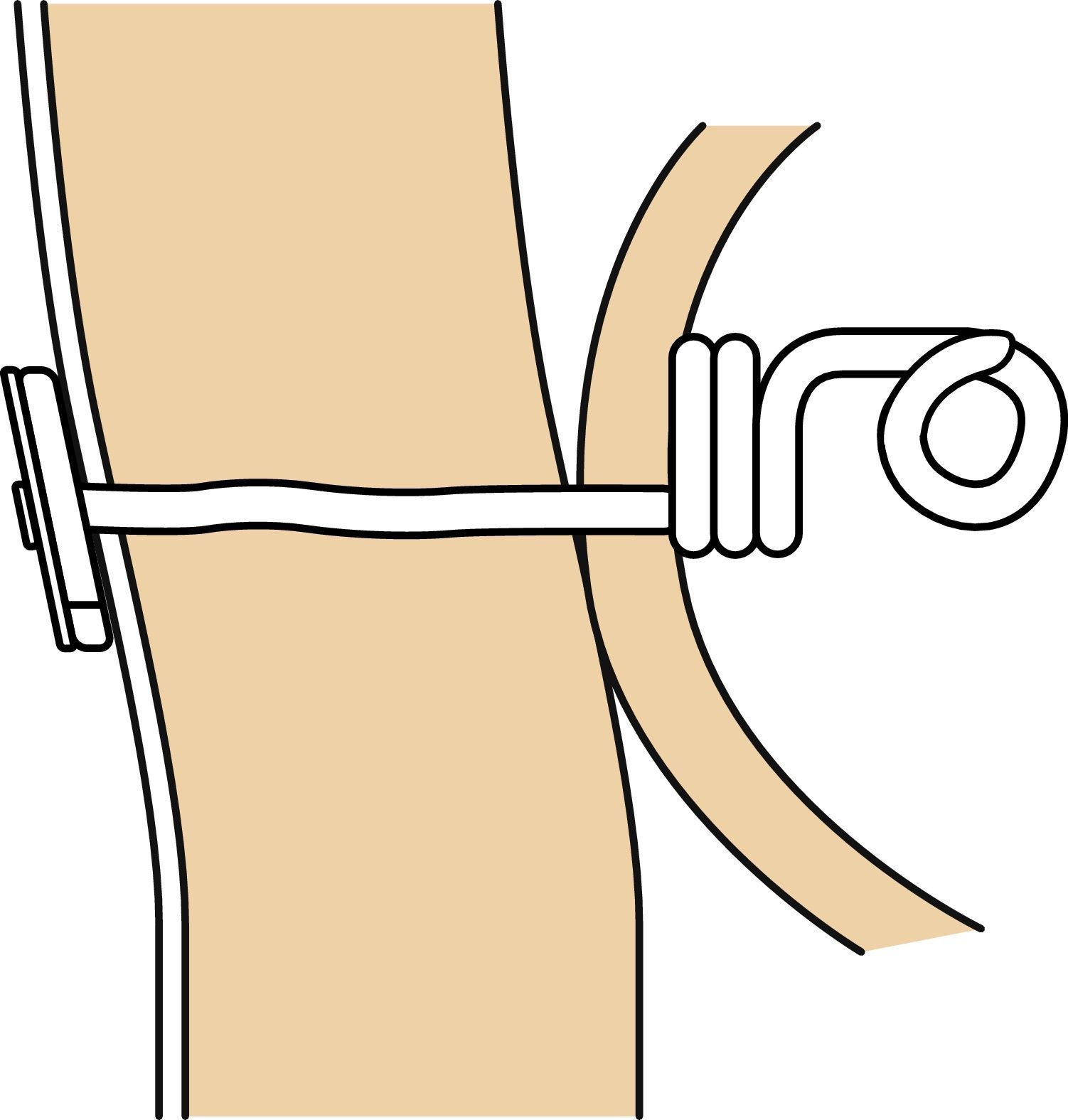
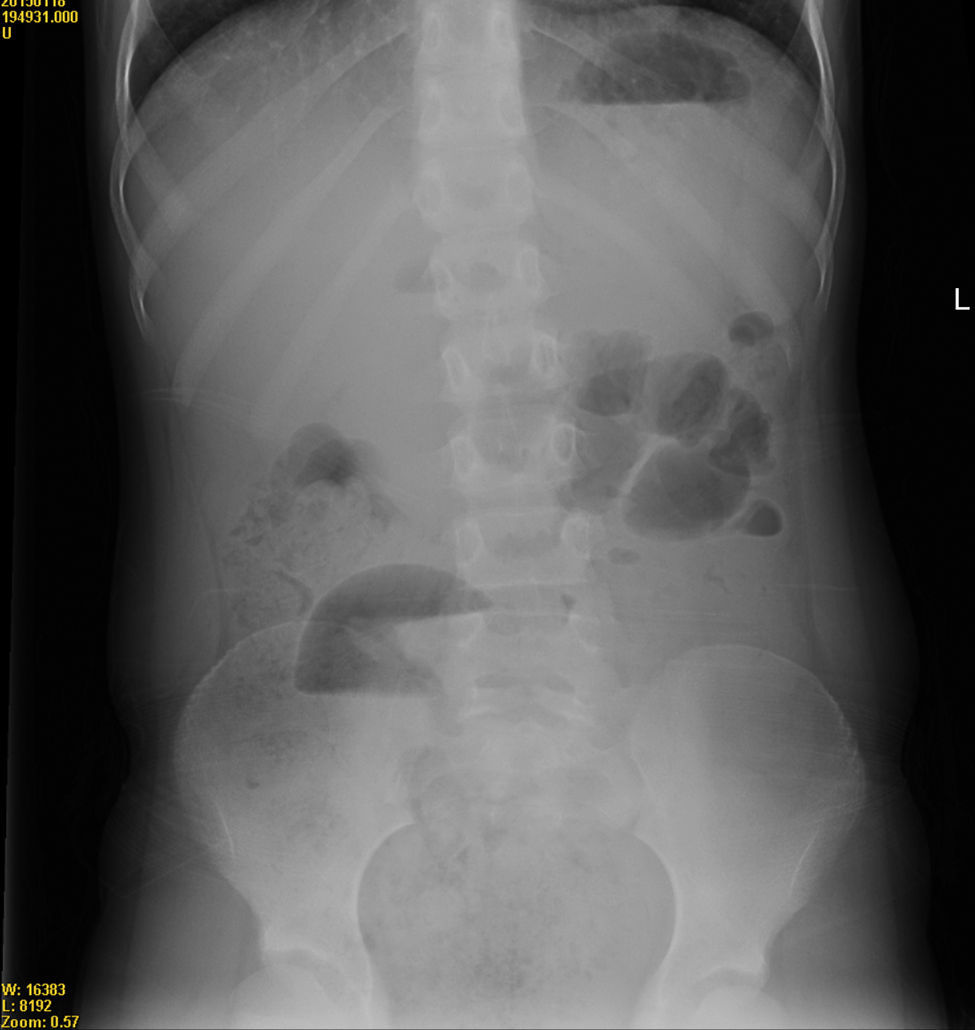
Case 3Female patient aged 5 years with CF DF508, presenting with DIOS of 4 days’ duration with a sudden worsening of symptoms after conservative treatment. A laparotomy was performed, revealing plastic peritonitis and faecal impaction in the distal ileum and colon. Manual disimpaction was performed, followed by caecostomy (Chait procedure) with placement of a Kher tube used in subsequent days to start treatment with antegrade lavage with N-acetylcysteine and PEG. The Kher tube was replaced by a Chait trapdoor (Fig. 1) for continued delivery of enemas, which was removed at seven months. In the four years that followed, the patient had two new episodes of DIOS (Fig. 2) that were treated early with rectal Gastrografin® gravity enemas (in the ward), with resolution of symptoms in both.
The conservative management of DIOS by means of laxatives or surfactants, administered either orally (in cases of low-grade obstruction) or via enema, is effective in 89–96% of cases,1–3 especially if it is initiated early. The administration of PEG at doses of 2g/kg/day (or 20–40mL/kg/h of solution, administered orally or with a nasogastric tube over 6–8h) is recommended, or alternatively a solution of 50mL of Gastrografin® in 200mL of water in children up to 6 years of age and of double this amount for older patients.1 The treatment can be repeated on subsequent days with the administration of half doses. The use of rectal lavage with water and/or Gastrografin® delivered directly to the caecum by colonoscopy has also been reported.5,6 In case of treatment failure or poor response to treatment, the surgical approach should be based on disimpaction with washout of the ileocaecal area, and enterostomy or caecostomy are preferred over intestinal resection.1,5,6 We chose to perform a caecostomy with placement of a temporary button in our patient because a complete disimpaction was not possible and due to the presence of peritonitis. This option allowed the patient to continue undergoing antegrade lavage efficiently during the convalescence period. Another, more permanent alternative reported in adult CF patients with recurrent DIOS refractory to conservative treatment and with poor adherence to treatment (as a last step in management, after failed enemas and having decided against placement of a Chait caecostomy catheter), is the performance of an antegrade continence enema (ACE),6 bringing the appendix out onto the abdominal wall to create a permanent stoma through which the bowel can be washed out periodically.
Please cite this article as: Fernández-Ibieta M, Ayuso-González L, Fernández-Córdoba MS, Argumosa-Salazar Y, Gonzálvez-Piñera J. Opciones de tratamiento del síndrome de obstrucción intestinal distal: ¿y si los enemas fallan? An Pediatr (Barc). 2016;84:54–55.