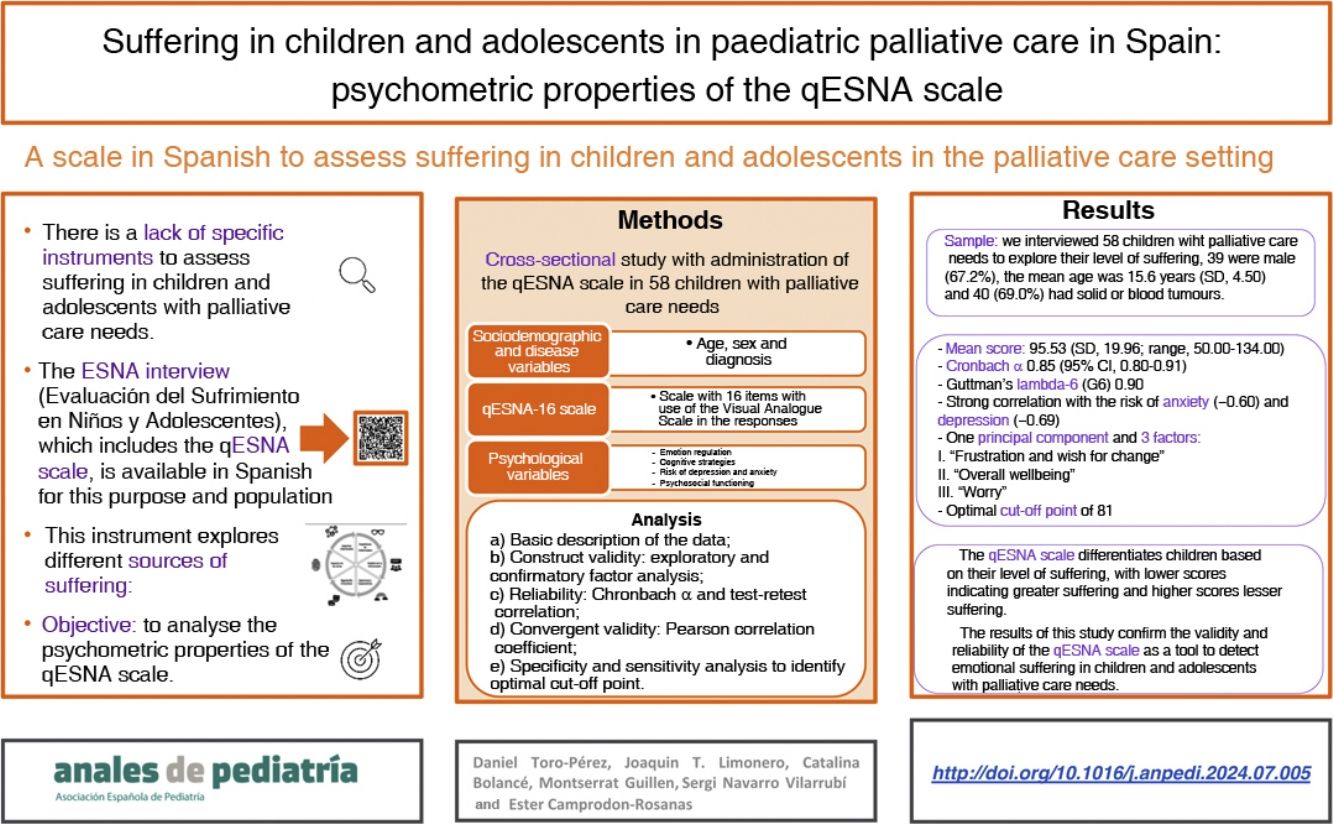
To analyze the psychometric properties of the qESNA scale and its usefulness to assess the suffering of paediatric patients with life-limiting and/or life-threatening diseases (children with LLTC) in clinical practice.
MethodsCross-sectional and longitudinal study in 58 patients in Spain (female, 32.8%; mean age, 15.6 [SD, 4.5]; age range, 8–23 years), with administration of the qESNA scale along with other scales to assess anxiety, depression, emotion regulation and psychosocial functioning. We performed exploratory and confirmatory factor analyses and calculated goodness-of-fit indices were calculated; we assessed reliability by means of the Cronbach alpha and temporal stability and convergent validity through the intraclass correlation coefficient with scales used to assess psychological disorders and the specificity and sensitivity through ROC curves.
ResultsThe factor analysis identified a 14-item scale with 3 factors, a comparative fit index of 0.93, a Tucker-Lewis index of 0.91 and a root mean square error of approximation of 0.07. The Cronbach alpha was 0.85 and the intraclass correlation coefficient was 0.66. The convergent validity was high for the correlation to the risk of depression (−0.69) and of anxiety (−0.60) and emotional changes (−0.59). The analysis of the ROC curves showed that a score of less than 81 would be indicative of suffering, with a sensitivity of 83.33% and a specificity of 93.48%.
ConclusionsThis study confirmed that the psychometric properties of the qESNA scale are good and the scale’s usefulness as an instrument to detect emotional suffering in children with life-limiting or life-threatening illnesses in clinical practice.
Analizar las propiedades psicométricas de la escala qESNA y su utilidad clínica para evaluar el sufrimiento de pacientes infantojuveniles con enfermedades limitantes y/o amenazantes para la vida (niños con LLTC).
Métodos58 pacientes en población española (mujeres = 32.8%; edad media = 15.6 ± 4.5 [8–23 años]), respondieron a la escala qESNA en un diseño transversal y longitudinal junto con otras escalas que evaluaban ansiedad, depresión, alteraciones emocionales y funcionamiento psicosocial. Se realizaron análisis factoriales exploratorios y confirmatorios, y calcularon índices de bondad de ajuste; la fiabilidad se obtuvo a partir del alfa de Cronbach y de estabilidad temporal; la validez convergente mediante coeficientes de correlación intraclase con escalas sobre alteraciones psicológicas; y el análisis de especificidad y sensibilidad a través de las curvas ROC.
ResultadosEl análisis factorial identificó una escala de 14 ítems con 3 factores, con un índice de ajuste comparativo de 0.93, índice de Tucker-Lewis de 0.91 y error cuadrático medio de aproximación de 0.07. El alfa de Cronbach fue de 0.85 y el coeficiente correlación intraclases de 0.66. La validez convergente fue alta en la correlación con el riesgo de depresión (-0.69) y ansiedad de (-0.60) y las alteraciones emocionales (-0.59). Los análisis de curvas ROC indican que una puntuación <81 sería tributaria de sufrimiento presentando una sensibilidad del 83.33% y especificidad de 93.48%.
ConclusionesEste estudio confirma las buenas propiedades psicométricas de la escala qESNA y su utilidad clínica como instrumento para detectar el sufrimiento emocional en niños con enfermedades limitantes o amenazantes para la vida.
At the global level, there are approximately 21 million children and adolescents aged 0–19 years (hereafter, ‘children’) with life-limiting or life-threatening conditions (LLTCs),1 and, in Spain, approximately 25 000 children are considered to have palliative care needs.2 The World Health Organisation defines the goal of paediatric palliative care (PPC) as the alleviation of suffering with a multidimensional physical, psychological, social and spiritual approach.3,4
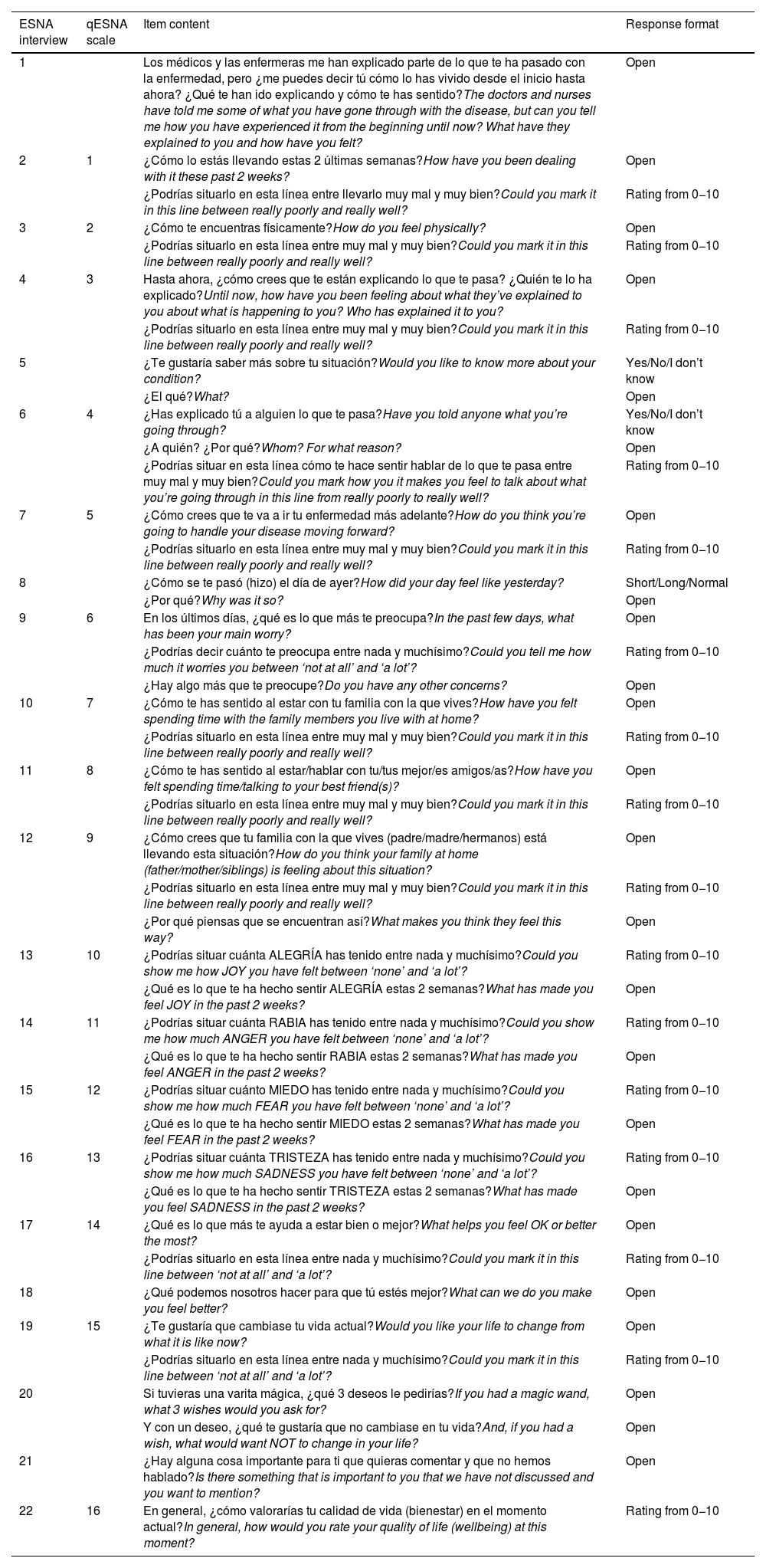
Children with LLTCs are at risk of suffering,5 for instance in the form of pain, irritability, adjustment disorders, in addition to depression and anxiety.6 The key element in understanding the experience of suffering in children with LLTCs is their perceived level of discomfort and threat to themselves,7,8 yet this is a rarely explored perspective.9,10 In the PPC setting in particular, there is a lack of instruments11 to assess this perception of suffering. In the Spanish language, there is the interview for the Evaluation of Suffering in Children and Adolescents with Palliative Needs (ESNA, for Evaluación del Sufrimiento de Niños y Adolescentes),12 from which the qESNA scale is derived. Table 1 presents the full ESNA interview and the qESNA scale.
Items of the ESNA interview and qESNA scale.
| ESNA interview | qESNA scale | Item content | Response format |
|---|---|---|---|
| 1 | Los médicos y las enfermeras me han explicado parte de lo que te ha pasado con la enfermedad, pero ¿me puedes decir tú cómo lo has vivido desde el inicio hasta ahora? ¿Qué te han ido explicando y cómo te has sentido?The doctors and nurses have told me some of what you have gone through with the disease, but can you tell me how you have experienced it from the beginning until now? What have they explained to you and how have you felt? | Open | |
| 2 | 1 | ¿Cómo lo estás llevando estas 2 últimas semanas?How have you been dealing with it these past 2 weeks? | Open |
| ¿Podrías situarlo en esta línea entre llevarlo muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 3 | 2 | ¿Cómo te encuentras físicamente?How do you feel physically? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 4 | 3 | Hasta ahora, ¿cómo crees que te están explicando lo que te pasa? ¿Quién te lo ha explicado?Until now, how have you been feeling about what they’ve explained to you about what is happening to you? Who has explained it to you? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 5 | ¿Te gustaría saber más sobre tu situación?Would you like to know more about your condition? | Yes/No/I don’t know | |
| ¿El qué?What? | Open | ||
| 6 | 4 | ¿Has explicado tú a alguien lo que te pasa?Have you told anyone what you’re going through? | Yes/No/I don’t know |
| ¿A quién? ¿Por qué?Whom? For what reason? | Open | ||
| ¿Podrías situar en esta línea cómo te hace sentir hablar de lo que te pasa entre muy mal y muy bien?Could you mark how you it makes you feel to talk about what you’re going through in this line from really poorly to really well? | Rating from 0−10 | ||
| 7 | 5 | ¿Cómo crees que te va a ir tu enfermedad más adelante?How do you think you’re going to handle your disease moving forward? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 8 | ¿Cómo se te pasó (hizo) el día de ayer?How did your day feel like yesterday? | Short/Long/Normal | |
| ¿Por qué?Why was it so? | Open | ||
| 9 | 6 | En los últimos días, ¿qué es lo que más te preocupa?In the past few days, what has been your main worry? | Open |
| ¿Podrías decir cuánto te preocupa entre nada y muchísimo?Could you tell me how much it worries you between ‘not at all’ and ‘a lot’? | Rating from 0−10 | ||
| ¿Hay algo más que te preocupe?Do you have any other concerns? | Open | ||
| 10 | 7 | ¿Cómo te has sentido al estar con tu familia con la que vives?How have you felt spending time with the family members you live with at home? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 11 | 8 | ¿Cómo te has sentido al estar/hablar con tu/tus mejor/es amigos/as?How have you felt spending time/talking to your best friend(s)? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| 12 | 9 | ¿Cómo crees que tu familia con la que vives (padre/madre/hermanos) está llevando esta situación?How do you think your family at home (father/mother/siblings) is feeling about this situation? | Open |
| ¿Podrías situarlo en esta línea entre muy mal y muy bien?Could you mark it in this line between really poorly and really well? | Rating from 0−10 | ||
| ¿Por qué piensas que se encuentran así?What makes you think they feel this way? | Open | ||
| 13 | 10 | ¿Podrías situar cuánta ALEGRÍA has tenido entre nada y muchísimo?Could you show me how JOY you have felt between ‘none’ and ‘a lot’? | Rating from 0−10 |
| ¿Qué es lo que te ha hecho sentir ALEGRÍA estas 2 semanas?What has made you feel JOY in the past 2 weeks? | Open | ||
| 14 | 11 | ¿Podrías situar cuánta RABIA has tenido entre nada y muchísimo?Could you show me how much ANGER you have felt between ‘none’ and ‘a lot’? | Rating from 0−10 |
| ¿Qué es lo que te ha hecho sentir RABIA estas 2 semanas?What has made you feel ANGER in the past 2 weeks? | Open | ||
| 15 | 12 | ¿Podrías situar cuánto MIEDO has tenido entre nada y muchísimo?Could you show me how much FEAR you have felt between ‘none’ and ‘a lot’? | Rating from 0−10 |
| ¿Qué es lo que te ha hecho sentir MIEDO estas 2 semanas?What has made you feel FEAR in the past 2 weeks? | Open | ||
| 16 | 13 | ¿Podrías situar cuánta TRISTEZA has tenido entre nada y muchísimo?Could you show me how much SADNESS you have felt between ‘none’ and ‘a lot’? | Rating from 0−10 |
| ¿Qué es lo que te ha hecho sentir TRISTEZA estas 2 semanas?What has made you feel SADNESS in the past 2 weeks? | Open | ||
| 17 | 14 | ¿Qué es lo que más te ayuda a estar bien o mejor?What helps you feel OK or better the most? | Open |
| ¿Podrías situarlo en esta línea entre nada y muchísimo?Could you mark it in this line between ‘not at all’ and ‘a lot’? | Rating from 0−10 | ||
| 18 | ¿Qué podemos nosotros hacer para que tú estés mejor?What can we do you make you feel better? | Open | |
| 19 | 15 | ¿Te gustaría que cambiase tu vida actual?Would you like your life to change from what it is like now? | Open |
| ¿Podrías situarlo en esta línea entre nada y muchísimo?Could you mark it in this line between ‘not at all’ and ‘a lot’? | Rating from 0−10 | ||
| 20 | Si tuvieras una varita mágica, ¿qué 3 deseos le pedirías?If you had a magic wand, what 3 wishes would you ask for? | Open | |
| Y con un deseo, ¿qué te gustaría que no cambiase en tu vida?And, if you had a wish, what would want NOT to change in your life? | Open | ||
| 21 | ¿Hay alguna cosa importante para ti que quieras comentar y que no hemos hablado?Is there something that is important to you that we have not discussed and you want to mention? | Open | |
| 22 | 16 | En general, ¿cómo valorarías tu calidad de vida (bienestar) en el momento actual?In general, how would you rate your quality of life (wellbeing) at this moment? | Rating from 0−10 |
The aim of our study was to analyse the psychometric properties of the qESNA scale in a Spanish population of children and adolescents in terms of construct validity, reliability and convergent validity.
MethodsParticipantsWe invited 100 children managed by the department of PPC of a tertiary care hospital between June 2021 and August 2023 participate in the study, and 58 of them (58%) responded. The flowchart of the assessed paediatric patients (Appendix A of the supplemental material) presents the reasons for not participating. The inclusion criteria were: (1) age >8 years; (2) fluency in Spanish;(3) having undergone an initial multidisciplinary assessment; (4) approval of participation by referring psychologist, and (5) informed consent/assent signed by legal guardians and patient. We excluded patients with moderate or severe neurological impairment or at risk of imminent death.
Measures- a)
Sociodemographic variables: we collected data on age, sex and nationality from the health records.
- b)
Disease-related variables: including the diagnosis, treatment withdrawal or withholding, clinical exacerbations, congenital disease and time elapsed from diagnosis. We collected this information from the health records and by asking specific questions from health professionals, who answered within a maximum of 3 days from the receipt of the child's response, thereby avoiding potential sources of bias.
- c)
Psychological variables through the following instruments:
- none-
Evaluation of Suffering in Children and Adolescents with Palliative Needs scale (qESNA): it comprises 16 items, all in visual analogue scale format, which the children completed on an electronic device through a digital platform (Aimentia Health), accompanied by the psychologist of the research team during the interview. The total score is obtained by adding the individual item scores for a maximum possible score of 160 points (range, 0–160). Five of the items are reverse-scored to control for response bias.
- none-
Emotion regulation: we used the emotion regulation (mood repair) subscale of the Spanish version of the Trait Meta-Mood Scale-24 (TMMS-24).13,14 It consists of 8 self-report items and it has been adapted and applied in children and adolescents,13 with a Cronbach α of 0.82. Items are rated on a 5-point Likert scale. In our study, we found an omega coefficient of 0.85.
- none-
Cognitive strategies for emotion regulation: we used a short version in Spanish of the Cognitive Emotion Regulation Questionnaire-Kids (CERQ-k).15,16 It comprises 18 items in 9 dimensions (self-blame, acceptance, rumination, positive refocusing, refocus on planning, positive reappraisal, catastrophizing, putting into perspective, and other-blame), each with 2 items rated on a 5-point Likert scale. Higher scores indicate greater use of regulation strategies. This self-report scale has been adapted for use in children and adolescents,15,17 with a Cronbach α of 0.80. In our study, we found an omega coefficient of 0.66.
- none-
Psychosocial functioning: the Strengths and Difficulties Questionnaire (SDQ)18 comprises a total of 25 items in 5 scales: emotional symptoms, conduct problems, hyperactivity problems, peer problems and prosocial behaviour. In every scale except for prosocial behaviour, higher scores indicate more severe problems, and the questionnaire achieved a Cronbach α of 0.73.19 In our study, we found an omega coefficient of 0.62.
- none-
Depression and anxiety symptoms: we used two questionnaires, each with 2 items, to screen for depression (Patient Health Questionnaire-2 [PHQ-2]) and for anxiety (Generalized Anxiety Disorder 2-item [GAD-2]),20 with answers given in a 4-point Likert scale (0–3) and a cut-off point of 3 (positive ≥3). The PHQ-2 (Cronbach α = 0.81) and GAD-2 (Cronbach α = 0.77) have been used previously in the paediatric population.21 In our study, we found an omega coefficient of 0.82.
- none-
Once the legal guardians and the patients had given informed consent, the psychologists of the department of PPC collected the data by interviewing the children, reviewing the health records and asking questions from the referring providers. We carried out a pilot study in 8 children (aged 8–18 years), which confirmed the feasibility of the use of these scales.
Statistical analysisWe used the software R, version 4.3.1, going through the following steps: (a) basic description of the data; (b) construct validity: exploratory factor analysis (EFA) with the Pearson correlation matrix, Bartlett test of sphericity and Kaiser-Meyer-Olkin (KMO) index, and confirmatory factor analysis (CFA). The goodness of fit was assessed by means of the χ2 test, comparative fit index (CFI), Tucker-Lewis index (TLI), standardised root mean square residual (SRMR) and root mean square error of approximation (RMSEA); (c) Reliability: Cronbach α, omega correlation coefficient, average variance extracted (AVE), composite reliability (CR) and test-retest correlation coefficient; (d) convergent validity with the Pearson correlation coefficient; and (e) analysis of specificity and sensitivity to determine the optimal cut-off point. We defined statistical significance as P < .05.
Ethical considerationsThe study was approved by the ethics committee of the hospital where it was conducted (file PIC-158-20 of 02/06/2020) and adhered to the principles of the Declaration of Helsinki. We informed parents and children about the study, the voluntary nature of participation and confidentiality; and participation in the study required signed informed consent.
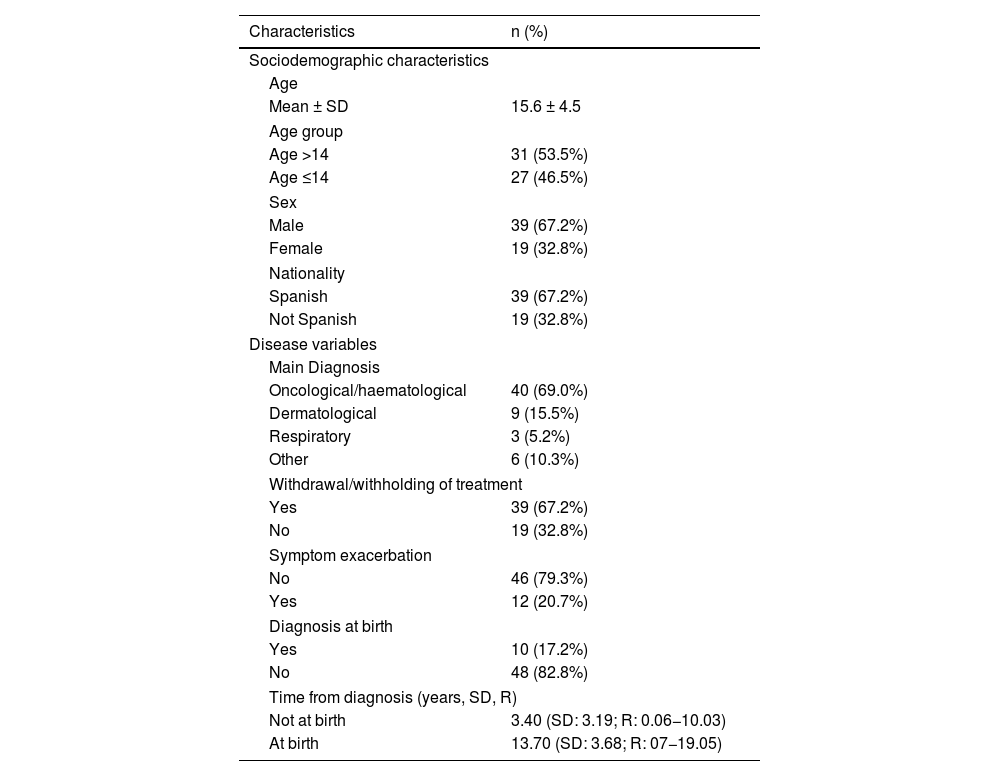
ResultsDescriptive analysis of the sampleThe qESNA scale was completed by 58 children, 19 (32.8%) female and 39 (67.2%) male, with a mean age of 15.6 years (standard deviation [SD], 4.50; range, 8.57–23.96), and 40 (69.0%) had oncological/haematological disease. Table 2 presents additional information on the characteristics of the sample.
Characteristics of the sample (N = 58).
| Characteristics | n (%) |
|---|---|
| Sociodemographic characteristics | |
| Age | |
| Mean ± SD | 15.6 ± 4.5 |
| Age group | |
| Age >14 | 31 (53.5%) |
| Age ≤14 | 27 (46.5%) |
| Sex | |
| Male | 39 (67.2%) |
| Female | 19 (32.8%) |
| Nationality | |
| Spanish | 39 (67.2%) |
| Not Spanish | 19 (32.8%) |
| Disease variables | |
| Main Diagnosis | |
| Oncological/haematological | 40 (69.0%) |
| Dermatological | 9 (15.5%) |
| Respiratory | 3 (5.2%) |
| Other | 6 (10.3%) |
| Withdrawal/withholding of treatment | |
| Yes | 39 (67.2%) |
| No | 19 (32.8%) |
| Symptom exacerbation | |
| No | 46 (79.3%) |
| Yes | 12 (20.7%) |
| Diagnosis at birth | |
| Yes | 10 (17.2%) |
| No | 48 (82.8%) |
| Time from diagnosis (years, SD, R) | |
| Not at birth | 3.40 (SD: 3.19; R: 0.06−10.03) |
| At birth | 13.70 (SD: 3.68; R: 07−19.05) |
SD, standard deviation.
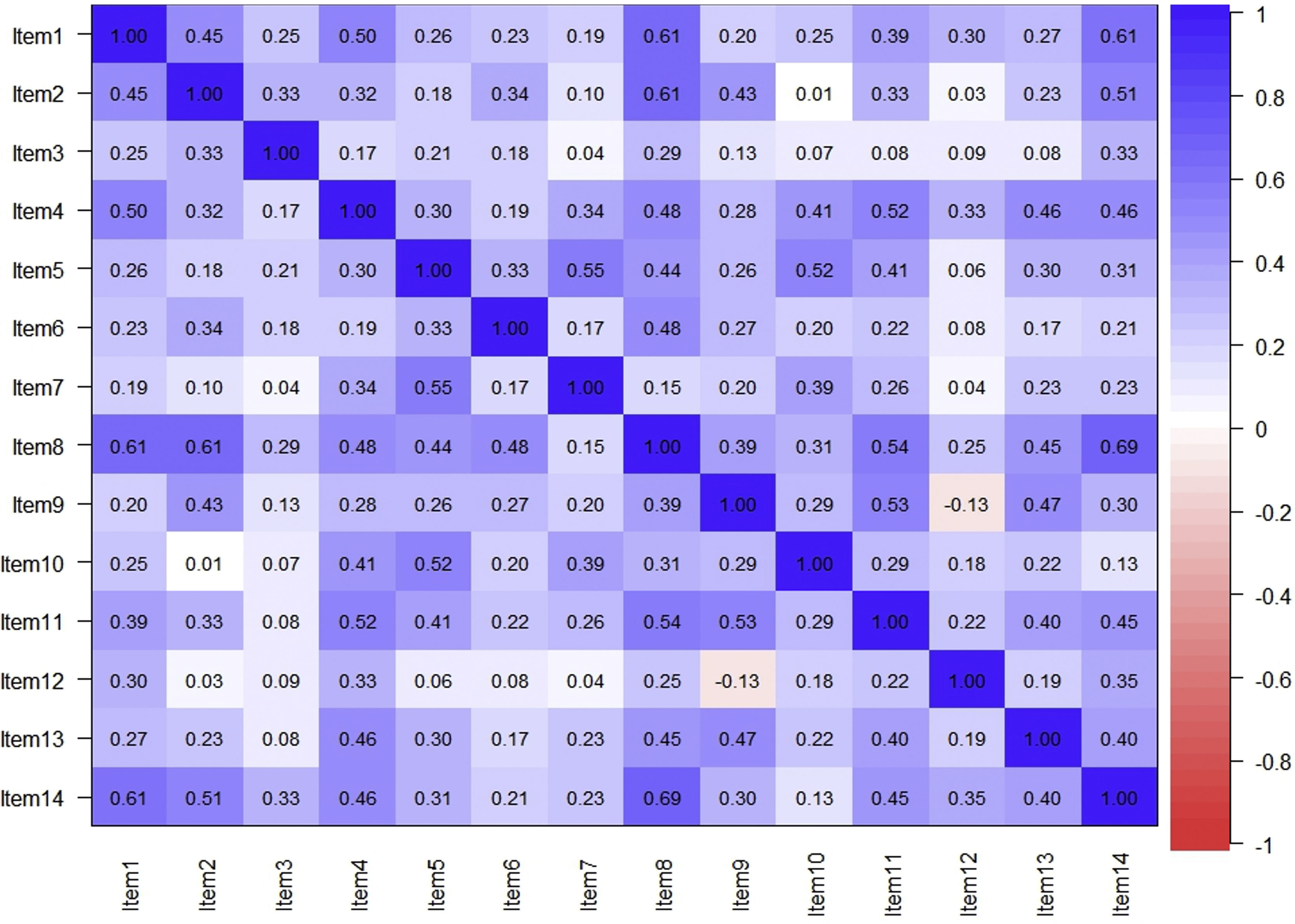
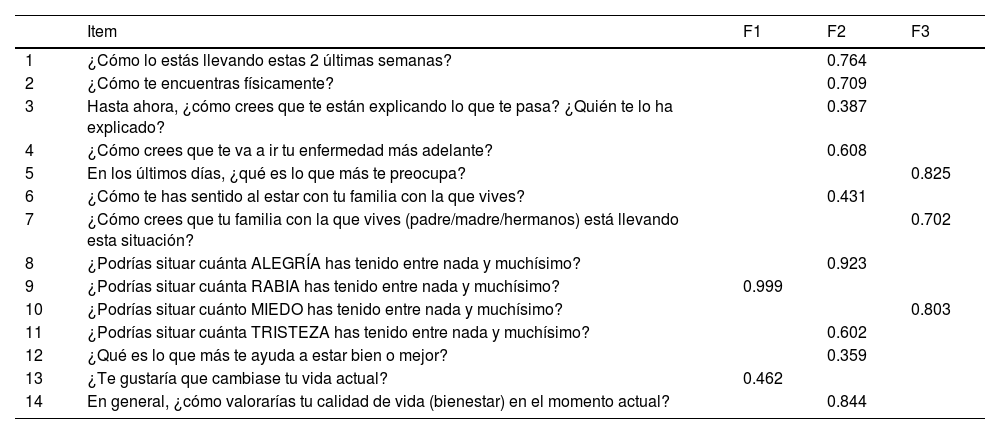
Item 4 did not meet the criterion of a KMO greater than 0.5 (KMO = 0.47), and was consequently eliminated from the scale. After analysing the factor loading matrices and the corresponding graph, we found that item 11, with a factor loading of less than 0.3, was not associated with any of the common factors, so it was also eliminated. With the 14 remaining items, we carried out the Bartlett test again (Bartlett = 305.266; P < .001) and the KMO index, and found that all values were greater than 0.5.
We performed the EFA and, using the parallel analysis scree plots (Appendix A, Supplemental Material, Parallel Analysis Scree Plots Figure), we found 3 eigenvalues above the thresholds proposed by Horn,22 so we propose a structure consisting of one eigenvector and 3 factors.
Fig. 1 presents the linear correlation matrix for the 11 items remaining in the new version of the qESNA scale.
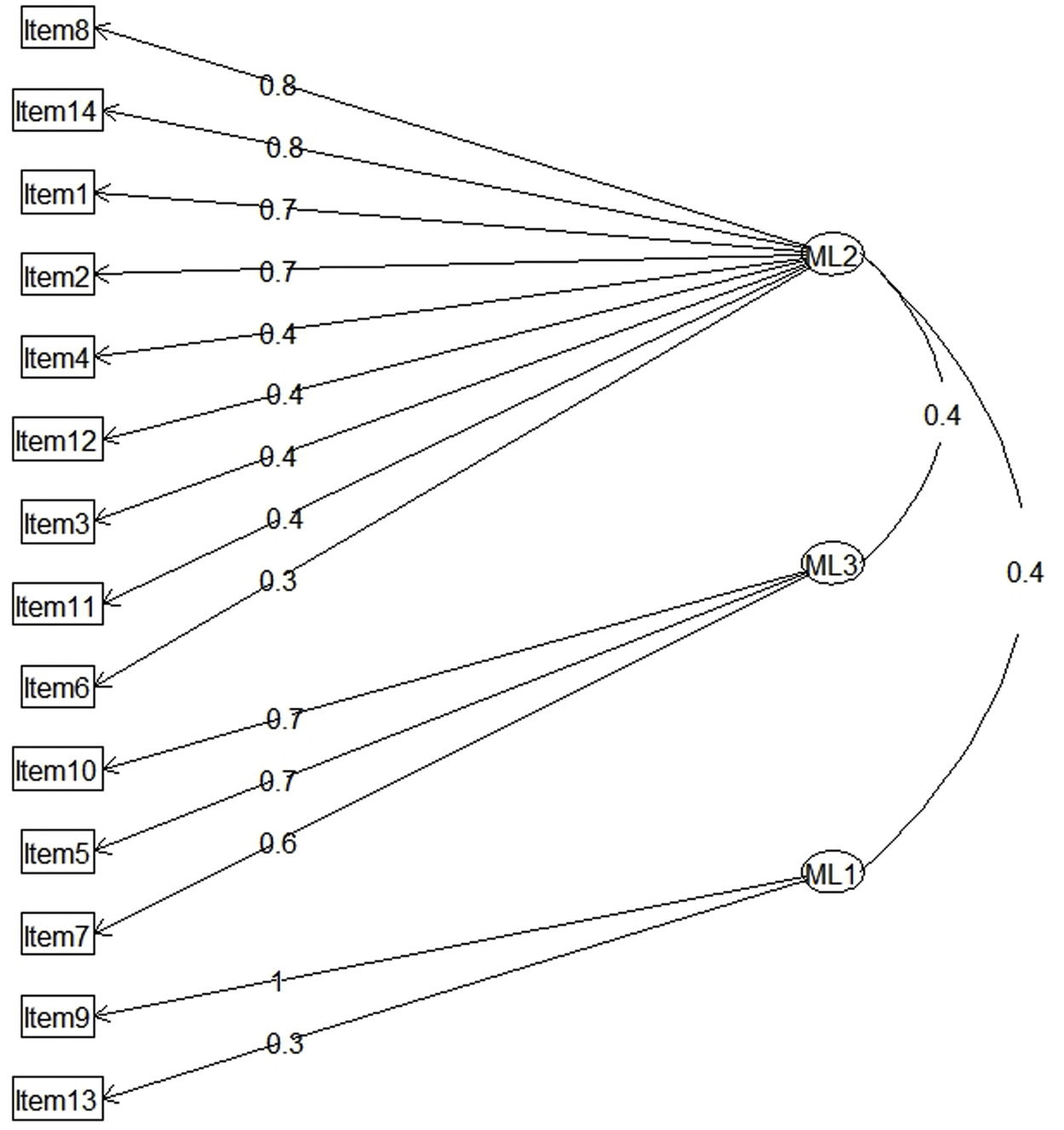
Confirmatory factor analysisOne scale with 14 items and 3 factors (qESNA) exhibited a good fit for the data (CFI = 0.93; TLI = 0.91 and RMSEA = 0.07). Fig. 2 presents the standardised loadings for the scale.
Together, these 3 factors explained 45% of the variance: the first factor explained 10% of the variance, encompassed items 9 and 13 and was labelled “Frustration and wish for change”; the second factor, labelled “Overall wellbeing”, explained 23% of the variance and encompassed items 1–4, 6, 8, 11 and 12; and the third one, labelled “Worry”, explained 12% of the variance and encompassed items 5, 7 and 10. The SS loadings for each factor were greater than 1 (factor 1: 1.49; factor 2: 1.86; factor 3: 3.38). Table 3 presents the factor loadings for the estimated model.
Factor loadings of the items.
| Item | F1 | F2 | F3 | |
|---|---|---|---|---|
| 1 | ¿Cómo lo estás llevando estas 2 últimas semanas? | 0.764 | ||
| 2 | ¿Cómo te encuentras físicamente? | 0.709 | ||
| 3 | Hasta ahora, ¿cómo crees que te están explicando lo que te pasa? ¿Quién te lo ha explicado? | 0.387 | ||
| 4 | ¿Cómo crees que te va a ir tu enfermedad más adelante? | 0.608 | ||
| 5 | En los últimos días, ¿qué es lo que más te preocupa? | 0.825 | ||
| 6 | ¿Cómo te has sentido al estar con tu familia con la que vives? | 0.431 | ||
| 7 | ¿Cómo crees que tu familia con la que vives (padre/madre/hermanos) está llevando esta situación? | 0.702 | ||
| 8 | ¿Podrías situar cuánta ALEGRÍA has tenido entre nada y muchísimo? | 0.923 | ||
| 9 | ¿Podrías situar cuánta RABIA has tenido entre nada y muchísimo? | 0.999 | ||
| 10 | ¿Podrías situar cuánto MIEDO has tenido entre nada y muchísimo? | 0.803 | ||
| 11 | ¿Podrías situar cuánta TRISTEZA has tenido entre nada y muchísimo? | 0.602 | ||
| 12 | ¿Qué es lo que más te ayuda a estar bien o mejor? | 0.359 | ||
| 13 | ¿Te gustaría que cambiase tu vida actual? | 0.462 | ||
| 14 | En general, ¿cómo valorarías tu calidad de vida (bienestar) en el momento actual? | 0.844 |
P < 0.01.
We assessed internal consistency with the Cronbach α (0.85; 95% CI, 0.80−0.91), Guttman’s lambda-6 (0.90) and the omega coefficient (0.89), which were indicative of a high internal consistency. The Cronbach α values for individual items ranged from 0.83 to 0.86. The AVE values were less than 0.5 (0.126; 0.269; 0.479). The CR values (0.223; 0.741; 0.726) were greater than 0.7 for subscales 2 and 3. Following the criterion proposed by Fornell and Larcker,23 the latter result indicates that the validity of the scale is still acceptable, even if the explained variance is small.
We assessed temporal stability using data for 7 (12.1%) of the 58 children, with an average of 39.6 days elapsed between the two tests. The intraclass correlation coefficient was 0.66, indicative of an adequate stability.
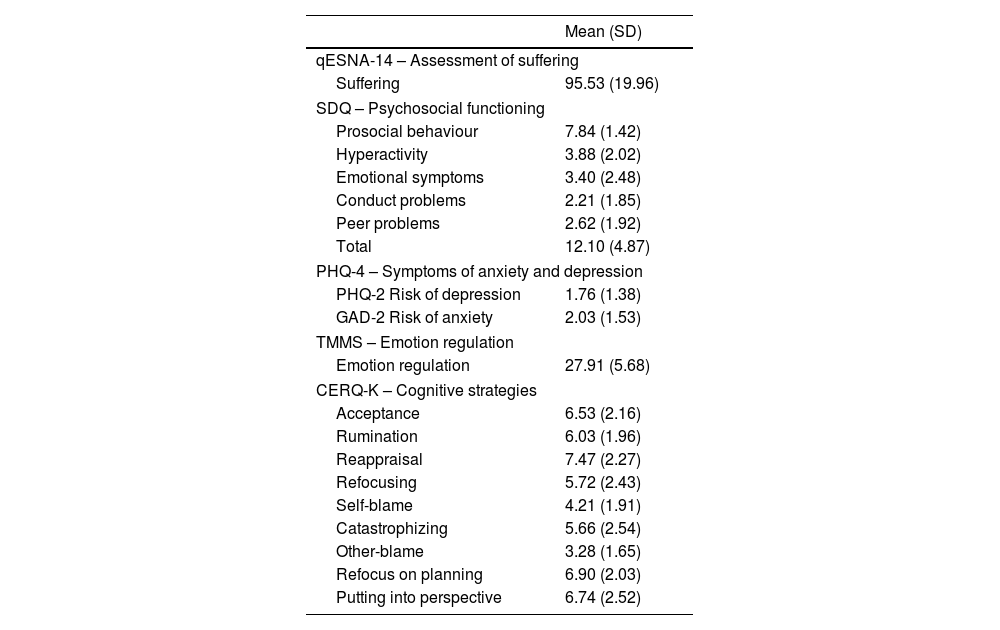
Convergent validityThe mean suffering score in the sample was 95.53 (SD, 19.96; range, 50.00–134.00), with a median of 97.00. Very few patients expressed discomfort (5.17%); 77.59% stated they did not find the interview long, and 79.31% stated that they believed it could help other children like them. Table 4 presents the results of the descriptive analysis of the psychological variables under study.
Descriptive analysis of psychological variables.
| Mean (SD) | |
|---|---|
| qESNA-14 – Assessment of suffering | |
| Suffering | 95.53 (19.96) |
| SDQ – Psychosocial functioning | |
| Prosocial behaviour | 7.84 (1.42) |
| Hyperactivity | 3.88 (2.02) |
| Emotional symptoms | 3.40 (2.48) |
| Conduct problems | 2.21 (1.85) |
| Peer problems | 2.62 (1.92) |
| Total | 12.10 (4.87) |
| PHQ-4 – Symptoms of anxiety and depression | |
| PHQ-2 Risk of depression | 1.76 (1.38) |
| GAD-2 Risk of anxiety | 2.03 (1.53) |
| TMMS – Emotion regulation | |
| Emotion regulation | 27.91 (5.68) |
| CERQ-K – Cognitive strategies | |
| Acceptance | 6.53 (2.16) |
| Rumination | 6.03 (1.96) |
| Reappraisal | 7.47 (2.27) |
| Refocusing | 5.72 (2.43) |
| Self-blame | 4.21 (1.91) |
| Catastrophizing | 5.66 (2.54) |
| Other-blame | 3.28 (1.65) |
| Refocus on planning | 6.90 (2.03) |
| Putting into perspective | 6.74 (2.52) |
SD, standard deviation.
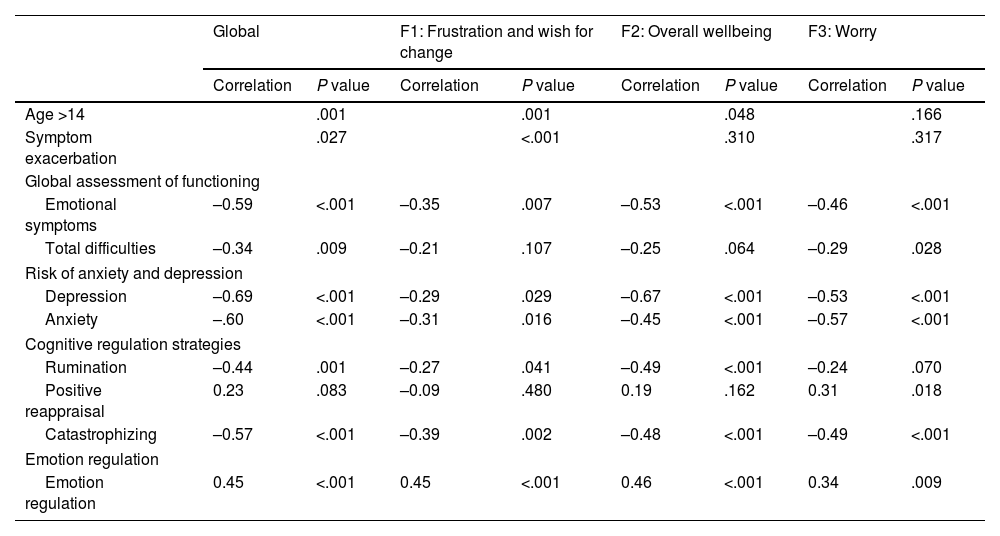
Table 5 shows the significant Pearson correlation coefficients for the association between the total score and the different factors of the qESNA with the other variables under study. We found strong correlations (>0.60) between the total score and the risk of anxiety (−0.60) and of depression (–0,69) and between factor 2—overall wellbeing—and the risk of depression (−0.67).
Significant correlations for the qESNA scale.
| Global | F1: Frustration and wish for change | F2: Overall wellbeing | F3: Worry | |||||
|---|---|---|---|---|---|---|---|---|
| Correlation | P value | Correlation | P value | Correlation | P value | Correlation | P value | |
| Age >14 | .001 | .001 | .048 | .166 | ||||
| Symptom exacerbation | .027 | <.001 | .310 | .317 | ||||
| Global assessment of functioning | ||||||||
| Emotional symptoms | –0.59 | <.001 | –0.35 | .007 | –0.53 | <.001 | –0.46 | <.001 |
| Total difficulties | –0.34 | .009 | –0.21 | .107 | –0.25 | .064 | –0.29 | .028 |
| Risk of anxiety and depression | ||||||||
| Depression | –0.69 | <.001 | –0.29 | .029 | –0.67 | <.001 | –0.53 | <.001 |
| Anxiety | –.60 | <.001 | –0.31 | .016 | –0.45 | <.001 | –0.57 | <.001 |
| Cognitive regulation strategies | ||||||||
| Rumination | –0.44 | .001 | –0.27 | .041 | –0.49 | <.001 | –0.24 | .070 |
| Positive reappraisal | 0.23 | .083 | –0.09 | .480 | 0.19 | .162 | 0.31 | .018 |
| Catastrophizing | –0.57 | <.001 | –0.39 | .002 | –0.48 | <.001 | –0.49 | <.001 |
| Emotion regulation | ||||||||
| Emotion regulation | 0.45 | <.001 | 0.45 | <.001 | 0.46 | <.001 | 0.34 | .009 |
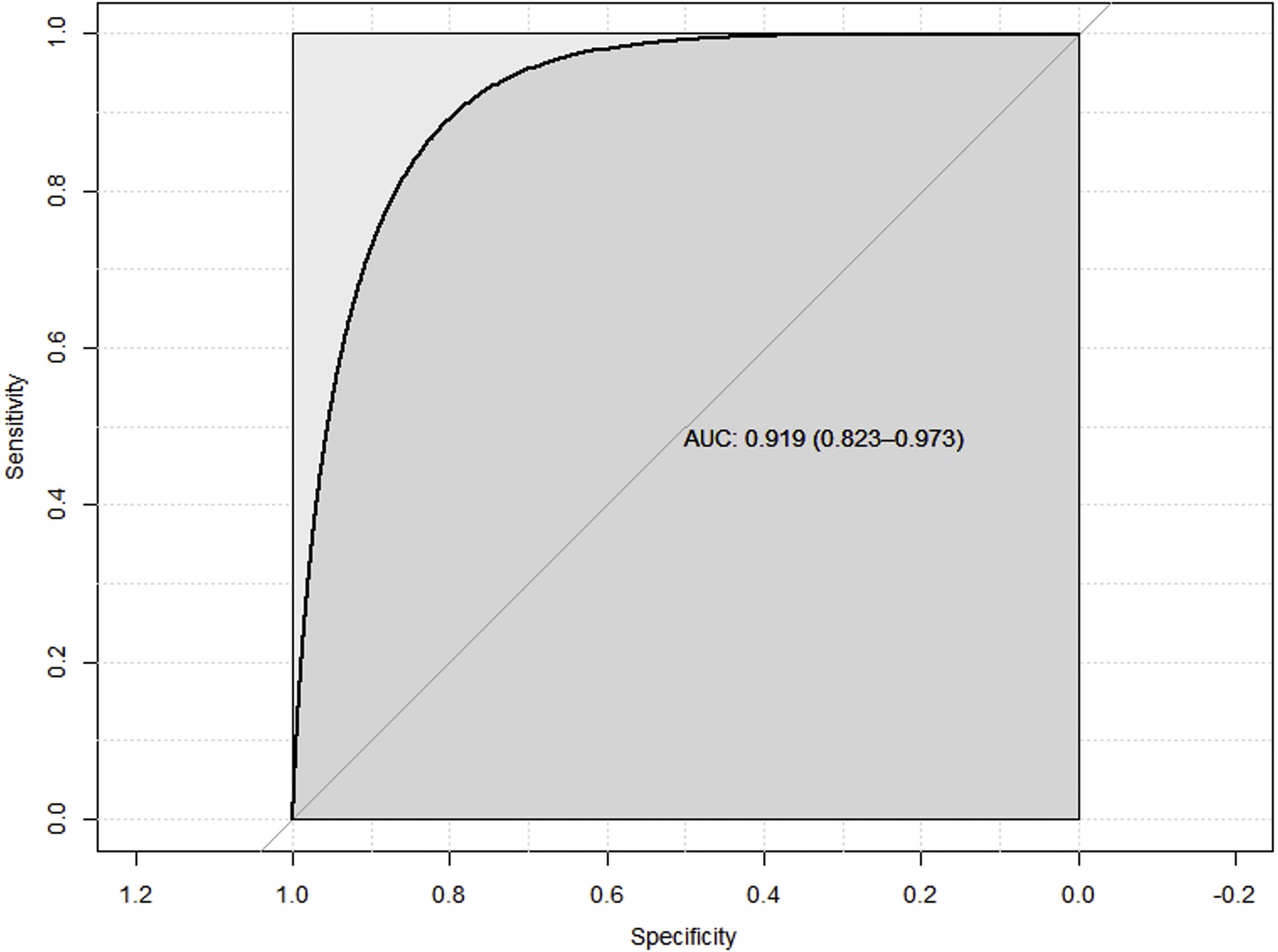
Based on the existing literature,12 we created a criterion variable for the assessment of suffering that was a composite of 3 criteria1: presence of emotional or peer problems based on the SDQ scale2; risk of anxiety or depression based on the PHQ-43; scoring above the mean in the use of the rumination and catastrophizing cognitive regulation strategies (>12). Fig. 3 shows the ROC curve obtained in the analysis, with an area under the curve of 0.914 (P < 0.001) and a 95% CI of 0.810−0.971. This proved the predictive/diagnostic capacity of the qESNA, and we established a cut-off point of 81, which was the value that offered the best possible combination of sensitivity (83.33%) and specificity (93,48%) values. A score of less than 81 would be indicative of suffering in children with a significant impact on the emotional, interpersonal and psychological domains. The total score can range from 0 to 140. Based on the establish cutoff, 13 children (22.41%) had suffering.
DiscussionThe aim of this study was to analyse the psychometric properties of the qESNA scale in the context of the ESNA interview.12 The results yielded a version of the qESNA composed of 14 items with a global scale score and 3 dimensions (‘frustration and wish for change’, ‘overall wellbeing’ and ‘worry’) that exhibited a high internal consistency, sensitivity and specificity, in which a score of less than 81 differentiates children with greater suffering. It also showed good convergent validity in relation to emotional symptoms and global functioning assessed with the SDQ, emotion regulation assessed with the TMMS, the risk of anxiety and depression assessed with the PHQ-4, and the use of the cognitive strategies of rumination and catastrophizing assessed with the CERQ-K.
The results of the EFA reduced the scale to 14 items, revealing issues with 2 items. One explanation may be that children found it difficult to identify their own emotions in connection to their own actions with or involving other individuals.24
The CFA corroborated the 14-item, 3-factor model of the qESNA scale, a multidimensional structure that was consistent with the previous literature,25,26 which demonstrates that suffering is a multifactorial experience. The qESNA includes items that address coping strategies, the impact of symptoms, information management, parent/child relations, the impact on the family, the main concerns, the emotional impact, peers relations and spiritual aspects such as hope, meaning and sources of strength; in line with the relevant aspects described in the literature.24 Although there are validated scales27 used in the PPC setting to assess quality of life, such as the PedsQL,28 the KIDSCREEN-27,29 the KINDL30 or the CPOS,9,26 the proposed interview format, including open- and closed-ended questions and a scale such as the qESNA, allows a deeper exploration of the children's discourse and narrative, giving room for their concerns and difficulties to be expressed, in addition to yielding scores that can aid the assessment of suffering.
The convergent validity analysis found a strong correlation with the risk of depression and anxiety, which was consistent with other studies.5 The cognitive strategies of rumination and catastrophizing were also associated with a greater degree of suffering, as evinced by other studies that found an association with depressive symptoms.17 Emotional problems and difficulty regulating emotion were also associated with a greater degree of suffering in the qESNA scale. Higher levels of emotion regulation are associated with better mental health.31 Adolescents aged more than 14 years exhibited greater suffering based on the qESNA score, results similar to those observed in adolescents and young adults with palliative care needs who were found to have a poorer quality of life compared to younger children.32 This could reflect the greater cognitive capacity of adolescents for logical and abstract thought, and a better understanding of the disease,33 as children aged 7–11 years tend to use their reasoning skills more successfully with concrete information rather than abstract concepts,34 which can have an impact on assessment results. Other important aspects highlighted in the literature35 are the need to make interviews short and the preference for digital assessment tools that are also developmentally appropriate, all conditions met by the qESNA scale. Still, further research is needed to determine what is appropriate based on the child’s stage of development.9
The assessment detected suffering in 23% of the children, which indicates the need to prioritise delivering their care needs. We found adequate internal consistency values for all 3 factors. Factor 1, “frustration and wish for change”, includes the emotion of anger and the wish to change, so we considered it was associated with the change or loss of what they consider normal, which has already been found to be a source of considerable suffering.12,36 This was the only factor that was positively correlated to symptom exacerbation, which led us to believe that this is the factor that evinces the impact of symptoms most strongly, as corroborated in previous studies.33,37 Factor 2, “overall wellbeing”, offers a broader perspective of the sources of suffering. It correlates to the severity of emotional symptoms, depression, anxiety, rumination and catastrophizing. Factor 3, “worry”, collects information on the chief concern, the patient’s perception of parental wellbeing and the emotion of fear. Children with severe disease describe their families as their main source of support and are aware that their suffering has an impact on the family’s suffering and vice versa.38
In conclusion, the qESNA scale has good psychometric properties, is reliable, easy to administer and provides a total suffering score, as well as scores for the factors that contribute to it.
Limitations and strengthsThere are some limitations in this study in relation to the interpretation and generalisability of the results. One of the main limitations of the study is that the sample size was smaller than recommended for an adequate psychometric analysis. The hypothesised factor pattern was confirmed by the analysis of the errors of the model; however, these errors encompassed a substantial portion of the variance that was not explained by the factors, and therefore the reliability analysis of the subscales did not fulfil all the criteria to corroborate the reliability of the 3 factors. Another limitation is the wide age range of the sample under study, a factor that may have affected participants’ ability to understand and respond based on their stage of development. On the other hand, the internal consistency of the used scales was acceptable, with the exception of the scale assessing strengths and skills. (SDQ). In any case, we consider the study has also strengths, including achieving a large sample from the population of interest and the fact that the scale has good psychometric properties, is easy to administer and has a multifactorial structure fitting the multidimensional perspective of suffering. The research team believes it is an advance in the field and a starting point for further research. New studies in larger samples should be conducted to corroborate these findings and making a more detailed analysis.
ConclusionTo be able to differentiate between an adaptive and a maladaptive response and assess the degree of suffering to prioritise and guide the psychological support required by children with life-threatening or limiting diseases, simple, reliable and feasible instruments need to be available in the clinical care setting. Although further research is required to confirm our results, our study demonstrates that the qESNA is a simple and easy to use tool for the assessment of suffering in children and adolescents with palliative care needs and serves as an initial step to guide the planning and delivery of appropriate and personalised psychological and/or multidisciplinary care, while also allowing longitudinal monitoring of suffering in these children during the follow-up.
FundingThis research did not receive any external funding.
AuthorshipDTP participated in conceiving and designing the study, developed the data collection tools, collected data and drafted and reviewed the manuscript.
JL and ECR participated in conceiving and designing the study, coordinated and supervised data collection and participated in the critical review of the intellectual contents of the manuscript and its editing.
SNV participated in the critical review of the intellectual contents of the manuscript and contributed to its drafting and editing.
CB and MG analysed the results and contributed to the drafting and editing of the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to express our gratitude to all the children and parents who participated in the study and therefore contributed to improving the assessment of children with complex chronic diseases and life-limiting and life-threatening conditions. We would also like to thank the members of the Department of Paediatric Palliative Care and Chronic Complex Disease of our hospital. We would also like to thank the ANJANA Working Group of the Sociedad Catalana-Balear de Cuidados Paliativos (Catalan-Balearic Society of Palliative Care) and the Sociedad Catalana de Pediatría (Catalan Society of Paediatrics) for their support and for including this study among their research priorities toward the improvement of end-of-life care.